Twin Reversed Arterial Perfusion Syndrome (TRAP or Acardiac Twin)-A Case Report
Kalyani R.1, Mandeep S. Bindra2
1 Associate Professor, Department of Pathology, ESIC Medical College & PGIMSR, Bangalore, Karnataka, India.
2 Assistant Professor, Department of Pathology, CMC, Vellore, Tamil nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr Kalyani R., H.No: 127/13, “Sri Ganesh”, 4th main, 4th cross, P. C. Extension, Kolar-563101. Karnataka, India.
Phone: 9448402775,
E-mail: drkalyanir@rediffmail.com
Twin reversed arterial perfusion (TRAP) syndrome is a rare condition (0.3:10,000 births) that occurs in monochorionic twin pregnancies, resulting in coexistence of a normal “pump” twin and an acardiac twin. The acardiac twin is dependent upon the normal twin to provide circulation by means of vascular anastomosis. Many of the bizarre defects are felt to be caused by low oxygen tension and this causes dramatic alteration in the twin fetal physiology and high prenatal mortality. The acardiac twin is a parasite, putting the pump fetus at risk of high output cardiac failure. Overall only 50% of pump twins survive. We present a case in a twenty year female, gravida two, para one, living one, full term normal pregnancy, ultrasound showed twin pregnancy. Following delivery, the first fetus survived only for one day and the second fetus showed features of TRAP syndrome.
Acardiac twin, fetal anomaly, twin reversed arterial perfusion syndrome
Case Report
Twenty year old female with gravida two, para one, living one, non-consanguious marriage, seven months amenorrhoea presented with over distended abdomen. Examination showed multiple fetal parts, fetal heart sound not localised, cervix 30% effaced and 0.5 cms dilated. Ultrasound examination showed twin monochorionic diamniotic intrauterine pregnancy with viable first twin. The second twin showed large cystic lesion around head & neck, upper extremities, chest and abdomen with no cardiac activity. Anatomy of the fetus was distorted. A provisional radiological diagnosis of Cystic Hygroma was made. Patient underwent therapeutic amniocentesis and was discharged. Two weeks later, on second admission patient underwent emergency caesarean section for severe oligohydramnious of first fetus.
The first fetus was male (pump twin) which survived for 24 hours and the second was still born. A diagnosis of fetal papyraceous / massive cystic hygroma (second fetus) with fetal (first twin) demise was made. The consent for autopsy of first twin was not obtained. Consent for autopsy of second twin was obtained.
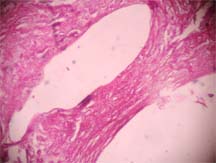
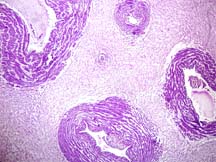
The second male twin at autopsy weighted 2.3 Kg. A provisional clinical diagnosis of cystic hygroma was made. External examination showed a cystic mass around head and neck to sacrum involving proximal 3/4th of upper limb with flap like distal 1/4th of upper limb having two fingers [Table/Fig-1]. Both feet showed 4 toes and absence of small toe. Depressed nasal bridge and cleft palate was noted. The consent for autopsy obtained. Cystic mass on dissection showed multiloculated subcutaneous cystic spaces containing about 2000 ml of straw colour fluid. Internal examination showed rudimentary cardia with absence of lungs, liver, gall bladder and spleen [Table/Fig-2]. Microscopy showed focal calcification in rudimentary heart [Table/Fig-3], pancreas, adrenals and skin showed oedematous dermis. Umbilical cord measured 8 cms in length and cut section showed three vessels. Microscopy showed one artery, two veins and one very small (rudimentary) artery [Table/Fig-4]. Cranium showed only membranous structures grossly [Table/Fig-5] and microscopy showed multiple dilated blood vessels. Final Diagnosis was TRAP syndrome.
Gross photograph of fetus showing cystic dilated sac around head, neck & upper half of the body with deformed face and upper limb.

Gross photograph showing loculated cystic spaces around upper half of the body with thorax & abdominal contents having rudimentary heart, absence of lung, liver & spleen.

Microphotograph of rudimentary heart showing cystic spaces with myocardium. (H&E x 100)
Microphotograph of umbilical card showing two veins, one artery and one rudimentary artery. (H&E x 100)
Gross photograph showing cranial cavity having only membranous vascular structure.

