Comparison of The Effect of Implant Abutment Surface Modifications on Retention of Implant-Supported Restoration with A Polymer Based Cement
Nabaprakash Sahu1, Namratha Lakshmi2, N.S. Azhagarasan3, Yoshaskam Agnihotri4, Manoj Rajan5, Ramasubramanian Hariharan6
1 Assistant Professor, Department of Prosthodontics, HiTech Dental College & Hospital, Bhubaneswar, India.
2 Assistant Professor, Department of Prosthodontics, HiTech Dental College & Hospital, Bhubaneswar, India.
3 Professor & Head, Department of Prosthodontics, Ragas dental College & Hospital, Chennai, India.
4 Assistant Professor, Department of Conservative dentistry & Endodontics, HiTech Dental College & Hospital, Bhubaneswar, India.
5 Professor, Department of Prosthodontics, Ragas dental college & Hospital, Chennai, India.
6 Assistant Professor, Department of Prosthodontics, Ragas Dental College & Hospital, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Yoshaskam Agnihotri, Flat no 508, Harihar enclave, Gautam Nagar, Bhubaneswar-751014, Odisha, India.
Phone: 9692119999,
E-mail: docagnihotri@gmail.com, docagnihotri@yahoo.com
Background: In cement-retained implant-supported restoration it is important to gain adequate retention of definitive restoration as well as retrievability of prosthesis. The surface of the abutment, alloy of the restoration and the type of cement used influences the retention of the restoration. There is a need to analyze the influence of surface modifications of abutments on the retentive capabilities of provisional implant cements.
Purpose of study: To compare the effect of implant abutment surface modifications on retention of implant-supported restoration cemented with polymer based cement.
Materials and method: Thirty solid titanium implant abutments (ADIN), 8mm height, were divided into 3 groups. Ten abutments with retentive grooves (Group I) as supplied by the manufacturer, Ten abutments milled to 20 taper circumferentially (Group II), and Ten abutments milled and air-abraded with 110 μm aluminum oxide (Group III) were used in this study. Ni-Cr coping were casted for each abutment and polymer based cement was used to secure them to the respective abutments. Using a universal testing machine at a crosshead speed of 0.5 cm/minute, tensile bond strength was recorded (N).
Results: Mean tensile bond strength of Group I, II and III were found to be 408.3, 159.9 and 743.8 Newton respectively. The values were statistically different from each other (p<0.001).
Conclusion: Abutments with milled and sandblasted surface provide the highest retention followed by abutments with retentive grooves and then by abutments with milled surface when cast copings were cemented to implant abutments with polymer based cement.
Clinical implications: Retention of restoration depends on the surface of the abutment as well as the luting agents used. Incorporation of retentive grooves or particle abrasion can enhance retention especially in situation of short clinical crown.
Implant abutment surface, Implant supported restoration, Abutment surface modification
Introduction
The selection of mode of retention of implant-supported fixed prostheses is influenced by the passivity of the framework, interarch space, occlusion, esthetics and retrievability of prosthesis. Retrievability of the prosthesis is essential for periodic replacement of prosthodontic components, loosening or fracture of the fastening screws, fracture of abutments, modification of the prosthesis after loss of an implant, and for surgical re-intervention [1]. Screw retention in implant-supported prostheses was developed in response to the need for retrievability of the prosthesis [2,3]. But it has the disadvantages of compromise in esthetics due to the visibility of the screw access hole and difficulty in establishing ideal occlusal contacts as the screw access hole occupies at least 50% of the occlusal table [4]. On the contrary, cement-retained prostheses have superior occlusion, esthetics, passivity [5], and loading characteristics [1] but are difficult to retrieve.
It is well-documented in the dental literature that several factors like taper, surface area and height, surface finish and roughness [6–8] influence the amount of retention in cement-retained restorations, whether they exist on natural teeth or implant abutments. An increase in surface roughness of prepared teeth will result in an increase in retention of cemented casting due to mechanical interlocking of the cementing medium with the roughened tooth surface [7,8]. Similarly the surface modification on implant abutment can increase the retention of the cement-retained implant-supported cast coping [9]. Different implant abutment surface modifications namely air-borne particle abrasion [10,11] with diamond rotary cutting instrument [10] retentive grooves [12,13] have been advocated to enhance the retention of cement-retained implant-supported cast copings.
