Right Bundle Branch Block: An Uncommon Cardiotoxic Manifestation of Hair Dye Poisoning-A Case Report
Deepak Balasubramanian1, Saravanan Subramanian2, Pugazhenthan Thangaraju3, Kani Shanmugam4
1 Resident, School of Public Health, PGIMER, Chandigarh, India.
2 Senior Assistant Professor, Department of Medicine, Thoothukudi Government Medical College, Thoothukudi.
3 Medical Officer, Central Leprosy Training and Re-search Institute, Chengal-pattu, Tamil Nadu, India.
4 Professor, Department of Medicine, Thoothukudi Government Medical College, Thoothukudi, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deepak Balasubramanian, Resident, School of Public Health, PGIMER, Sector 12, Chandigarh, India.
Phone: 09988793364,
E-mail: deep19882000@gmail.com
Hair dye poisoning has been rising in incidence in the recent years. Apart from the commoner manifestations of upper airway edema, rhabdomyolysis and acute renal failure, cardiac toxicity, convulsions and sudden cardiac death are relatively rare complications. We discuss a case of hair dye poisoning manifesting as oropharyngeal edema along with cardiac complication. The patient survived.
Hair dye poisoning, Paraphenylenediamine, Myocarditis
Introduction
The incidence of Hair dye poisoning is increasing in many places in India [1, 2] and it constitutes a significant proportion of the poisoning cases in some regions [3]. It manifests as upper airway edema compromising the airway, rhabdomyolysis, acute renal failure and multi organ damage [2]. Myocarditis is a rare complication, which is also life threatening [4]. Unless the patient is monitored continuously and prompt treatment instituted, it may prove fatal.
Case
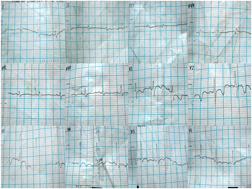
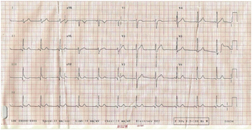
A 15-year-old male presented to the emergency department 1 hour after consumption of 70ml of Hair dye with complaints of difficulty in breathing, swelling in the neck region and vomiting. The patient’s mother revealed that he had no prior history of poisoning, epilepsy and heart disease. Examination revealed edema of the submandibular, sublingual & lingual area. There was no carpopedal spasm or trismus. Patient was anxious with a pulse rate of 108/minute, respiratory rate of 26/minute, Blood pressure – 110/70mmHg. Patient was given oxygen therapy, Injection Hydrocortisone sodium 200mg stat followed by 100mg tds, Injection Chlorpheniramine maleate 2ml i.m bd, Injection Ranitidine 50mg i.v. bd, intravenous antibiotics (Parenteral Cefotaxime) & FAD (Forced Alkaline Diuresis) cycle was started. Electrocardiogram showed sinus tachycardia [Table/Fig-1] (a). The pulse rate was 120/minute, Blood pressure 116/70 mmHg and respiratory rate was 32/minute. As the patient developed stridor, he was taken up for emergency tracheostomy [Table/Fig-2]. Investigations taken at the time of admission were normal [Table/Fig-3] except for raised CPK levels (50150 U/L), elevated liver enzymes and dark coloured urine. Follow up ECG taken up on the next day revealed a Right Bundle Branch pattern [Table/Fig-1] (b), but patient had no complaints. The pulse rate was 94/minute, blood pressure was 114/76 mmHg and respiratory rate 20/min. Blood investigations revealed raised CPK levels and positive Troponin-T. The changes persisted on the third and fourth day [Table/Fig-1(c)] . The vitals were normal during this period. ECG taken on the fifth day showed diffuse T wave inversion [Table/Fig-1(d)] in the chest leads. The patient was asymptomatic, was discharged and advised follow up after a week. But, as the patient was from a far off place, he came for review only after 2 weeks. ECG taken revealed normal sinus rhythm [Table/Fig-1(e)] with pulse rate of 66/minute, blood pressure of 108/70 mmHg and respiratory rate was 16/minute. Echocardiography performed on the 2nd day, at the time of discharge and during follow up was normal.
