Oral cancer is generally preceded by some potentially malignant lesions and conditions potentially malignant disorders for a varying length of time. They share the same etiological factors with oral cancer, particularly the use of tobacco and areca nut exhibit the same site eg:buccal mucosa since the buccal mucosa has larger surface area and the toxins leached from the arecanut and tobacco products contact them for longer period than any other area in the oral mucosa.and habit relationship [1].
Individuals with oral precancer such as oral leukoplakia and oral submucous fibrosis run a risk that is 69 times higher for them to develop oral cancer compared to tobacco users who do not have pre cancer. The recognition and management of potentiallly malignant disorders therefore constitutes a vital oral cancer control measure [2].
Epidemiological studies indicate that intervention at an early stage might reduce oral carcinoma related morbidity and mortality. This includes detection of oral cancer at its precancerous stage. The discovery of immunological markers at blood level, histological and molecular level has revolutionized the diagnosis and prognosis in oral precancerous and cancer lesions [3].
Immune complexes are clusters of interlocking antigens and antibodies. Under normal conditions immune complexes are rapidly removed from the bloodstream by macrophages in the spleen and Kupffer cells in the liver. In some circumstances, however, immune complexes continue to circulate [4].
Immune complexes may themselves cause disease when they are deposited in organs,such as in certain forms of vasculitis. This is the third form of hypersensitivity in the Gell-Coombs classification, called Type III hypersensitivity [5].
Immune complex deposition is a prominent feature of several autoimmune diseases, including systemic lupus erythematosus, cryoglobulinemia, rheumatoid arthritis, scleroderma and Sjögren’s syndrome.
Circulating immune complex disease occurs when the host’s antibody production, relative to the amount of antigens, is inadequate for prompt elimination of antigen. Normally, excess amounts of antibody are formed which generate large immune complexes that are removed very rapidly from the circulation and are disposed of by the mononuclear phagocytic system. If the antibody response is very poor, only a few very small complexes are formed and are prone for vascular deposition [5].
The occurrence of Circulating Immune Complexes (CIC) as a marker for tumor burden and prognosis in the sera of patients with oral precancer and cancer is now well established [6].
Recent advances in the fields of Circulating Immune Complexes, tumor progression, drug resistance, tumor cell heterogeneity and metastasis have resulted in a renewed interest in the development of non- specific immunotherapeutic modalities.
The overall consensus is that only a small percentage of the detected CIC in vivo represent tumor associated antigens complexed with antibodies. The bulk of CIC most likely represent auto antibodies or the reaction to denatured self proteins, microbes, normal lymphocyte, antigens and nuclear antigens. Antigenic make up of CIC in cancer patients reflects the host’s immune response to a variety of often overlapping antigenic stimuli and hence paves way for further studies [7].
This study was conducted to understand the role of these CICs in the oral potentially malignant disorders like oral leukoplakia and OSMF. It can be suggested that immunological assessment of markers such as CIC in oral precancer patients may help in earlier diagnosis and prognosis of these lesions/conditions. Since ,CIC levels in Serum helps in predicting malignant potential of the pre malignant disorders it can be used as a reliable biomarkers [7].
Materials and Methods
This study was conducted in the Department of Ragas Dental college and Hospital, Outpatient Department, Uthandi, Chennai, Tamilnadu, India. The age of the subjects included in the study ranges between 20-60 years. 25 patients with oral leukoplakia, 25 patients with Oral submucous fibrosis. Since the habit of arecanut chewing and tobacco chewing starts usually at early adolescence the age group is selected from 20 years and considering the incidence of previous studies conducted in India [3,8] it is restricted between 20-60 years. and sex matched healthy controls formed the study group. Subjects with positive history of smoking tobacco, chewing arecanut, it is only arecanut not mixed with any other tobacco products. Positive clinical features suggestive of Oral leukoplakiaall types of leukoplakia are taken in to account to see the correlation between the types on the basis of CIC. and Oral submucous fibrosis were selected. For Normal controls, subjects with no oral mucosal lesions were selected. Normal controls are checked for other red and white lesions.
Lesions belonging to other entities such as Lichen planu, lupuserythematosus,leukedema and white sponge nevus and lesions for which etiology can be established, such as frictional keratosis, cheek/lip/tongue biting, contact lesions and stomatisnicotinapalatini.
Subjects with major systemic ailments with cardiovascular, respiratory diseases were excluded.
Subjects with any form of immunosupression and with autoimmune disorders were excluded
Subjects with history of corticosteroid therapy were excluded.
For Oral submucous fibrosis clinical diagnosis was made with the aid of clinical grading given by Gupta PC and Dinesh Chandra in 1992 [8].
