Hypohidrotic Ectodermal Dysplasia (ED): A Case Series
Mallika Kishore1, Sunil R. Panat2, Ashish Aggarwal3, Nupur Agarwal4, Nitin Upadhyay5, Kratika Ajai6, Abhijeet Alok7
1Post Graduate Student, Department of Oral Medicine and Radiology,Institute of Dental Sciences, Bareilly, Uttar Pradesh, India.
2Professor & Head of Department, Department of Oral Medicine and Radiology,Institute of Dental Sciences, Bareilly, Uttar Pradesh, India.
3Senior Lecturer, Department of Oral Medicine and Radiology,Institute of Dental Sciences, Bareilly, Uttar Pradesh, India.
4Senior Lecturer, Department of Oral Medicine and Radiology,Institute of Dental Sciences, Bareilly, Uttar Pradesh, India.
5Senior Lecturer, Department of Oral Medicine and Radiology,Institute of Dental Sciences, Bareilly, Uttar Pradesh, India.
6Post Graduate Student, Department of Oral Medicine and Radiology,Institute of Dental Sciences, Bareilly, Uttar Pradesh, India.
7Post Graduate Student, Department of Oral Medicine and Radiology,Institute of Dental Sciences, Bareilly, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mallika Kishore, Post Graduate Student, Department of Oral Medicine and Radiology, Institute of Dental Sciences, Bareilly, Uttar Pradesh, India.
E-mail: dr.mallika.kishore01@gmail.com
Ectodermal Dysplasia (ED) is a rare disorder with defects in two or more of the following structures: the teeth and the skin and its appendages including hair, nails, eccrine, and sebaceous glands. Dental manifestations include hypodontia, complete anodontia or malformed teeth. The most common form of the ED syndrome is hypohidrotic ED and is usually inherited as an X-linked recessive trait. Female carriers may have a variable degree of clinical manifestations. The condition is thought to occur in approximately 1 in every 100,000 live births. Dental treatment for these patients varies on an individual basis. Children with ED are often treated dentally with conventional adult appearing prosthesis which are focused only on the oral manifestations of the syndrome. We are here reporting two classical cases of hypohidrotic ED with a review of the literature.
Ectodermal dysplasia, Genetic disorder, Hypohidrotic
Case Report
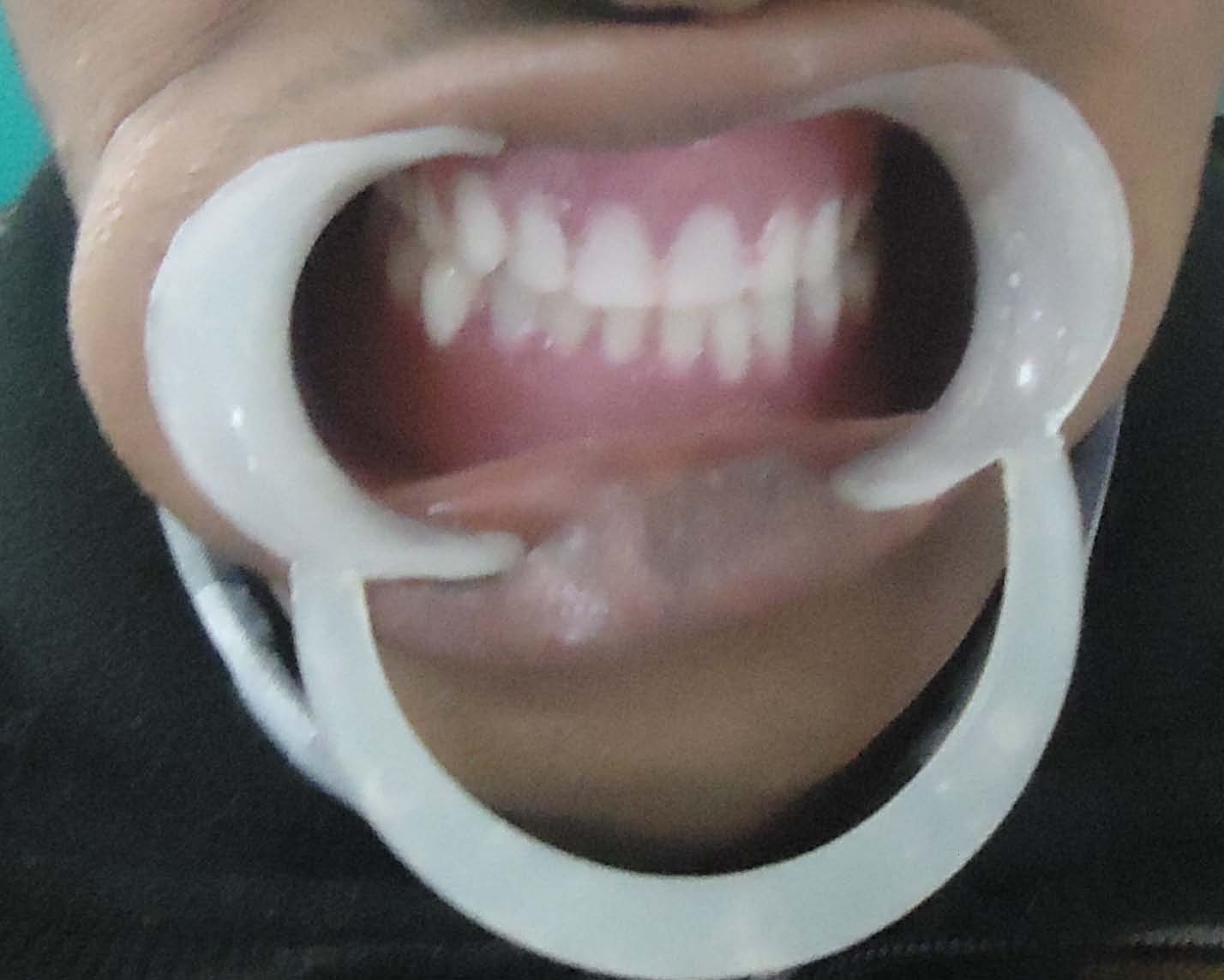
