FESS is a minimally invasive technique in which sinus air cells and ostia are opened under direct visualisation. The goal of this procedure is to restore the sinus ventilation and normal function [1]. Though minimally invasive, the surgery is associated with mild to moderate post-operative pain, which is related to both surgical trauma and nasal packing [2]. Routine analgesic treatment is usually based on non-opioid analgesics with rescue opioids [3].
Pre-emptive pain control is where, regional or systemic analgesics are applied before the start of the surgical procedure. The affect is achieved by suppressing, either together or separately, central or peripheral sensitization. Pre-emptive analgesia gives rise to a subsiding pain model, a decrease in analgesic requirements, and a decline in morbidity, promoting wellness and shortening the length of hospital stays [4–6]. However, opinions on the utility of pre-emptive analgesia differ between observers [6,7].
Paracetamol (acetaminophen; N-acetyl-p-aminophenol) is one of the most regularly used drugs worldwide, attributable to an excellent safety profile of the drug. Paracetamol inhibits both isoforms of cyclo-oxygenase (COX); COX-1 and COX-2 and it also reinforces descending serotonergic inhibitory pain pathways [8]. The pre-emptive effect of intravenous paracetamol has been studied in various surgical procedures. While some are of the opinion that iv paracetamol is effective as a pre-emptive analgesic [9] others find no credibility [10]. Even though there are studies to show that intravenous paracetamol provides good analgesia in endoscopic sinus surgeries [11–13] there has been no study to study the pre-emptive effect of paracetamol in these surgeries. The purpose of the present study was to determine the post-operative analgesic effects of pre-emptive iv paracetamol and the amount of reduction in tramadol consumption in FESS.
Materials and Methods
Ethical clearance was obtained by the ethical committee of the institution. After obtaining written informed consent from each participant, 39 patients in the age group of 16 – 69 years, undergoing FESS, were enrolled. The inclusion criteria were ASA physical status I and II, not having any contraindications to the use of the study drug. Patients of age more than 70 years; having history of central nervous system disorders, impaired renal functions, impaired liver function, patients 20% more or less than the ideal body weight, history of allergic reactions to paracetamol or tramadol and patients on chronic analgesic treatment were excluded. Patients were seen on the day before surgery and trained about the usage of the VAS for pain scores. The VAS represents the simple verbal scale and evaluates pain according to the following scores: 0=no pain; 10=excruciating pain.
Study Design
The study was single centred, randomized, double-blind study. The computer-generated block randomization schedule was prepared using random number generator to create a list of random numbers by a statistician. A total of 2 anaesthetists were involved in the study. The attending anaesthesiologist was blinded to the patient grouping.
Group I patients (n=20) received iv paracetamol 1g, 15 minutes prior to induction. In Group II (n=19), iv paracetamol 1g was given at the end of the surgery. In the operating room, Electrocardiogram (ECG), Non-Invasive Blood Pressure (NIBP), Heart Rate (HR), and Peripheral Oxygen Saturation (SpO2) were monitored. Anaesthetic technique was standardized. The patients were preoxygenated for 3 minutes with 100% oxygen. For induction and intubation, 2-2.5 mg/kg propofol, 2 μg/kg fentanyl citrate, and 0.8 mg/kg vecuronium were given. Following intubation, maintenance of general anestahesia was accomplished by providing 2% sevoflurane in 40/60 oxygen/nitrous oxide and, if required, 0.2 mg/kg vecuronium. Patients were extubated when fully awake. All the patients were transferred to Post Anaesthesia Care Unit (PACU).
Post-operative pain was assessed at recovery room till the first hour of surgery and then at the patient’s rooms. VAS pain scores were recorded at 0, 30th minutes and 1, 2, 6, 12, 18, and 24 hours after the completion of surgery. Patients of both groups received iv tramadol 1.5 mg/kg of starting dose and the same dose was repeated with a maximum dose of 400 mg daily. The time for first analgesic requirement was noted. Total consumption of tramadol was noted. Side effects if any, such as nausea, vomiting, respiratory depression, itching, rash, allergic reaction and hypotensions were recorded.
