Giant Peritoneal Loose Body: A Case Report and Review of Literature
Hemanth Makineni1, Poornachandra Thejeswi2, Shivananda Prabhu3, Rahul R. Bhat4
1 Junior Resident, Department of General Surgery, Kasturba Medical College, Mangalore, Manipal Univesity,India.
2 Associate Professor, Department of General Surgery, Kasturba Medical College, Mangalore, Manipal Univesity,India.
3 Professor, Department of General Surgery, Kasturba Medical College, Mangalore, Manipal Univesity,India.
4 Assistant Professor, Department of General Surgery, Kasturba Medical College, Mangalore, Manipal Univesity,India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Poornachandra Thejeswi, Shreyas, Pragathi Coloney, Near Baliga Stores, Bejai, Managalore, India.
Phone: +919986874910,
E-mail: drpoornachandra@gmail.com
A 52-year-old man was presented with discomfort in lower abdomen and irritative voiding symptoms. Computed tomography showed a well circumscribed mass with calcification in front of bladder compressing the bladder diagnosed as leiomyoma with calcifications, probably araising from rectum. Surgery revealed a giant peritoneal loose body measuring 6cm in diameter. After the removal of peritoneal loose body patient was relieved of symptoms. Peritoneal loose bodies are usually small and are found incidentally at surgery. Giant peritoneal loose bodies are rare. A comprehensive review of literature is presented.
Peritoneal loose body, Appendices epiploicae
Case Report
A 52-year-old Indian male was presented to the surgical outpatient department with complaints of discomfort in lower abdomen and increased frequency of micturition, occasionally associated with urge incontinence. Patient was experiencing these symptoms, which were progressively increasing for a duration of six months. He did not complain of burning micturition, haematuria and other bowel symptoms. There was no significant past medical history. General physical examination, abdominal exam including per rectal examination were normal.
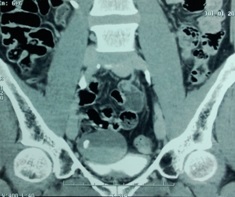
Baseline blood investigations and urine examination were with in normal limits. Computed tomography of abdomen revealed a well defined spherical lesion with calcification located in pelvis, in front of rectum, compressing the bladder [Table/Fig-1]. All fat planes were well made out. A diagnosis of leiomyoma with calcifications, probably arising from rectum was made based on above findings.
Exploratory laparotomy revealed a shiny white, oval, firm Peritoneal Loose Body (PLB) in the recto-vesical pouch compressing the bladder [Table/Fig-2]. The PLB was removed and sent for histopathological evaluation. Post operative recovery was uneventful and patient is relieved of symptoms.

The PLB had smooth surface and measured 6cm in diameter [Table/Fig-3]. Cut surface of PLB showed central yellow fat with calcifications surrounded by white laminated periphery [Table/Fig-4]. Histopathological examination showed central fat necrosis with calcification surrounded by laminated eosinophilic periphery consistent with peritoneal loose body originating from torted appendix epiploica.
Giant Peritoneal Loose Body


Discussion
Giant peritoneal loose bodies are rare with only few reports in literature. The first case of PLB was reported by Littre in 1703. Virchow in 1863 described a case of peritoneal loose body and he proposed from his observations that obesity or infection can lead to increase in the amount of fat deposited in the appendices epiploicae. This fat undergoes saponification and calcification, leads to gradual and progressive obstruction of the blood-vessels of the pedicle. When the vascular obstruction is complete, necrosis of base occurs and appendix epiploica falls into the peritoneal cavity [1]. In 1933, Paterson proposed that torsion and inflammation as the predominant causes for detachment of the appendices epiploicae [2].The fat gets saponified and calcified and over years serum from the peritoneal cavity gets deposited in layers leading to its enlargement. This explains the structure of PLB with a central yellowish portion made up of calcified appendix epiploica and surrounding white laminated fibrinoid material as in our case. Rare cases of loose bodies from torted separated ovaries have been reported [3].
Most PLBs are small, asymptomatic and are found incidentally at laparotomies or as incidentelomas during imaging procedures. However Giant PLBs (measuring more than 5cm) are rare and can present with various symptoms due to extrinsic compression of the viscera like acute retention of urine, constipation, and rarely intestinal obstruction [4]. The PLB in our case measured 6cm caused irritative voiding symptoms due to extrinsic compression of bladder which were relieved post-operatively. Careful pre-operative evaluation is required to avoid unnecessary laparotomies in asymptomatic cases. CT or MRI can be used for the diagnosis but have their own limitations. Loose bodies tend to migrate into the pelvis and can be mistaken radio graphically for a dermoid, teratoma, leiomyoma, calcified uterine fibroid, ovarian cyst or tubercular granuloma [5]. CT imaging often reveals a concentric round or oval, well-defined mass with central calcification, surrounded by a peripheral soft tissue density. In MRI PLB appears as a well-circumscribed, low-intensity mass on both T1 and T2 weight images. The MRI signal is similar to that of muscle and a central high intensity area may be seen on T1 weighted images. PLB does not exhibit any enhancement and this is useful in the process of discrimination because contrast enhancement is achieved in leiomyoma and teratoma. In cases were findings are suspicious of PLB, a repeat scan in prone position is useful to demonstrate the mobility [6].
Conclusion
Giant peritoneal loose bodies are rare clinical entities and are rarely diagnosed preoperatively. Diagnosis of PLB should be considered in cases where imaging modalities show mobile pelvic masses, with central calcifications and well preserved fat planes all around and an attempt should be made to demonstrate mobility by repeating CT scan in prone position. This will reduce unnecessary surgeries for asymptomatic PLBs diagnosed incidentally. When diagnosis is in doubt diagnostic laparoscopy can be performed and symptomatic peritoneal loose bodies can be removed with smaller incisions with minimal morbidity.
[1]. Harrigan Appendices epiploicaeAnn Surg 1917 (66):467-78. [Google Scholar]
[2]. Patterson DC, Appendices epiploicae and their surgical signifi- cance with report of three casesN Engl J Med 1933 209:1255-9. [Google Scholar]
[3]. Bricker Burns J, Rogers James V JR, A Sequestered Ovary as a Loose Peritoneal BodySouth. Med. J 1969 62(8):995-99. [Google Scholar]
[4]. Shepherd JA, Peritoneal loose body causing acute retention of urineBr J Surg 1951 39:185-7. [Google Scholar]
[5]. Takada A, Moriya Y, Muramatsu Y, Sagae T, A case of giant peri- toneal loose bodies mimicking calcified leiomyoma originating from the rectumJpn J Clin Oncol 1998 28:441-2. [Google Scholar]
[6]. Gayer G, Petrovitch I, CT diagnosis of a large peritoneal loose body: a case report and review of the literatureBr J Radiol 2011 84:e83-5. [Google Scholar]