Two brothers, 20-year-old and 25-years-old reported to the Department of Oral Medicine and Radiology, Institute of Dental Sciences, Bareilly, UP, India, with a chief complaint of missing teeth in upper and lower jaw region since childhood. History of present illness revealed that teeth were congenitally missing. They had also difficulty in chewing food and speech. They were intolerable to hot climate and hot water with a history of reduced sweating. Parental history revealed that there were no other cases of ED in their family. Past dental and medical history were not significant. Extra-oral examination [Table/Fig-1] revealed there were scarce eyebrows and eyelashes,thinning of scalp hair, frontal bossing, prominent supraorbital ridges, depressed nasal bridge, thick and prominent lips with a concave profile. There was mid face hypoplasia with reduced facial height. Perioral, periorbital and perinasal pigmentation were also present on lower lip. Skin was dry and wrinkled with no nail dystrophy. Intraoral examination [Table/Fig-2] revealed the presence of peg shaped 11, 21 and all the remaining teeth were clinically missing in younger brother while in elder there was presence of 11, 21, 22, 12 [Table/Fig-3]. The edentulous ridge was thin and atrophic with decreased height and loss of sulcus depth in maxillary and mandibular arches. Tongue was relatively large with atrophic glossitis. The palate was shallow, oral mucosa was normal and dry due to less saliva. On the basis of history and clinical examination, a provisional diagnosis of hypohidrotic ED was given, as there was triad of symptoms present, that is hypotrichosis, hypohidrosis and oligodontia was present. Orthopantomograph [Table/Fig-4] revealed the presence of peg shaped 11, 21 in younger brother while in elder one 11,21,12,22 were present. There was reduction in the height of alveolar crest in maxillary and mandibular arches. Lateral cephalogram revealed the Class III relationship of maxillary and mandibular arches. Since, clinical findings suggest the presence of ED, a final diagnosis of hypohidrotic ED was given. Patients were advised frequent sipping of water, emollients for dry skin and to wear cool clothing. In the treatment, they were advised for the implant supported over denture [Table/Fig-5] and to maintain cool and ambient temperature.