GROUP-I: Leukoplakia; GROUP-II: Oral submucous fibrosis; GROUP-III: Normal controls.
Permission from the ethical committee of Ragas Dental College and Hospital, Chennai was obtained before starting the study for interpretation and examining the subjects and for drawing 5ml of blood.
Also an informed consent was obtained from the subjects forming the study sample, both in English and Tamil to participate in the study and to undergo blood investigation in the course of study.
Modified Poly Ethylene Glycol-6000(PEG) Mediated Precipitation technique was used to estimate the levels of Circulating Immune Complex (CIC) in serumby using the Reagents,0.01M Borate buffer,with PH–8.4 and 4.166% Poly Ethylene Glycol (PEG). After incubation at room temperature for 60 minutes, the turbidity developed will be measured spectrophotometrically 450nm against control containing 1:30 diluted serum in Borate buffer without PEG. The level of CIC in serum will be expressed in terms of OD-450 (OD- Optical Density) measured at the end of 60 minutes [3].
The readings are done with digital spectrometer and it is a single blind study. All the datas were entered in Microsoft excel sheets. Statistical analysis was done using SPSS software SYSTAT version 7.0.
Mean and standard deviation were estimated in the sample for each study group. Mean values were compared by using one-way ANOVA followed by multiple range tests by Tukey-HSD procedure.
In the above test ‘P’ value of less than 0.05 is accepted as statistically significant.
Results
[Table/Fig-1] shows the retro commissure area to be the highest % of area to get affected, followed by buccal mucosa, floor of the mouth and tongue to be the last area.
Distribution of Subjects in Group-I According to the Site of Leukoplakia
| Sl.no | Site of leukoplakia | No.of subjects | Percentage |
|---|
| 1. | Retro commissure | 14 | 56 % |
| 2. | Buccal mucosa | 9 | 36% |
| 3. | Floor of the mouth | 1 | 4% |
| 4. | Tongue | 1 | 4% |
| Total | 25 | 100% |
[Table/Fig-2] shows homogeneous leukoplakia is the most common type to affect,followed by speckled, Verrucous and ulcerative types.
Distribution of Subjects in Group-I According to the Type of Leukoplakia
| Sl no | Type | No. of subjects | Percentage |
|---|
| 1. | Homogeneous leukoplakia | 19 | 76% |
| 2. | Speckled leukoplakia | 05 | 20%0 |
| 3. | Verrucousleukoplakia | 1 | 4% |
| 4. | Ulcerativeleukoplakia | 0 | 0 |
| | Total | 100% |
For Oral submucous fibrosis clinical diagnosis was made with the aid of clinical grading given by Gupta PC and Dinesh Chandra in 1992 [8].
[Table/Fig-3] shows clinical Grade –III is the highest of all grades encountered followed by Grade-IV and Grade-I.
Distribution Of Subjects In Group Ii (Osmf) According To Clinical Grade.
| Sl.no | Clinical Grade | No. of Subjects | Percentage |
|---|
| 1. | I | 2 | 8% |
| 2. | II | 0 | 0 |
| 3. | III | 20 | 80% |
| 4. | IV | 3 | 12% |
| Total | 25 | 100% |
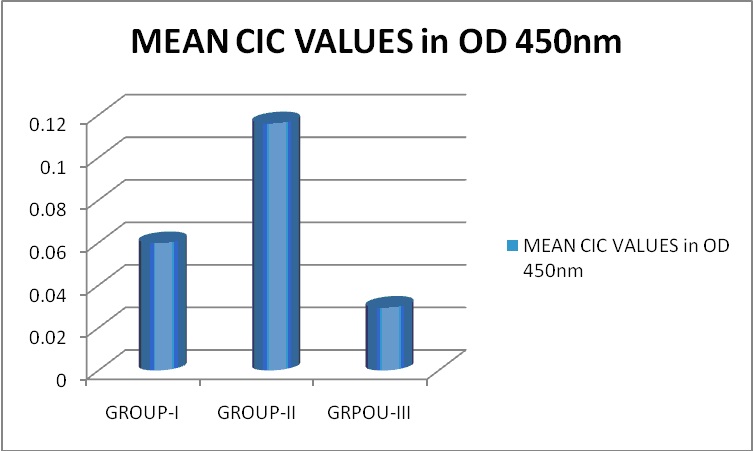
[Table/Fig-4] shows CIC values to be highest in Group-II Oral sub mucous fibrosis, followed by Group-I Oral leukoplakia, then Group-III the Normal subjects.