The choice of cement is one of the most important factors controlling the amount of retention attained [14–20]. Selection of cement that is too retentive could lead to damage to implant, implant abutment, abutment screw and the prosthesis if an aggressive removal technique is used. The selection of cement that is not retentive enough could be a potential source of failure of retention of the restoration [19]. The definitive cements such as resin composite, zinc phosphate, zinc polycarboxylate, glass-ionomer and resin modified glass-inomer increase retention, provide good marginal seal and significantly enhance the cement failure loads of the prosthesis luted to titanium abutments in comparison to provisional luting agents [1,20,21]. But retrievability is more difficult when definite cements are used. For ease of retrievability, the literature reports suggested the use of provisional cements [22–24] such as zinc-oxide eugenol, non-eugenol zinc-oxide. But the problems encountered are inadequate retention to resist functional force, [11] cement washout and mobility of restoration [25].
The use of resin based provisional cement for luting definitive restoration on implant abutment are well documented [16,19,22,26].
Since the polyurethane and resin base provisional luting cements luting agents are typically stable intraorally, the cement gap and the tensile bond strength of these luting agents would change less over time [24,27]. So the newer polymer based resin cements could satisfy the requirements of adequate retention to resist functional force, marginal seal and also retrievability of the suprastructure.
Therefore the purpose of this study was to evaluate and compare the effect of abutment surface modification on the retention of implant-supported restoration with polymer based cement.
Materials and Methods
Thirty clear autopolymerising acrylic blocks of approximately 20 x 20 x 20mm were fabricated with an implant analog in the centre of the block with the help of a custom-made silicone mold and surveyor.
Thirty implant abutments, 8mm in height with five retentive grooves of 100μm in depth and (ADIN Dental Implant System Ltd., Israel), thirty implant analogs (ADIN Dental Implant System Ltd., Israel) were used. In this study the abutments were divided into three groups (I, II, III) with 10 abutments each. In Group I, abutments with grooves as obtained from the manufacturer were used. In Group II, abutments were milled with 20 taper circumferentially to obtained smooth surface to mimic a clinical situation. In Group III, abutments were milled in a similar manner and then sandblasted with 110μm size alumina till the prepared finish line. The implant abutments were screwed to the implant analogs [Table/Fig-1] to a torque of 35 Ncm with a Torque Ratchet (ADIN Dental Implant System Ltd., Israel).
Implant abutment with retentive grooves (Group I), Milled implant abutment (Group II) and Milled and sandblasted implant abutment (Group III)

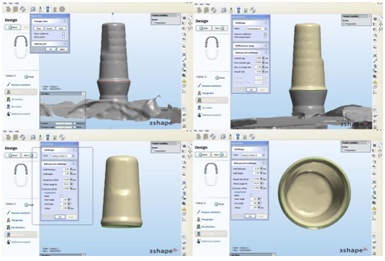
Impression of the implant abutment was made using one stage putty wash impression technique using putty and light body consistency polyvinyl siloxane impression material (Coltene Whaledent, United State). The die of implant abutment was poured with Type-IV dental stone (Ultrarock, Kalabhai, Mumbai, India). The dies were scanned using a D700 scanner (3Shape Dental System, Copenhagen K, Denmark). The scanner employs a unique 2 camera and 3-axis motion system. The 3-axis allows the object to be tilted, rotated and translated so as to be scanned from any viewpoint, making 3-axis the optimal number of axis for a scanning a dental model. The system’s powerful algorithms automatically detect the margin line. The copings were designed virtually using software (CAM Bridge software). They were designed with a thickness of 0.3mm after creating a space of 25 microns for the luting cement [Table/Fig-2]. The designed copings were printed epoxy resin using 3D printer (Polyjet HD3000 for 3D Printing) [Table/Fig-3].