Statistical analysis was performed by using Medcalc 12.6.1.0 for windows. P-values <0.05 were considered significant. Data are presented as mean values and standard deviation (mean ± SD).
Results
Both groups were comparable with regard to demographic variables (age, gender and weight), ASA physical status and the mean duration of surgery time [Table/Fig-1].
Demographic properties and duration of surgery
| Group I (n=20) | Group II (n=19) |
|---|
| Age (year) | 40.7 (9.24) | 43.9 (7.58) |
| Gender M/F | 12/8 | 11/8 |
| ASA I/II | 17/3 | 17/2 |
| Weight (kg) | 48.67 (9.68) | 49.90 (9.46) |
| Duration of surgery (minutes) | 111.60 (15.33) | 109.83 (12.58) |
| Data are expressed as mean (SD) |
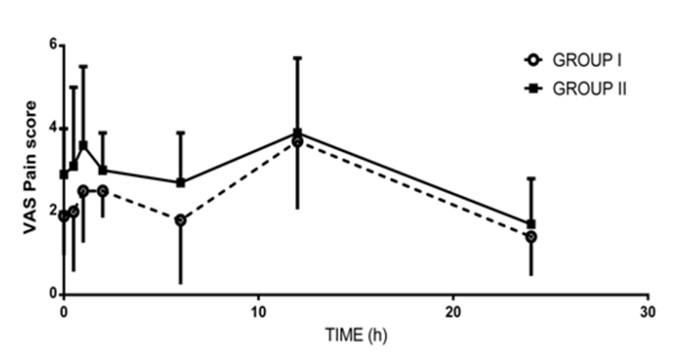
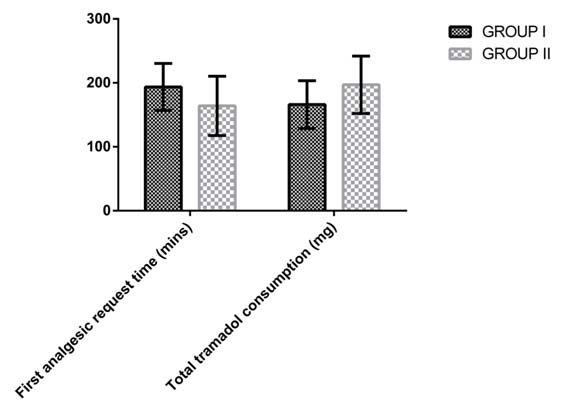
The changes in post-operative VAS pain scores are shown in [Table/Fig-2,3]. Mean VAS pain scores recorded at 15, 30 minutes, 1, 2 and 6 hours were higher in Group II, compared to Group I (P < 0.05). Time to first request analgesic was significantly longer in Group I compared to Group II (P = 0.0329) [Table/Fig-4,5]. The total consumed dose of tramadol during the post-operative 24 hours was significantly less in Group I (P = 0.0141) when compared to Group II.
VAS score for postoperative pain
| 0 minutes | 30 minutes | 1 hour | 2 hours | 6 hours | 12 hours | 24 hours |
|---|
| Group I (n=20) | 1.9 (0.9) | 2.0 (1.4) | 2.5 (1.2) | 2.5 (0.6) | 1.8 (1.5) | 3.7 (1.6) | 1.4 (0.9) |
| Group II (n=19) | 2.9 (1.1) | 3.1 (1.9) | 3.6 (1.9) | 3.0 (0.9) | 2.7 (1.2) | 3.9 (1.8) | 1.7 (1.1) |
| p-value | 0.0036 | 0.0459 | 0.0362 | 0.0474 | 0.0463 | 0.7156 | 0.3562 |
Data expressed as mean (SD). Statistically significant if p <0.05
Comparison of VAS scores between the two groups
First analgesic requirement time, post-operative analgesic requirements and total length of hospital stay.