Discussion
TRAP syndrome is a rare obstetric condition unique to monozygotic monochorionic twin pregnancies in which there is co-existence of a normal pump (donor) twin and an acardiac recipient (perfuse) twin [1–4]. The incidence of TRAP syndrome is 1 in 35,000 pregnancies, 1 in 100 monozygotic monochorionic twin gestation and 1 in 30 monochorionic triplet gestation [1–6]. Most cases are seen in twins with only 8% in triplets [5]. The risk in multiple pregnancies of a higher order is ever greater [6].
The acardiac twin is dependent upon the normal twin to provide blood by means of anomalous reversal of umbilical arterial flow which results from umbilical artery to artery or venous to venous anastomosis between two circulations of twins which develops at 3-4 weeks of gestation [1,3,4,6]. Exact pathogenesis is not known. One theory explains that umbilical vascular anastomosis in early embryogenesis in fused placenta resulting in vascular disruption, early tissue hypoxia in one twin giving rise to atrophy of heart and other organs [1–4]. Other theory postulates that severe genetic/other primary cardiac embryogenesis defect first cause the failure of cardiac development in one twin followed by anastomosis between umbilical vessels allowing survival of affected twin [1–6]. In one case report, there is association of TRAP with VACTERL which indicates defect in early embryogenesis [7]. Chromosomal disorder has been reported in 50% of cases of TRAP syndrome [1,4]. A case of TRAP syndrome reported in triamniotic dichorionic triplet pregnancies conceived by in-vitro fertilization [6]. Monochorionicity always highlights risk of TRAP. In our case it was monochorionic and diamniotic twins. Chromosomal analysis was not done in our case.
The acardiac twin becomes dependent on the perfusion of the “Pump” twin. The upper half of the body of an acardiac twin is extremely poorly developed and sometimes not developed at all. Head, cervical spine and upper limbs are usually absent. Oedema in the upper body consistent with cystic hygroma is common. In contrast the lower half of the body although malformed is better developed. This is because of mechanism of perfusion of the acardiac twin where blood enters via abdominal aorta is deoxygenated blood that left the normal twin. So the oxygen and nutrition available is extracted allowing some development of caudal aspect. Once blood enters upper torso in retrograde fashion oxygen saturation is extremely low, halting development of heart, head and upper torso giving rise to severe deficits. The pump twin suffers from high output cardiac failure which is directly proportional to size/weight of the acardiac twin [2].
The anomalies in acardiac twin are partial/total absence of cranial vault, holoprosencephaly, absent facial structures, anophthalamia, micro-ophthalmia, cleft lip, cleft palate, absent or rudimentary limbs, diaphragmatic defects, absent lungs & heart, oesophageal atresia, ventral wall defects, ascites, absent liver & gall bladder, oedema of the skin, single umbilical artery (75% cases), markedly different sized umbilical artery, inconsistent membrane development between the twins and occasionally umbilical artery drawn directly into superior mesentric artery [2,3]. Depending on anomalies the acardiac twin are classified as hemiacardius (if the heart is incompletely formed) and holocardius (if the heart is absent). Other classification is acephalus (if head is absent), anceps (if head is poorly formed), acormus (presence of head only) and amorphous (unrecognizable amorphous masses) [2–5]. The classifications have little significance as acardiac fetus is invariably fatal and the importance of survival of pump twin is the priority [2]. In our case the acardiac fetus showed calcification in heart, pancreas, adrenals and umbilical cord showed four vessels with membranous structures in the cranium.
Congenital anomalies are present in about 9% of pump twins; however pump twin presents with ascites, pleural effusion, polyhydramnios and skin oedema which are features of congestive heart failure [2,4]. In the present case the consent for autopsy of pump twin was not given.
Prenatal diagnosis by ultrasound is suspected when a twin gestation presents with discordance and bizarre malformations with retrograde blood flow in acardiac twin demonstrated by pulsed/colour flow Doppler [1,2]. Anencephaly, cystic hygroma, conjoined twins, twin demise and intramniotic placental tumours are differential diagnosis to be ruled out. In our case ultrasound diagnosis of cystic hygroma was made.
Recurrence of TRAP syndrome is unknown/not increased, likely to be low and the couples can therefore be counselled optimistically for future pregnancy [2,5].
The prognosis in TRAP syndromes is lethal for acardiac twin [1,2]. The fetal mortality of the pump twin is extremely high [50-75%] because high output cardiac failure [1–6]. A case of survivor pump twin with TRAP sequence is reported who had poor neurological outcome on long them follow-up [5]. In our case, the pump twin survived for 24 hours and acardiac twin was still born.
Conclusion
The obstetrician and radiologist should be aware of this anomaly especially in twin/multiple pregnancies so that timely proper measures can be taken to survive the pump twin. The pathologist should also be aware of this entity so that proper autopsy report can be given to the parents so that they can plan their future pregnancy. This also highlights the importance of fetal autopsy.
[1]. Chia-Jen Wu, Dah-Ching Ding, Shi-Shih Ren, Cheng-Chang Chang, Jueng-Tsueng Weng, Kwei-Shai Hwang, Prenatal diagnosis and management of Twin Reversed Arterial Perfusion (TRAP) syndromeTaiwan J Obstet Gynecol 2008 47(1):126-128. [Google Scholar]
[2]. Steffensen TS, Gilbert-Barness E, Spellacy W, Quintero RA, Placental Pathology in TRAP sequence: clinical and pathologic implicationsFetal Pediatr Pathol 2008 (1):13-29. [Google Scholar]
[3]. Hanafy A, Peterson CM, Twin Reversed arterial perfusion ( TRAP) sequence: case report and review of literatureAust N Z J Obstet Gynaecol 1997 May 37(2):187-91. [Google Scholar]
[4]. Kariappa TM, Chidananda HT, Mamatha R, Acardiac twin: an unusual case reportIndian J Pathol Microbiol 2007Oct 50(4):801-3. [Google Scholar]
[5]. Chih-Chen Chen, Yu-Hsin Hsu, Te-Fu Chan, Shyng-Shiou F Yuan, Jinu-Huang Su, Poor long-term outcome in a survivor presenting with the twin reversed arterial perfusion sequence In-utero: A case reportKaohsing J Med Sci 2003 19(10):526-30. [Google Scholar]
[6]. Chaliha C, Schwarzler P, Bookes M, Battash MA, Ville Y, Case report: Trisomy 2 in an acardiac twin in a triplet in-vitro fertilization pregnancyHuman Reproduction 1999 14(5):1378-80. [Google Scholar]
[7]. Athwal Sharan, Millard Katherine, Lakhoo Kokila, Twin reversed arterial perfusion (TRAP) sequence in association with VACTERL association: a case reportJournal of Medical Case Reports 2010 4:411 [Google Scholar]