Mean CIC Values In Relation to Group-I, Group-II and Group-III Group-I: Leukoplakia, Group-II: Oral Sub Mucous Fibrosis, Group-III: Normal Controls
Discussion
Oral cancer is prevalent in most areas where tobacco related practices are observed. For development of oral cancer, tobacco is the single it comes as prime risk factor of all the reasons for oral cancergreatest risk factor. When this is combined with arecanut the risk increases many fold.
Ignorance of early symptoms together with lack of proper diagnostic and treatment facilities at the gross root level lead to presentation of patients to cancer hospitals in advanced disease status [9].
The immunological abnormalities in patients with cancer in the head and neck appear to be more profound than those associated with cancers of the bronchus, breast, cervix, colon or bladder [10].
The CIC play a specific role as initiators of mechanism of tissue injury in many infections, autoimmune disorders, and neoplastic diseases. A strong correlation exists between CIC level and progression to cancer [11].
In the present study, Oral leukoplakia group had maximum number of cases in the age group of 41-50years, with [Table/Fig-5] 12 subjects (44%),that is in the fifth decade of life,and is consistent with the studies done by Rajenderan R et al., 2006 [7,12].
Showing Age Wise Distribution of Subjects Group-I: Leukoplakia, Group-II: Oral Sub Mucous Fibrosis, Group-III: Normal Controls In our study it has been interpreted as above mentioned.
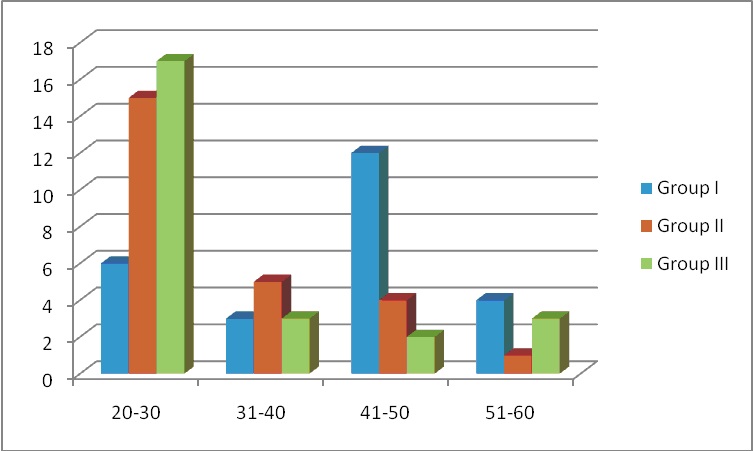
In Oral sub mucous fibrosis group the prevalence of age group is much more younger than oral leukoplakia age group. That is 15 (60%) [Table/Fig-5] subjects lie between the age group of 20-30 years which is consistent with the study done by Babu S, in 1996 (58%) [13].
In a study done by Gupta PC in 1998 [9] arecanut usage was concentrated in the lower age group less than 35 years. They found upto 85% cases were below 35 years, which is also in consistent with our study [14].
In the present study oral leukoplakia was completely seen in males only, with 25 subjects (100%) which is exactly matching with the study done by Hogewind WFC and Van Der I in 1989 (100%) [15].
In the present study 24 males (96%) and 1 female (4%) were clinically diagnosed having oral submucousfibrosis,which is in accordance with the study of Dayal PK in 1998 (89% -M; 11%-F) [16].
In the present study in Oral leukoplakia group 25 subjects (100%) were found with the habit of smoking tobacco. Other habits such as chewing arecanut, alcohol consumption also seen in this group. However the predominant form of the habit is smoking tobacco which is in consistent with the study of Holmstrup P et al., in 2006 [17] in which they found that 73% of leukoplakia being associated with tobacco habit, the value in the present study is slightly higher than what they reported.
In the Oral sub mucous fibrosis group areca nut chewing habit predominated 25 subjects (100%) and can be predicted as the only etiological factors associated with OSMF. The subjects also had habits of smoking and alcohol consumption but to varying degree. This is in accordance with the study done by Maher et al., in 1994 [18] where they found 98% of subjects were with the habit of chewing areca nut who suffered from OSMF.
By comparing Oral leukoplakic group, Oral submucous fibrosis group and the control group with the habit as smoking, chewing and alcohol consumption by using one way ANOVA it was found that there exists significant correlation among the groups in relation to habits with p value 0.035.
Distribution of subjects with habit of smoking in oral leukoplakia, oralsubmucous fibrosis and control groups revealed that there exists significant correlation among the groups with respect to smoking frequency with p value 0.0002 and smoking duration with p-value 0.003.