Facial view of the first patient

Intraoral view of the upper jaw of the first patient

Intraoral view of the upper jaw of the second patient

Orthopantomogram of the first patient

Postoperative view of the first patient
Discussion
The incidence of ED is 1:100,000, with a mortality rate of 28% in males up to three years of age [1]. ED is a genetic disorder that has congenital birth defects of two or more ectodermal structures [2]. It might be inherited in any form of several genetic patterns including autosomal-dominant, autosomal-recessive and X-linked modes [3]. Hypohidrotic ectodermal dysplasia (HED) is an X-linked condition and is the most common form of ED. In this type of syndrome, there are no sweat glands or they are significantly decreased. HED (Christ-Siemens-Touraine syndrome) has characteristic triad of reduction in the amount of hair (hypotrichosis), absence of sebaceous glands (asteatosis) and absence of sweat glands (anhidrosis) [4]. ED represents a large and complex group of diseases comprising more than 170 different clinical conditions [5]. Affected males have agenesis of primary and permanent teeth, whereas, heterozygous females have agenesis of permanent teeth [6]. Normal and psychological development of young patients dictates that they look and feel as normal as possible. Therefore, dental appearance in these patients is extremely important because it can affect their self-esteem. Prosthodontic treatment of these patients include fixed, removable or implant supported prosthesis [7].
There are two major types of this condition depending on the number and functionality of the sweat glands: (1) X-linked anhidrotic or hypohidrotic, where sweat glands are either absent or significantly reduced in number (Christ-Siemens- Touraine syndrome, (2) hidrotic, where sweat glands are normal and the condition is inherited as 274autosomal dominant (Clouston’s syndrome) [1-4]. Hypohidrotic ED is the most common kind of ED encountered by dentists, as multiple missing teeth is the striking feature of the disease, which is true in both of our patients. The X-linked recessive HED has full expression in males. Female carriers are more than affected men, but they have little or no signs of the condition and their clinical identification is difficult [6]. Both of our patients were males,this confirms the fact that the disease is being x-linked so it is more common in males than in females.The conical and pointed teeth are key features of the syndrome and may be the only obvious abnormality. In both the cases, there were multiple missing teeth and had conical shaped teeth, which is again a pathognomic feature of ED. These findings coincide with the cases reported by Hickey et al., Mokhtari et al., Viera et al., [3-5]. As a result of oligodontia, both the patients had edentulous ridge, which was thin and atrophic with decreased height and loss of sulcus depth in maxillary and mandibular arches, which proves the fact that alveolar process fails to develop in absence of teeth. Because of their severely diminished ability to sweat, patients with HED have a propensity to develop hyperthermia with physical exertion or exposure to a warm environment, and affected infants often present with recurrent high fevers. The scalp hair, eyebrows, and eyelashes are sparse, fine, and often lightly pigmented. In both the patients, there were scanty and sparse hairs indicating hypertrichosis to be one of the most common clinical feature to be encountered in ED patients as reported by Agarwal et al., and Hickey et al., [3-8]. HED patients have a characteristic facies with frontal bossing, a saddle nose and full, everted lips. Both of our patients had similar facial appearance with dry, scaly skin and history of reduced sweating. Abnormal mucous glands result in extremely thick nasal secretions and a propensity to develop respiratory tract infections [8]. These findings contrast with our cases, as there was absence of thick nasal secretions and there was no history of respiratory tract infections. In cases where the salivary glands are hypoplastic or absent, varying degrees of xerostomia are expected [9]. In both the patients oral mucosa was dry due to less saliva with large tongue. Orthopantomogram at an early age to rule out hypodontia and other dental abnormalities [10]. The clinical diagnosis is based on clinical and radiological manifestations such as the number and distribution of sweat pores, the amount of sweat produced, the structural and biochemical characteristics of hair, skin biopsy, and characteristics of lacrimal secretions [11]. In both of our cases, the diagnosis made on clinical findings suggest the presence of ED.Histopathology shows flattened epidermis, reduced number of sebaceous glands and hair follicles [2]. The management of children and adults with HED is a challenge because of their heat intolerance and because of their susceptibility to pulmonary infections. During hot weather, affected individuals must have access to an adequate supply of water and a cool environment, which may mean “cooling vests,” air conditioning, a wet T-shirt, and/or a spray bottle of water[12].In both the cases implant supported overdenture, emollients for dry skin,frequent sipping of water was advised and patient was asked to maintain cool and ambient temperature.