Scanned die on computer screen, Designed coping on scanned die, outer view of designed coping and Inner view of designed coping
Printed resin coping on die

A wax loop was made with a preformed wax sprue former of 2.5mm diameter (Bego, Germany) and attached on top of each resin coping. The 30 resin patterns with wax loop were invested in phosphate-bonded investment (Belasun, Bego, Germany) and casting with Nickel-chromium alloy (Bellabond Plus, Bego, Germany). The divested castings were sandblasted, cleaned and carefully seated on the respective abutments to check for a passive fit [Table/Fig-4]. Intaglio surface were sandblasted with 110μm alumina. The casted copings were then cemented to the respective abutments of three groups using the polymeric implant cement (Implacem, Equinox Medical Technologies B.V. Holland). The cement was auto-mixed and dispensed onto the intaglio surface of the cast coping and a load of 2 kg was applied for a period of 10 minutes using a custom-made acrylic resin table attached to the surveying arm of the dental surveyor (Bego, Germany) [Table/Fig-5]. The test samples of each group were kept in distilled water (Metro Lab, Pondicherry, India) for 48 hours at room temperature for aging. The copings were pulled from the abutment with a 500kg load cell in the universal testing machine (Lloyd instruments, Farnham, U.K.) at a crosshead speed of 5mm/min, until the coping debonded from the abutment [Table/Fig-6]. The tensile bond strength of polymer based cement was recorded in Newton.
Casted coping on implant abutment

Cementation of cast coping to implant abutment

Testing of sample in Universal Testing Machine

Results
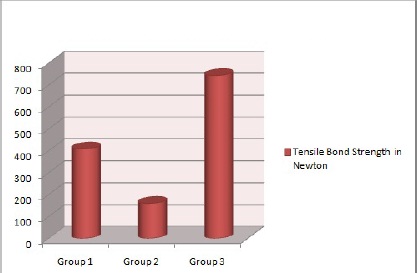
The tensile bond strength as recorded from the universal testing machine was tabulated and the mean value obtained [Table/Fig-7 and 8]. The values obtained were analyzed using ONE-WAY analysis of variance (ANOVA) and Tukey-HSD procedure. Castings cemented with polymeric implant cement on abutments with milled and sandblasted surface had the highest mean tensile bond strength (743.8 Newton), followed by abutments with retentive grooves (408.3 Newton) and milled abutments (159.9 Newton). The results of one-way ANOVA indicated that significant interaction existed between surface condition and provisional polymeric implant luting agent (p < 0.001).
Comparison of mean tensile bond strength of three test groups (I, II & III) by One-way ANOVA
| Groups | Mean ± S.D. | Overall p-value* |
|---|
| I | 408.3 ± 48.3 | <0.001* |
| II | 159.9 ± 37.0 |
| III | 743.8 ± 62.4 |
| *Denotes statistical significance at 1% level |
Comparison of mean tensile bond strength of test groups (I, II & III) in Newton
Discussion
The factors like abutment configuration and height of the abutment are determined by the particular clinical situation and cannot be changed as per the clinician’s choice. Whereas, the alloy used for the prosthesis [18,21], type of cement and the surface modifications of the abutment are factors that can be easily altered to influence the amount of retention required.
The vast number of luting cements available for cementation makes it a factor that can be altered with ease to improve retention. Numerous studies have been carried out to test the retention offered by various cements available in the market [15,17,18,22,27]. Literature shows the use of both provisional cements and definitive cements for the cementation of implant supported fixed prosthesis [10,17–19,24]. Controversy exists as to whether a provisional or permanent luting cements should be used for cementing implant prosthesis [26]. Various authors have suggested the use of provisional cements for cementation of cement-retained implant-supported restoration in order to achieve crown retrievability based on assumption that provisional cements are less retentive than permanent cements [22,24].
Study on leakage of various types of luting agents and conclude that the zinc oxide-eugenol cement showed increased leakage with time. Ramp et al., [24] evaluated three resin, one polyurethane, and two eugenol-containing provisional luting agents and reported that the eugenol-containing luting agents were most soluble in oral fluids. Therefore the problems encountered with provisional cements are insufficient to resist functional force [11] and cement washout [25] at the margin of the abutment/crown interface resulting in marginal leakage and bacterial proliferation jeopardizing the health of the soft tissue and the implant/tissue interface [24].
The stability of polyurethane and resin cements and the ability of resin based provisional cements to achieve good bond strength with metallic abutments [24] makes them a good choice for cementing medium.