In subjects with predominantly smoked form of tobacco habit,14 subjects (56%) had lesions in the retero commissural area,followed by 9 subjects (36%) had lesions in buccal mucosa,1subject (4%) had lesion in the floor of the mouth and I subject had lesion in the tongue (4%) which is consistent with the study conducted by Reichart PA and Kohn H in 1996 [19], in which they found the reterocommisure was the most commonly affected site upto 43.35% followed by 36.7% in buccal mucosa.
In the present study it was found that most of the cases were of homogeneous leukoplakia with 19 subjects (76%),followed by speckled leukoplakia with 5 subjects (20%) and Verrucousleukoplakia in 1 subject (4%). No ulcereativeleukoplakia was seen in our study. This study is in accordance with the study conducted by Reichart PA and Kohn H in 1996 [19] where homogeneous type to be more (84.2%) than nonhomogeneous type (15.8%).
In the present study out of 7 cases 4 homogemous and 3 non homogenous leukoplakia showed high CIC values which is above Optical Density 450 nm –0.08 deviates greatly from the mean value from the Group I leukoplakia which is 0.05988 [Table/Fig-6], this may be attributed to the fact that these lesions carries a high relative risk for malignant transformation, which is in accordance with the study done by Cynthia Jane in 2007 [3] (p< 0.002).
Mean, Standard Deviation, Test of Significance of CIC in Relation to Group-I, Group-II and Group-III
| Group | No. of subjects | Mean CIC values in OD 450nm | Standard deviation | Minimum CIC value in OD 450 nm | Maximum CIC value in OD 450 nm |
|---|
| GROUP-I | 25 | 0.05988 | 0.024761 | 0.014 | 0.089 |
| GROUP-II | 25 | 0.11620 | 0.046957 | 0.048 | 0.251 |
| GROUP-III | 25 | 0.02956 | 0.008912 | 0.012 | 0.045 |
| TOTAL | 75 | 0.06855 | 0.047390 | 0.012 | 0.251 |
The occurrence of CIC is never a normal immune response. The half-life of such CIC is transitory in nature. Continued presence of CIC over extended periods however is a cause of consequence of some pathological condition or infection [20].
Presuming the involved antigen to be of malignancy-specific, serum CIC levels in cancer patients have been used for early diagnosis, metastaticspread, tumourburden, degree of aggressiveness, therapeutic response as well as prognosis [20].
In our study there is marked elevation of CIC values from Normal control to oral leukoplakia then to OSMF which is in accordance with the study conducted by Cynthia Jane in 2007 [3] ( Mean values in OD 450nm Normal-0.02315, Oral Leukoplakia-0.03817, Oral submucous fibrosis-0.1871).
In the present study out of 25 subjects 4 homogemous and 3 non homogenous leukoplakia showed high CIC values which is above OD450nm -0.08 deviates greately from the mean value from the Group I leukoplakia which is 0.05988 [Table/Fig-6]. This may be attributed to the fact that lesion carries a high relative risk for malignant transformation, which is in accordance with the study by Cynthia Jane in 2007 [3] (p < 0.002).
Non homogeneous leukoplakia accounted for the highest frequency of malignant transformation of 20%, whereas 3% of the homogeneous leukoplakia developed carcinoma [1].
In the same way OSMF subjects with clinical Grade IV showed high levels of CIC of OD 450 >0.2 which can be attributed to malignant transformation which is in accordance with the study by Cynthia Jane in 2007 [3] (p < 0.001).
The results of the present study however clearly show that there is an elevation in the CIC in patients with OSMF whereas minimal changes were observed in Oral leukoplakic groups.
This may be attributed to the fact that OSMF carries a high relative risk for malignant transformation. It is thus clear that the level of CIC may be of help in predicting the malignant transformation of OSMF which is in accordance with the similar study done by Remani et al in 1988 [21] . It is thus clear that the level of CIC may be of help in predicting the malignant transformation of OSMF.
The mean difference is significant at the 0.05 level between the three Groups I, II, III with p value < 0.0001 (Significant).
The results obtained in the present study are comparable with the study of Cynthia Jane et al in 2007 [15] which clearly show the raise in CIC levels from,
Normalcontrols-->Oral Leukoplakia-->Oral Submucous Fibrosis.
The CIC levels increase from normal controls to oral leukoplakia patients and then to OSMF patients.
Conclusion
The stages of the malignancy can be determined by the levels of CIC levels present in the serum. This can be correlated with histo pathological study and proper grading can be achieved. When studying the larger sample size, if the specific antigen for the tumour is identified and isolated from the serum, it will be helpful in treating the malignancy in a more specific manner to reduce the severity and also aids in curing of the disease.
These efforts may be of value for proactive intervention, especially in high risk groups with potentially malignant lesions and conditions, as the early detection decreases the morbidity and mortality of the diseases.