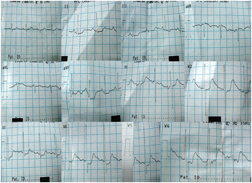
Right Bundle Branch Block
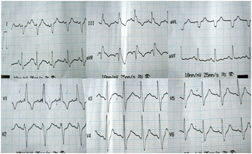
Right Bundle Branch Block
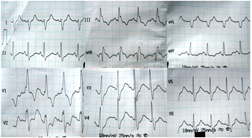
Follow up ECG showing diffuse ‘T’ wave inversion in the chest leads
Normal ECG at 20 at follow upBundle Branch Block

Biochemical investigations of the patient
| BLOOD INVESTIGATIONS |
|---|
| Day of admission | Day 3 in the hospital | On the day of discharge |
| Hemoglobin (13.0-16.2 g/dL) | 16 | | |
| TC (4100-10900 cells/mm3) | 9000 | | |
| DC (45-62%, 16-33%, 1-3%) | 52,45,3 | | |
| ESR (0-8) | 2,6 | | |
| CPG (70-110 mg/dL) | 120 | | |
| Urea (7-18 mg/dL) | 30 | 28 | 26 |
| Creatinine (0.7-1. mg/dL) | 1 | 1.1 | 1.1 |
| Bicarbonate (22-28 mEq/L) | 18 | 22 | 26 |
| CPK (25-192 U/L) | 50150 | 30080 | 3369 |
| Troponin T (0-0.02 μg/L) | | Positive | |
| Na+ (137-147 mEq/L) | 135.9 | 127.4 | |
| K+ (3.6-5.1 mEq/L) | 4.99 | 3.6 | |
| Ca+ (8.4-10.2 mg/dL) | 8.2 | | |
| SGOT (8-40 IU/L) | 541 | | 110 |
| SGPT (5-20 IU/L) | 140 | | 72 |
| ALP (53-128 U/L) | 46 | | 50 |
| URINE INVESTIGATIONS |
| Volume(ml/24hrs) | 1500 | 3300 | 1400 |
| Colour | Black | Dark | Straw coloured |
| Albumin | Loaded | Traces | Nil |
| Sugar | Nil | Nil | Nil |
| Deposit | Full of Pus cells, 4-8 RBC | Few pus cells, 2-6 RBC | Scanty Pus cells, 1-2 RBC |
Discussion
The incidence of Hair dye poisoning has been increasing over the past few years. Suicide (98%) was the most common reason for ingestion, followed by accidental and homicidal [2,4]. Most of the cases consumed the hair dyes orally [4]. Mortality rates in the larger studies varied from 6.8% to 22.48% [1,2,5]. The reasons behind the increasing incidence might be the strict regulations of the sale of other poisonous substances like organophosphorus compounds, which make hair dye a dearer option. Secondly, hair dyes are easily available in the household for the young adults [1] (who constitute a majority of the population affected) whose parents use the hair dye. Thirdly, the hair dye is cheap and easily available in the market. Fourthly, there is availability of information on the Internet, mass media and peer groups regarding the high morbidity and mortality of hair dye poisoning.
Hair dye poisoning presents a variety of manifestations. Myocarditis is one of the rare complications. Previous studies report a myocarditis incidence of 15% with a high mortality rate of 29% [4]. But the incidence is bound to vary with patients differing in their susceptibility to Paraphenylenediamine, apart from the amount of dye ingested. Singh AP et al., present a case with Right bundle branch block, supraventricular and ventricular ectopics with elevated parameters of myocardial damage and the patient could not be revived [6]. In another case published by Singh N et al., patient developed ST segment elevation and T wave inversion in anterior chest leads with elevated biochemical parameters and the patient expired [7]. Right Bundle Branch Block (RBBB) is a relatively rare (4.0%) Electrocardiographic (ECG) finding in myocarditis [8].
A new onset RBBB in a patient without heart disease is associated with increased future cardiovascular risk and mortality in addition to being associated with increased rate of myocardial infarction and pacemaker implantation [9]. Moreover, this association seems to be stronger in younger patients [9,10]. The Bundle Branch blocks usually remained for months, but in our case, it was transient only [11].
The patient survived the episode of myocarditis in our case as the patient had consumed only 70 ml of hair dye containing approximately 2.8 g of paraphenylenediamine. Studies suggest that myocarditis is a dangerous complication at doses greater than 10 g [4]. Many studies relate the toxicity of the dye with the dose ingested [2,4,12]. A study measuring the plasma level of paraphenylenediamine in hair dressers showed very low levels [13]. Though studies have been done measuring urinary and plasma levels [14], they are usually not measured as individual sensitivity to the dye also varies. Moreover the patient had vomited after consumption of the hair dye, which might have washed out the poison from the stomach, thereby, reducing the exposure. The young age o the patient also favored a good prognosis [9].
The patient presented with signs and symptoms of upper airway edema, but myocarditis manifested only on the 2nd day. This might be related to the biphasic blood clearance of paraphenylenediamine. The half lives recorded in animal studies are 24 minutes and 43.5 hours with blood concentration rising steadily for the first 24 hours [15].
