Dengue fever (DF) is transmitted by Aedes aegypti mosquitoes. Dengue virus belongs to genus Flavivirus and has four sero-types namely, DEN-1, DEN-2, DEN-3 and DEN-4 [1]. Infection with one sero-type gives lifelong immunity to same sero-type and temporary immunity to other sero-types [1]. Infection with multiple sero-types and secondary infections manifest severely than primary infections [2]. With growing population, rapid urbanization and lack of appropriate sanitary measures, proliferation of mosquitoes and subsequent dengue infections have increased rampantly with an estimated 30-fold increase in incidence over last five decades [1]. Dengue fever can manifest as milder undifferentiated fever and dengue fever or much severe disease like dengue hemorrhagic fever and dengue shock syndrome [1]. Mortality in untreated cases is as high as 20% against 1% in treated cases [1]. With rising disease burden atypical manifestations have increased as well which are missed most often due to lack of awareness. Our aim of the study was to look for the atypical manifestations of dengue fever.
Materials and Methods
It is a prospective hospital based observational study conducted at hospitals of Kasturba Medical College in Mangalore, India, over a period of two years (June–2010 to May–2012). All probable dengue cases were investigated initially. Out of them, 150 ELISA confirmed IgM-dengue sero-positive cases aged 18 years and above, satisfying WHO criteria were included in the study group after ruling out other causes of fever. A detailed clinical history, physical examination and baseline investigations were undertaken and followed-up till the patient got discharged from hospital. All clinical and laboratory details were carefully reviewed with daily assessment during hospital stay as per pre-tested questionnaire and data of atypical presentations were recorded.
Ethical Considerations
Departmental approval for the study and informed consent from the patients had been obtained.
Results