The bond strength obtained in this study for milled samples (159.9 Newton) was similar to bond strength with resin cements to smooth surface implant abutment reported by Sheets et al., [19]. The bond strength obtained in this study for the unaltered abutment samples with retentive grooves was 408.3 Newton. This could be attributed to the mechanical retention on abutment by means of horizontal retentive grooves. The higher values obtained for samples with retentive grooves are similar to those reported by Maydan L et al., [12]. This value is also comparable to Ultra Temp, temporary polycarboxylate cements (regular set) cemented on smooth surface abutment reported by Sheets et al., [19].
The bond strength obtained for the milled and sandblasted with 110 μm aluminum oxide (743.8 Newton) is comparable to permanent luting Panavia (resin cement) bonding to natural tooth [6]. This could be due to increase in surface area, which helps micromechanical bonding of the cement and thus increasing retention.
Samples of all three groups had bond failures occurring at the interface of cement and the abutment, although there was cohesive failure in cement. Even in the sandblasted group, the cement was retained in the coping. The reason for this could not be explained since the intaglio surface of the crown was also blasted with 110 μm alumina. The difference in bond strength of the cement to titanium and base metal alloy need to be studied to understand this failure. The finding in this study is contrary to that found by Lorey HYPERLINK “http://www.ncbi.nlm.nih.gov/pubmed?term=%22Lorey%20RE%22%5BAuthor%5D&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel. Pubmed_RVAbstract” RE et al., [28] where titanium exhibited better bonding than nickel-chromium to resin cements.
Considering the advantages obtained by surface modification of abutment, the temporary cement itself can be used for luting purpose and retention comparable to GIC and resin cements can be achieved. In addition, retention achieved with sandblasting will be of use in clinical situations when abutment height is to be reduced.
Since there are no criteria for minimum amount of force required to prevent easy dislodgement of crowns, the choice of cements or abutment surface modifications to improve the retention is based on clinician choice.
Limitations
In our study, the sample size taken was small, so a further study with a larger sample would provide better results. Furthermore, studies on transmission of force to abutment screw, implant, and implant-bone junction during intact retrieval of cement-retained crown are lacking. Therefore the minimum retentive force required to prevent dislodgement as well as for easy retrievability without damaging the implant components and osseointegration need to be explored.
Conclusion
The tensile bond strength of polymer based cement obtained with milled and sandblasted implant abutment surface shows the highest bond strength followed by those with retentive grooves on implant abutment and then by smooth surfaced milled abutments.
[1]. Michalakis KX, Hirayama H, Garefis PD, Cement-retained versus screw-retained implant restorations: A critical reviewInt J Oral Maxillofac Implants 2003 18:719-28. [Google Scholar]
[2]. Mehl C, Harder S, Wolfart M, Kem M, Wolfart S, Retrievability of implant-retained crowns following cementationClic Oral Implants Res 2008 19(12):1304-11. [Google Scholar]
[3]. Da Rocha PV, Freitas Ma, de Morais Alves da Cunha T, Influence of screw access on the retention of cement-retained implant prosthesisJ Prosthet Dent 2013 109(4):264-8. [Google Scholar]
[4]. Hebel KS, Gajjar RC, Cement-retained versus screw-retained implant restorations: Achieving optimal occlusion and esthetics in implant dentistryJ Prosthet Dent 1997 77:28-35. [Google Scholar]
[5]. Lee MY, Heo SJ, Park EJ, Park JM, Comparative study on stress distribution around internal tapered connection implants according to fit of cement- and screw-retained prosthesesJ Adv Prosthodont 2013 5(3):312-8. [Google Scholar]
[6]. Zidan O, Fergusson GC, The retention of complete crowns prepared with three different tapers and luted with four different cementsJ Prosthet Dent 2003 89:565-71. [Google Scholar]
