Massive Recurrent Chondroblastic Osteosarcoma of Maxilla: A Rare Case Report
Dwarkadas Adwani1, Anirudh Bhattacharya2, Nitin Adwani3, Rinku Adwani4, Vijay W Sharma5
1Professor & Head, Department of Oral & Maxillofacial Surgery,VYWS Dental College & HospitalAmravati, Maharashtra, India.
2Post Graduate Student, Department of Oral & Maxillofacial Surgery,VYWS Dental College & Hospital, Amravati, Maharashtra, India.
3Sr. Lecturer, Department of Oral & Maxillofacial Surgery,VYWS Dental College & Hospital, Amravati, Maharashtra, India.
4Sr. Lecturer, Department of Orthodontics,VYWS Dental College & Hospital, Amravati, Maharashtra, India.
5Post Graduate Student, Department of Oral & Maxillofacial Surgery,VYWS Dental College & Hospital, Amravati, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anirudh Bhattacharya, Adwani Hospital, Ambapeth, Amravati, Maharashtra- 444601, India.
Phone: +91- 8390103969,
E-mail: dranirudhb@gmail.com
The jaw bones are particularly difficult to manage because of their proximity to important structures and later limited options in the rehabilitation of their form and functional factors. This stands true especially in cases of maxilla as being situated in a very peculiar anatomic location, comprising of the skull base and its related structures, any radical treatment is deferred. In order to retain the maximum form and function as later there are few reconstruction options available for maxilla the trend always goes in favour of least morbid treatment option whether being surgery, chemotherapy or radiation therapy. Moreover in maxilla the anatomic complexities makes it very difficult to get wide and clear surgical margins which again accounts for a poor prognostic rate. Recurrences are common in osteosarcomas of maxilla and the line of treatment for recurrence is still a matter of research.
Osteosarcoma, Maxillectomy, Cisplatin, Central jaw tumour
Case Report
A 17-year-old male patient reported to our hospital complaining of painless swelling over right side of his face which was gradually increasing from past two months. The patient was apparently alright two months ago after which he suddenly noticed a small swelling inside his mouth over the right side of hard palate. The swelling was not associated with any kind of pain or discomfort. The swelling gradually increased to attain the present size and the patient did not report this to any medical centre for treatment. The patient had some difficulty in mastication and deglutition due to the enlarging mass inside his mouth. He also complained of weight loss and anorexia. His medical and personal history was non-contributory. On general examination he was moderately built with all normal vital statistics and no other obvious physical or mental abnormalities.No cervical lymphadenopathy was discernible following the bilateral palpation of neck. Physical examination of the intraoral swelling revealed a firm, non-tender and sessile lesion of size ~ 4x4 cms. attached to hard palate extending mediolaterally from marginal gingiva of right maxillary lateral incisor till the ipsilateral last present molar, covering the whole of hard palate and reaching upto the left maxillary canine tooth. Antero-posteriorly it extended from the palatal gingiva of maxillary anterior teeth till the junction of hard and soft palate. The surface of the swelling was irregular and covered with a slough [Table/Fig-1]. No dental problems relating to teeth were noticed. Chest X-ray, routine blood investigations and ultrasonography results of abdomen and neck were normal.The patient’s ELISA for HIV and VDRL were negative. A homogenous mass was appreciable obliterating the whole of right maxillary sinus in PNS Waters view radiograph [Table/Fig-2]. The CT appearance was of a mass of mixed radiopacity with a predominant soft tissue component, central calcification/ossification and destruction of the structures involved. Coronal section revealed a large soft tissue density lesion with its epicentre in the maxilla, causing destruction of the anterior, anterolateral and posteriolateral walls of the maxillary sinus, extending upto the inferior orbital rim, inferiorly causing destruction of the hard palate and alveolar processes of the right maxilla in the molar region. Radiographic findings were in favour of malignant tumor of maxilla or maxillary sinus. Scrapings taken from the involved region to rule out fungal granulomas did not show any fungi. A punch biopsy of the lesion was taken from the most dependent site and the histopathology report stated a well developed cartilaginous matrix which was arranged in lobules. Typical neoplastic osteoblasts were surrounding the osteoid and immature bone intermixed with neoplastic cartilaginous tissue was also seen. The tumorcells in the central portions had atypical nuclei and lacunar cytoplasm. The peripheral portions were richly cellular and composed predominantly of pleomorphic, spindle-shaped cells. The bulk of bone formation was occurring by endochondral ossification, small amount of osteoid like material was apparently seen in part of the peripheral portion of the lesion. It confirmed the diagnosis of osteosarcoma of maxilla.
The clinical differential diagnosis included the most common malignancies in the oral cavity such as squamous cell carcinoma (SCC), fibro-osseous lesion, minor salivary gland tumor, giant cell tumor, lymphoma and carcinoma of the sino-nasal tract.
On the basis of histopathological diagnosis, surgical planning was done and the patient underwent partial maxillectomy [Table/Fig-3]. Postoperative histopathological diagnosis of the specimen was confirmative of chondroblastic osteosarcoma and the surgical margins were negative for the tumour cells in gross as well as microscopic examination. The nearest margin of the resection to tumour was three millimetres away [Table/Fig-4]. External beam radiation therapy was adviced at 60grays, 5 days/week for 6 weeks.
After one month of radiotherapy, the patient reported with a painful swelling in the operated area with difficulty in oral feeding and chemosis. On clinical examination, a massive recurrent lesion at the operated site was noted intra orally but still patient had no evidence of lungs or liver metastasis [Table/Fig-5]. Treatment plan consisted of chemotherapy (Cisplatin 100 mg/m2 D1 and doxorubicin 25 mg/ m2, D1-D2-D3, 6 cycles every 3 weeks), because the lesion was locally advanced and thus inoperable. Following the chemotherapy, there was an improvement in his symptoms but no regression of the lesion was noted [Table/Fig-6]. The patient refused further radiotherapy and succumbed to the disease in 2 months.
Surface of the swelling was irregular and covered with a slough