Average duration of fever was 5.64 days (standard deviation 1.977 and range 1-16 days). Common symptoms noticed were myalgia (54.6%), headache (54.6%), rash (41.3%), arthralgia (32.7%) and petechiae (19.33%). Most common abdominal symptoms were nausea (43.3%), vomiting (40%), pain in abdomen (41.3%), dyspepsia (32%) and loose stools (12%). Altered liver enzymes were seen in 92.66% cases. 92.7% patients had aspartate transaminase (AST) >40u/l and three-fold increase was seen in 58.7%. 85.3% patients had alanine transaminase (ALT)>40u/l and three-fold increase was seen in 38.7% cases.
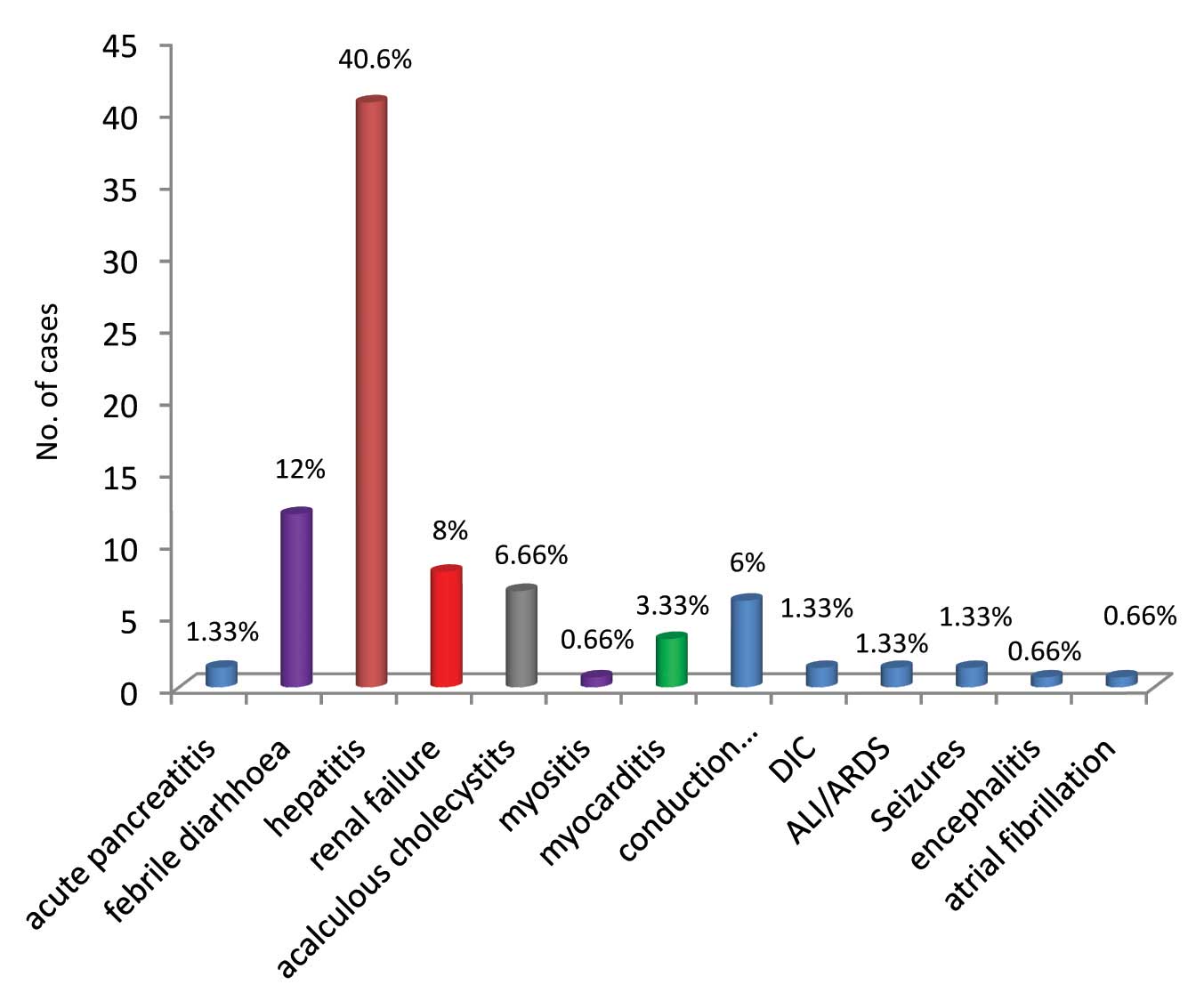
Most common atypical manifestation was hepatitis found in 40.6% patients. Febrile diarrhea (12%), renal failure (8%), acalculous cholecystitis (6.66%) and conduction abnormalities of heart (6%) were among other common manifestations [Table/Fig-1]. Other less common manifestations were encephalitis, seizures, acute lung injury (ALI)/acute respiratory distress syndrome (ARDS), disseminated intravascular coagulation (DIC), acute pancreatitis, myositis/rhabdomyolysis and atrial fibrillation. Most common conduction abnormality was sinus bradycardia seen during convalescence, while others were heart blocks and atrial fibrillation [Table/Fig-2]. Three patients with dengue hemorrhagic fever died of multi-organ dysfunction, DIC and shock. Out of them one patient also had a major intracranial bleed. Overall final outcome was good with a recovery rate of 98% and 2% mortality. There was no significant difference in bleeding noted among patients with decreased platelet counts. 35.4% of bleeding manifestations were seen in patients with platelet < 20,000 cells/mm3 and 37% with platelet count between 20,000 cells/mm3 to 50,000 cells/mm3. Platelet counts ranged from 8,000 cells/mm3 to 4,31,000 cells/mm3 with hematuria as manifestation at 8000 cells/mm3 platelet count. Majority of the bleeding manifestations were minor events (petechiae, hematuria, gum bleeding, melena) and not life-threatening. Type/severity of bleeding did not correlate well with platelet count as they were seen at varied platelet counts, signifying the fact that factors other than thrombocytopenia might be contributory like platelet dysfunction, consumption coagulopathy and endothelial dysfunction.
Atypical manifestations ofdengue fever DIC - Disseminated intravascular coagulation, ALI - Acute lung injury, ARDS - Acute respiratory distress syndrome
Analysis of data among survivors and expired patients.