[7]. Ayad MF, Rosenstiel SF, Salama M, Influence of tooth surface roughness and type of cement on retention of complete cast crownsJ Prosthet Dent 1997 77:116-121. [Google Scholar]
[8]. Felton DA, Kanoy BE, White JT, The effect of surface roughness of crown preparations on retention of cemented castingsJ Prosthet Dent 1987 58:292-96. [Google Scholar]
[9]. Kaufman EG, Coelho DH, Colin L, Factors influencing the retention of cemented gold castingsJ Prosthet Dent 1961 11:487-502. [Google Scholar]
[10]. Kim Y, Yamashita J, Shotwell JL, Chong K, Wang H, The comparison of provisional luting agents and abutment surface roughness on retention of provisional implant-supported crownsJ Prosthet Dent 2006 95:450-55. [Google Scholar]
[11]. Michalakis K, Pissiotis AL, Kang K, Hirayama H, Garefis PD, Petridis H, The effects of thermal cycling and air abrasion on cement failure loads of 4 provisional luting agents used for the cementation of implant-supported fixed partial denturesInt J Oral Maxillofac implants 2007 22:569-74. [Google Scholar]
[12]. Maydan L, Lewinstein I, Lehr Z. Effect of Circumferential Grooves on Retention of Implant-Cemented Crowns. Implantology Research, Scientific Program, 27 August 2004 Crowne Plaza Hotel AVSA I [Google Scholar]
[13]. Lewinstein I, Block L, Lehr Z, Ormianer Z, Matalon S, An in vitro assessment of circumferential grooves on the retention of cement-retrained implant-supported crownsJ Prosthet Dent 2011 106(6):367-72. [Google Scholar]
[14]. Bernal G, Okamura M, Munoz CA, The effect of abutment taper, length and cement type on resistance to dislodgement of cement-retained, implant-supported restorationsJ Prosthodont 2003 12:111-15. [Google Scholar]
[15]. Covey DA, Kent DK, Henry A, St. Germain Jr, Koka S, Effects of abutment size and luting cement type on the uniaxial retention force of implant-supported crownsJ Prosthet Dent 2000 83:344-48. [Google Scholar]
[16]. Dixon DL, Breeding LC, Lilly KR, Use of luting agents with an implant system: Part IIJ Prosthet Dent 1992 68:885-90. [Google Scholar]
[17]. Maeyama H, Sawase T, Jimbo R, Kamada K, Suketa N, Fukui J, Atsuta M, Retentive strength of metal copings on prefabricated abutments with five different cementsClin Implant Dent Relat Res 2005 7(4):229-34. [Google Scholar]
[18]. Mansour A, Ercoli C, Graser G, Tallents R, Moss M, Comparative evaluation of casting retention using the ITI solid abutment with six cementsClin Oral Implants Res 2002 Aug 13(4):343-8. [Google Scholar]
[19]. Sheets JL, Wilcox C, Wilwerding T, Cement selection for cement-retained crown technique with dental implantsJ Prosthodont 2008 17:92-96. [Google Scholar]
[20]. Cano-Batalla J, Soliva-Garriga J, Campillo-Funollet M, Munoz-Viveros CA, Giner-Tarida L, Infuence of abutment height and surface roughness on in vitro retention of three luting agentsInt J Oral Maxillofac Implants 2012 27(1):36-41. [Google Scholar]
[21]. Guncu MB, Cakan U, Canay S, Comparison of 3 luting agents on retention of implant-supported crowns on 2 different abutmentsImplant Dent 2011 20(5):349-53. [Google Scholar]
[22]. Breeding LC, Dixon DL, Bogacki MT, Tietge JD, Use of luting agents with an implant system: Part IJ Prosthet Dent 1992 68:737-41. [Google Scholar]
[23]. Michalakis KX, Pissiotis AL, Hirayama H, Cement failure loads of 4 provisional luting agents used for the cementation of implant-supported fixed partial denturesInt J Oral Maxillofac implants 2000 15:545-49. [Google Scholar]
[24]. Ramp MH, Dixon DL, Ramp LC, Breeding LC, Barber LL, Tensile bond strengths of provisional luting agents used with an implant systemJ Prosthet Dent 1999 81:510-14. [Google Scholar]
[25]. Singer A, Serfaty V, Cement-retained implant-supported Fixed Partial Dentures: A 6 month to 3-year follow-upInt J Oral Maxillofac implants 1996 11:645-49. [Google Scholar]
[26]. Squier RS, Agar JR, Duncan JP, Taylor TD, Retentiveness of dental cements used with metallic implant componentsInt J Oral Maxillofac implants 2001 16:793-98. [Google Scholar]
[27]. Bresciano M, Schierano G, Manzella C, Screti A, Bignardi C, Preti G, Retention of luting agents on implant abutments of different height and taperClin Oral Implants Res 2005 16(5):594-98. [Google Scholar]
[28]. Lorey RE, Edge MJ, Lang BR, Lorey HS, The potential for bonding titanium restorationsJ Prosthodont 1993 2(3):151-55. [Google Scholar]