Homogenous mass was appreciable obliterating the whole of right maxillary sinus in PNS Waters view radiograph

Specimen showing partial maxilectomy

Showing the resection margin of tumour
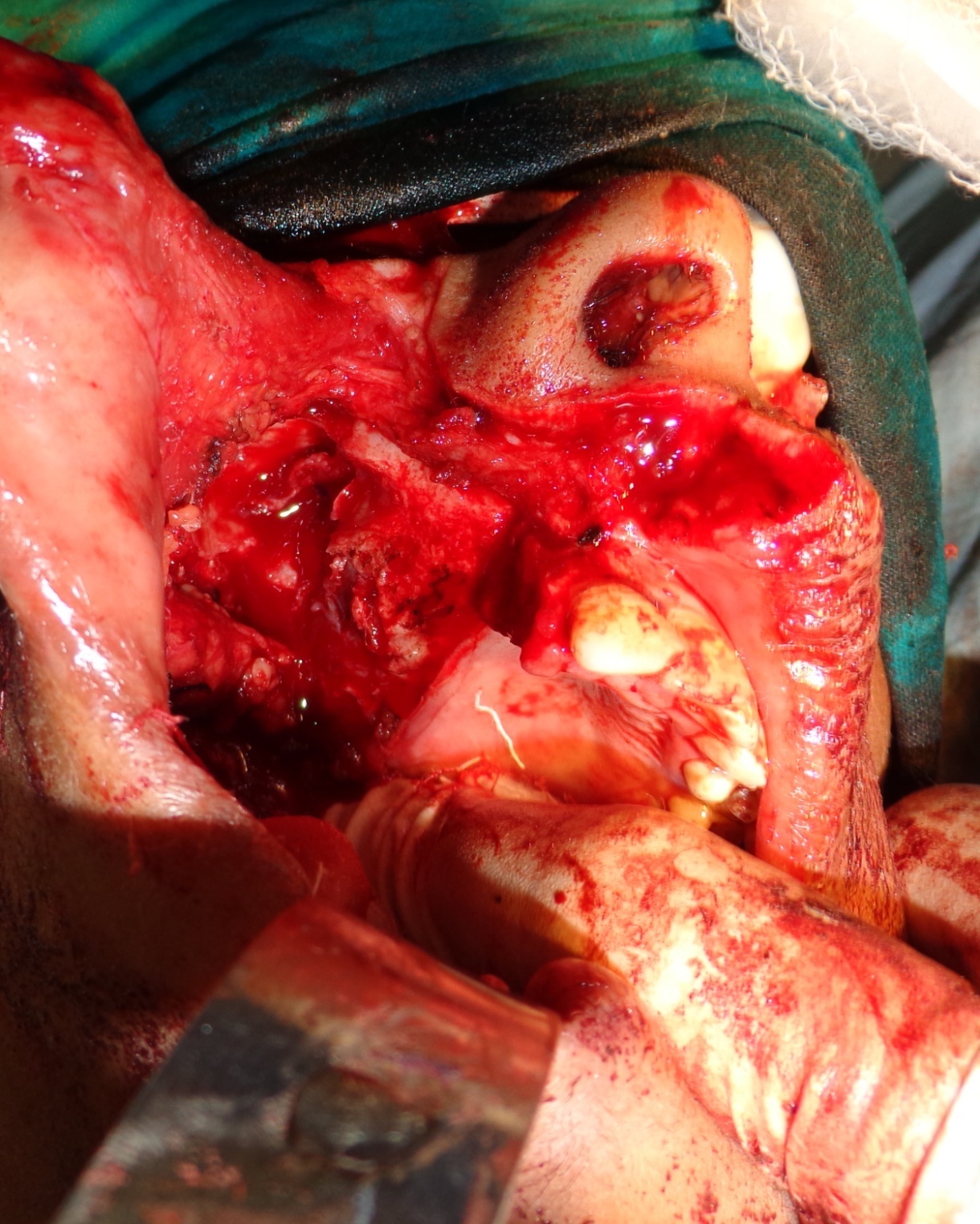
Post-operative view of the patient