| Expired 1 | Expired 2 | Expired 3 | Mean Values in Alive |
|---|
| Bleeding | Hematuria, Petechae | Hematuria, Subconjuctival Hemorrhage, Intracranial Bleed, Petechae | Epistaxis, Hematuria, Petechae |
|---|
| BP | hypotension | hypotension | hypotension | |
| Creatinine | 3.9 | 4.3 | 3.2 | 1.01 |
| urea | 104 | 34 | 27 | 22 |
| Total bilirubin | 1.4 | 0.9 | 11 | 0.9 |
| Albumin (g/dl) | 3.1 | 3.7 | 4.1 | 3.7 |
| AST (u/l) | 7595 | 217 | 791 | 292 |
| ALT (u/l) | 2839 | 96 | 1147 | 168 |
| Clinical manifestations | Pleural effusion, ascites, acalculous cholecystitis, ARDS, ARF, DIC, hepatitis | Pleural effusion, Ascites, hemorrhagic encephalopathy, Transtentorial herniation | Pleural effusion, ascites, status epilepticus, ARF, fulminant hepatic failure, DIC, microangiopathic hemolytic anemia | |
ARF-acute renal failure, ARDS-acute respiratory distress syndrome, DIC-disseminated intravascular coagulation, AST-aspartate transaminase, ALT-alanine transaminase, BP-blood pressure
Discussion
With an average incubation period of four to six days dengue fever presents with diffuse flushing or fleeting eruptions over the body evolving into maculopapular rash on third day of illness. Subsequently at defervescence rash fades and petechiae appear [1]. Sixteen days fever was a rare manifestation in one of our patients. Other symptoms noticed were as described in results. Just before or at defervescence is the critical phase when plasma leak usually happens, preceded by thrombocytopenia and leucopenia [1]. Hence, monitoring of vitals, postural drop of blood pressure, thrombocytopenia, serum albumin and rising hematocrit are very important to monitor for early signs of shock [1]. In the first week of presentation, NS1 antigen assay can be used to diagnose in suspected cases. Usually IgM dengue levels become positive only after one week of illness and to be ordered only after first week of illness. In our institution, we follow WHO protocol of management for dengue fever. As against the general consensus among people, platelet count was not the major cause of morbidity. Severity of bleeding did not correlate well to platelet count. Time to recovery of thrombocytopenia was three to four days. If recovery time exceeds this, other causes like ITP have to be ruled out. Platelet transfusion is advocated only in the presence of bleeding manifestations and counts less than 10,000 cells/mm3. FFP transfusion may be needed for DIC. According to proposed new classification of WHO, dengue is classified into severe dengue, dengue with warning signs and dengue without warning signs [3]. Early warning signs of dengue like pain in abdomen, persistent vomiting, hepatomegaly, hematocrit rise and evidence of fluid leak should be observed carefully for timely intervention to prevent shock and severe complications. Apart from one major intracranial bleed, most of the patients had only minor bleeding manifestations like petechiae, hematuria, gum bleeding and melena. Shock secondary to vascular leak, DIC and multi-organ dysfunction were the major cause of morbidity [1] [Table/Fig-1]. Karoli et al., study had 6% mortality as against 2% in our study group [4].
Atypical Manifestations of Dengue Fever
More than half of our study group had one or the other atypical manifestations. Most common atypical manifestation was hepatitis found in 40.6% patients. Febrile diarrhea, renal failure, acalculous cholecystitis and conduction abnormalities of heart were among other common manifestations. Other less common manifestations noted were, as listed in [Table/Fig-1]. As per the WHO guidelines for dengue fever, a list of atypical or unusual manifestations also termed ‘Expanded Dengue Syndrome’ are mentioned [1]. These could be explained as complications of severe profound shock or associated with underlying host conditions/diseases or co-infections [1].
Abdominal symptoms are the most important in dengue fever. They were seen in 2/3rd of our patients (70%). Among them nausea, vomiting, pain in abdomen and dyspepsia were leading symptoms in our study group (63% in Karoli et al., study) [4]. As a clinician, one must be very vigilant about symptoms like pain in abdomen and vomiting as these are the early warning signs before worsening to severe dengue [3]. General practitioners may be confused as hepatitis, whereas surgeons might think in terms of acute abdomen. If observed and managed in time, most of the complications of dengue can be prevented. Especially in dengue endemic areas, any patient with pain in abdomen has to be evaluated for dengue fever if other findings are suggestive of viral fever. Hepatitis, fulminant hepatic failure, Acalculous cholecystitis, acute pancreatitis, acute parotitis and febrile diarrhea are among the gastrointestinal manifestations reported [5].
Hepatitis presents as right hypochondriac pain, hepatomegaly and raised aminotransferases with liver enzymes peaking after first week of illness and normalizing in three weeks [5]. Jaundice is not evident in most of the cases and patients with hepatitis have a longer recovery time compared to uncomplicated cases. Direct cytopathic effect of dengue virus on liver cells has been proven in previous studies [6]. Fulminant hepatic failure is usually secondary to shock and DIC in severe dengue fever. Acalculous cholecystitis presents with right upper quadrant abdominal pain often radiating to right shoulder. Ultrasound abdomen reveals gall bladder mucosal edema and pericholecystic fluid without any gallstones secondary to vascular leakage of plasma [7–9]. Unlike other secondary causes, dengue related acalculous cholecystitis resolves spontaneously with supportive care in majority of cases. Although, there are isolated cases with gangrene and perforated gall bladder with peritonitis needing surgical intervention [5,7,8].