Conclusion
Dentists are often the first who diagnose these patients. Therefore, they should be aware of the clinical manifestations of this syndrome. This will be helpful in proper diagnosis, early interventions and appropriate therapies for these patients.
[1]. Jh Nunn, NE Carter, TJ Gillgrass, RS Hobson, NJ Jepson, JG Meechan, The interdisciplinary management of hypodontia: background and role of paediatric dentistryBr Dent J 2003 194:245-51. [Google Scholar]
[2]. H Lesot, F Clauss, MC Manière, M Schmittbuhl, Consequences of X-linked hypohidrotic ectodermal dysplasia for the human jaw boneFront Oral Biol 2009 13:93-9. [Google Scholar]
[3]. Aj Hickey, Jr Vergo TJ, Prosthetic treatments for patients with ectodermal dysplasiaJ Prosthet Dent 2001 86:364-8. [Google Scholar]
[4]. S Mokhtari, S Mokhtari, A Lotfi, Christ-siemens-touraine syndrome: a case report and review of the literature.Case Rep Dent 2012 [Google Scholar]
[5]. KA Vieira, MS Teixeira, CG Guirado, MB Gavião, Prosthodontic treatment of hypohidrotic ectodermal dysplasia with complete anodontia: case report.Quintessence Int 2007 38:75-80. [Google Scholar]
[6]. Mo Lexner, A Bardow, JM Hertz, LA Nielsen, S Kreiborg, Anomalies of tooth formation in hypohidrotic ectodermal dysplasia.Int J Paediatr Dent 2007 17:10-8. [Google Scholar]
[7]. MA Pigno, RB Blackman, Jr Cronin RJ, E Cavazos, Prosthodontic management of ectodermal dysplasia: a review of the literature.J Prosthet Dent 1996 76:541-5. [Google Scholar]
[8]. S Agarwal, S Gupta, Hypohidrotic ectodermal dysplasiaIndian Dermatol Online J 2012 3:125-27. [Google Scholar]
[9]. L Lo Muzio, P Bucci, F Carile, F Riccitiello, C Scotti, E Coccia, Prosthetic rehabilitation of a child affected from anhydrotic ectodermal dysplasia: a case reportJ Contemp Dent Pract 2005 6:120-6. [Google Scholar]
[10]. FS Ryan, C Mason, JI Harper, Ectodermal dysplasia--an unusual dental presentation.J Clin Pediatr Dent 2005 30:55-7. [Google Scholar]
[11]. M Bani, AM Tezkirecioglu, N Akal, T Tuzuner, Ectodermal dysplasia with anodontia: a report of two casesEur J Dent 2010 4:215-22. [Google Scholar]
[12]. GL Brengelmann, PR Freund, LB Rowell, JE Olerud, KK Kraning, Absence of active cutaneous vasodilation associated with congenital absence of sweat glands in humansAm J Physiol 1981 240:H571-5. [Google Scholar]