No regression of the lesion was noted past-operatively following chemotherapy

Discussion
Osteosarcoma of the craniofacial region is a relatively rare disease [1]. The mandible is usually reported as the most common site of involvement [2] The average age at the onset of osteosarcoma of the maxillofacial region is found in the third to fourth decade of life [3,4,5–7]. While a slight male predominance is reported [1]. The histologic types are chondroblastic (41%), osteoblastic (33%) and fibroblastic (26%) [1,2,5]. In our subject the site was maxilla which has a very low incidence of occurrence and also is less reported in literature. The presentation in maxilla is usually late due to the behavior of the tumor which invades the structures cranially rather caudally [4]. The patient seeks medical advice when the lesions start enlarging to such an extent that it becomes much evident inside the oral cavity or causes a disruption in mastication or deglutition. Obtaining a clear surgical margin is an established good prognostic factor, but in such cases of maxilla it becomes virtually impossible to retain such healthy margins along with tumor specimen while resecting. The deep invasion of tumor encasing some of the vital structures further makes the situation worse [7-8]. Maxilla being a more of cancellous bone is porous in nature and the evasion of tumor cells is comparatively easier than that of mandible. This again limits the prognostic value of resection majorly in cases of partial or subtotal maxillectomies were there are always chances of few tumor cells infiltrating the remaining part of maxilla. The surgery is stated to be the gold standard for such large tumors but such tumors presenting in maxilla are a challenge for the surgeon keeping in mind the oncologic safety, maintenance of form and function and creating minimum post operative morbidity [8-10]. Adjuvant therapies like chemotherapy and radiation have showed some effect on the management of such tumors but they still cannot be termed as curative therapies alone.
As of now the surgical treatment is the only primary treatment option for such massive lesions but in cases of recurrence it becomes practically impossible to manage the recurrent lesion and reduce the mortality.
Conclusion
Osteosarcoma of maxilla being aggressive in nature must be planned and treated immediately at the first onset of symptoms. Delay in the management leads to the lesion acquiring an un-operable size which will lead to increased mortality. It is therefore suggested to treat such cases at the earliest with surgery obtaining wide and clear surgical margins to have a better outcome followed by adjuvant therapies. Regular screening and follow up is highly recommended and must be diligently enforced in all centres.
[1]. Sheikh Soheyl, Pallagatti Shambulingappa, Aggarwal Amit, Gupta Deepak, Osteosarcoma of maxilla: A case reportJ Clin Exp Dent 2010 2(3):117-20. [Google Scholar]
[2]. AJ Ajura, SH Lau, A retrospective clinicopathological study of 59 osteogenic sarcoma of jaw bone archived in a stomatology unitMalaysian J Pathol 2010 32(1):27-34. [Google Scholar]
[3]. Pellitteri Phillip K, AlfioFerlito Bradley Patrick J, Shahad Ashok R, Management of sarcomas of the head and neck in adults.Oral Oncology 2003 39:2-12. [Google Scholar]
[4]. M August, P Magennis, D Dewitt, Osteogenic sarcoma of the jaws: factors influencing prognosisInt. J. Oral Maxillofac. Surg 1997 26:198-204. [Google Scholar]
[5]. R Fernandes, NG Nikitakis, A Pazoki, RA Ord, Osteogenic Sarcoma of the Jaws: A 10 year experience.Joral Maxillofac Surg 2007 65:1286-91. [Google Scholar]
[6]. MO Ogunlewe, OF Ajayi, WL Adeyemo, AL Ladeinde, O James, Osteogenic sarcoma of the jaw bones: A single institution experience over a 21-year period.Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 101:76-81. [Google Scholar]
[7]. Okinaka Yoshihiko, Takahashi Masahiro, Osteosarcoma of the maxilla: Report of a case and review of the literature concerning metastasis.J Oral Maxillofac Surg 1997 55:1177-81. [Google Scholar]
[8]. MJ Klein, GP Siegal, Osteosarcoma: anatomic and histologic variantsAm J Clin Pathol. 2006 125(4):555-81. [Google Scholar]
[9]. Cavalcanti MGP, AR uprechtand, Yang J, Radiological fndings in an unusual osteosarcoma in the maxilla:Dentomaxillofacial Radiology 2000 29:180-4. [Google Scholar]
[10]. Klein Michael J, Siegal Gene P, Anatomic and histologic variants.Am J Clin Pathol. 2006 125:555-81. [Google Scholar]