Acute pancreatitis is a rare complication of dengue fever due to possible direct cytopathic effect of virus or an autoimmune response by molecular mimicry causing pancreatic outflow obstruction by resulting edema although exact mechanism is unknown [10]. Ultrasound abdomen is characterized by enlarged pancreas and elevated serum amylase and lipase levels [10,11]. There are few case reports of febrile diarrhea in dengue patients as well [5]. Shock induced acute tubular necrosis is the main cause of renal failure in dengue patients apart from other rare causes like multi-organ dysfunction and rhabdomyolysis [5,12]. While classic dengue fever presents with myalgia and arthralgia, there are quite a few case reports of myositis/rhabdomyolysis in dengue patients which is mainly a cytokine mediated muscle damage [5,13]. These patients need to be detected promptly as there is a risk of progressing to renal failure if not identified in time. Rhabdomyolysis can be detected with haeme positivity in urine and elevated creatinine phosphokinase levels. Electromyography and muscle biopsy may be confirmatory for myositis. While rhabdomyolysis is managed with adequate fluid replenishment, myositis responds well to corticosteroids [5,13].
Cardiac manifestations of dengue are uncommon but cardiac rhythm disorders such as atrio-ventricular blocks, atrial fibrillation, sinus node dysfunction and ectopic ventricular beats have been reportedly attributed to viral myocarditis [5,14,15]. Majority of our patients were asymptomatic and had a spontaneous resolution as is the case in previous case reports. However, symptomatic and persistent defects might warrant support with specific drugs or pacemaker until resolution as needed apart from correcting treatable causes like electrolyte imbalances [14]. Acute lung injury (ALI) and Acute Respiratory Distress Syndrome (ARDS) are one of the dreaded complications of dengue hemorrhagic fever, secondary to increased alveolar-capillary membrane permeability leading to interstitial and alveolar edema. Early restoration of adequate tissue perfusion is critical to prevent progression of dengue shock syndrome to ARDS [5]. However, equal care must be exercised to avoid excessive fluid infusion after adequate volume replacement because fluid overload may result in ARDS. Pulmonary haemorrhage is another fatal complication to watch out for in these patients [5].
Neurological manifestations like seizures, encephalopathy, encephalitis/aseptic meningitis, intracranial haemorrhages and neuropathies have been reported in the past [5,16]. These manifestations are secondary to direct tissue invasion of virus (neurotropicity), cytokine mediated damage to the blood brain barrier, capillary hemorrhage, DIC, cerebral edema and metabolic derangements like hyponatremia, hypoxia, hepatic encephalopathy and uremic encephalopathy [5]. CSF analysis can be done to confirm in encephalitis/asceptic meningitis. Although rare, there has been isolated case reports of mononeuropaties, polyneuropaties, Gulliane Barre’ syndrome, acute disseminated encephalomyelitis and transverse myelitis [5,16]. We had a young patient who presented with severe headache, vomiting, neck rigidity and altered sensorium. He had a fatal complication with hemorrhagic encephalopathy worsening into transtentorial herniation, brainstem dysfunction and death. One patient presented with headache and altered sensorium who initially had an episode of GTCS seizures. She later developed myoclonic jerks and further into status epilepticus. Main line of management is supportive care with fluid resuscitation, intubation and mechanical ventilation, if needed in comatose patients, FFP transfusion for DIC, antiepileptics for seizures, correction of metabolic derangements and physiotherapy for neuropathies. 14% patients had neurological manifestations in Karoli et al., study as against 2% in our study [4].
Conclusion
Clinicians should have a high index of suspicion to detect and timely manage the atypical manifestations of dengue fever as they are no more a rare entity and will continue to rise so long as they are looked for carefully in dengue patients. Clinical vigilance about these presentations is important as some of these proved fatal in our study group. Some of these manifestations are no more atypical and might need to evaluate for dengue fever if seen, especially, in endemic areas.
ARF-acute renal failure, ARDS-acute respiratory distress syndrome, DIC-disseminated intravascular coagulation, AST-aspartate transaminase, ALT-alanine transaminase, BP-blood pressure