Our patient was given psychiatric counseling before discharge. For addressing this emerging problem, a dual pronged approach is necessary. First, we need to address the cause and motives behind the hair dye consumption. This may be through 24 hours support services, psychiatric counseling and more research into the reason behind this problem. The patient should be counseled in such a manner that he goes back to his community and propagates the harms of this poisoning, discouraging people from consuming it. Second, we would need to enforce regulations on the sale of hair dye, to reduce access to vulnerable population. Implementing these solutions might help reduce the burden on the family and healthcare system.
[1]. Mary Nirmala S, Ganesh R, Hair dye—an emerging suicidal agent: our experienceOtolaryngology Online Journal 2012 2(2):1-11. [Google Scholar]
[2]. Jain PK, Agarwal N, Kumar P, Sengar NS, Akhtar A, Hair dye poisoning in Bundelkhand region (prospective analysis of hair dye poisoning cases presented in Department of Medicine, MLB Medical College, Jhansi)J Assoc Physicians India 2011 59(415-9)Epub 2012/02/10 [Google Scholar]
[3]. Kiran GU, Shilpa N, Reddy KR, Babu SC, Reddy KVY, A prospective observational study on prevalence of poisoning cases – focus on vasmol poisoning (para-phenylenediamine (PPD) poisoning)European Journal of Hospital Pharmacy: Science and Practice 2012 19(2):225-6. [Google Scholar]
[4]. Jain PK, Sharma AK, Agarwal N, Sengar NS, Siddiqui MZ, Singh AK, A prospective clinical study of myocarditis in cases of paraphenylenediamine (hair dye) poisoning in Northern IndiaJournal of Clinical Medicine Research 2012 4(7):106-16. [Google Scholar]
[5]. Radhika D, Mohan KVM, Sreenivasulu M, Reddy YS, Karthik TS, Hair Dye Poisoning-A Clinicopathological Approach and ReviewJ Biosci Tech 2012 3(4):492-7. [Google Scholar]
[6]. Singh AP, Jatav OP, Dudani M, Myocarditis in hair dye poisoningIndian Heart J 2009 61(3):306-7.Epub 2010/05/28 [Google Scholar]
[7]. Singh N, Jatav OP, Gupta RK, Tailor MK, Myocardial damage in hair dye poisoning—an uncommon presentationJ Assoc Physicians India 2008 56:463-4.Epub 2008/10/01 [Google Scholar]
[8]. Ukena C, Mahfoud F, Kindermann I, Kandolf R, Kindermann M, Böhm M, Prognostic electrocardiographic parameters in patients with suspected myocarditisEuropean Journal of Heart Failure 2011 13(4):398-405. [Google Scholar]
[9]. Bussink BE, Holst AG, Jespersen L, Deckers JW, Jensen GB, Prescott E, Right bundle branch block: prevalence, risk factors, and outcome in the general population: results from the Copenhagen City Heart StudyEur Heart J 2013 34(2):138-46.Epub 2012/09/06 [Google Scholar]
[10]. Fernández-Lozano I, Brugada J, Right bundle branch block: are we looking in the right direction?European Heart Journal 2013 34(2):86-8. [Google Scholar]
[11]. Nakashima H, Honda Y, Katayama T, Serial electrocardiographic findings in acute myocarditisIntern Med 1994 33(11):659-66.Epub 1994/11/01 [Google Scholar]
[12]. Kondle R, Pathapati RM, Saginela SK, Malliboina S, Makineedi VP, Clinical profile and outcomes of hair dye poisoning in a teaching hospital in nelloreISRN Emergency Medicine 2012 2012(5) [Google Scholar]
[13]. Hueber-Becker F, Nohynek GJ, Dufour EK, Meuling WJ, de Bie AT, Toutain H, Occupational exposure of hairdressers to [14C]-para-phenylenediamine-containing oxidative hair dyes: a mass balance studyFood Chem Toxicol 2007 45(1):160-9.Epub 2006/10/13 [Google Scholar]
[14]. Hooff GP, van Huizen NA, Meesters RJW, Zijlstra EE, Abdelraheem M, Abdelraheem W, Analytical investigations of toxic phenylenediamine (PPD) levels in clinical urine samples with special focus on MALDI-MS/MSPLoS ONE 2011 6(8):e22191 [Google Scholar]
[15]. Rehani MM, Jain IS, Sharma SK, Distribution kinetics of 3H—labeled p-phenylene diamine—a hair dyeThe Indian Journal of Medical Research 1981 74:129-34. [Google Scholar]