| Group I | Group II | p-value |
|---|
| First analgesic requirement time (minutes) | 193.6 (36.8) | 164 (46.3) | 0.0329 |
| Total tramadol consumption | 166 (37.41) | 197 (44.79) | 0.0141 |
| Data expressed as mean (SD). Statistically significant if p <0.05. |
Comparison of first analgesic requirement time and total tramadol consumption between the two groups
Incidence of side effects (Number of patients who experienced the side effects (%))
| Group I | Group II |
|---|
| Nausea | 6 (30) | 5 (26) |
| Vomiting | 2 (10) | 3 (15) |
| Itching | - | - |
| Respiratory depression | - | - |
| Hypotension | - | - |
| Allergic reaction | - | - |
| Data expressed as mean (SD). Statistically significant if p <0.05. |
Post-operative side effects of the cases are shown in [Table/Fig-6]. Incidence of nausea and vomiting was similar in both the groups. About 30% patients developed nausea in Group I whereas in Group II it was 26%. About 10 % patients had vomiting in group I whereas the incidence was 15% in group II. No other side effects were recorded in either of the groups.
Discussion
Despite widespread use for over five decades, the mechanism of action of paracetamol is still unclear. Current evidence points to inhibition of prostaglandin synthesis (cyclooxygenase (COX) inhibition), and interaction with both serotonergic and cannabinoid pathways. Non-steroidal Anti-inflammatory Drugs (NSAIDs) also act by inhibition of COX, yet important differences exist; notably, paracetamol displays weak anti-inflammatory activity, few or no gastrointestinal side effects, and only a small dose-dependent alteration of platelet function [8].
Two systematic reviews have found the rate of adverse events following administration of paracetamol is not significantly different to that following administration of placebo [14,15], while hypersensitivity reactions are rare [16]. The onset and duration of paracetamol’s analgesic action is determined to a large extent by the route of administration. Intravenous administration will achieve therapeutic plasma concentrations within 20 minutes of an initial dose, and concentrations remain therapeutic for around 2 hours post dose [17]. Paracetamol has been found to be highly effective in pain treatment after endoscopic sinus surgery [11]. Unlike our study, the control group received intravenous paracetamol after the surgery. Also, the endoscopic surgeries were carried out under local anaesthesia, whereas in our study, all cases were done under general anaesthesia. On literature search, we found no studies on paracetamol being used as a pre-emptive analgesic in endoscopic sinus surgeries.
Pre-emptive analgesia means that an analgesic intervention is started before the noxious stimulus arises in order to block peripheral and central nociception. This afferent blockade of nociceptive impulses is maintained throughout the intra-operative and post-operative period. The goals of pre-emptive analgesia are, first, to decrease acute pain after tissue injury, second, to prevent pain-related pathologic modulation of the central nervous system, and third, to inhibit the persistence of post-operative pain and the development of chronic pain [6].
Intravenous paracetamol has been used as a pre-emptive analgesic in various other surgeries [9,10,13]. Arici and colleagues [9] have found that preemptively administered iv paracetamol 1g in patients undergoing a total abdominal hysterectomy operation had no negative effects on intra-operative or post-operative hemodynamic parameters, ensured an effective analgesia during the post-operative period, increased patient satisfaction by reducing post-operative morphine consumption and side effects, and thereby shortened the length of hospital stay. In our study, we have similarly found that paracetamol 1g given pre-operatively ensures effective analgesia and reduces total analgesic consumption.
Toygar and colleagues studied the pre-emptive analgesic effect of intravenous paracetamol in lumbar disk surgeries [10]. Similar to our study they administered paracetamol 1g 15 mins prior to the induction (group I) and in another group paracetamol 1g was given at the end the surgery (group II). Even though the VAS pain scores and total morphine consumption (delivered through patient controlled analgesia) was lower in group I, the difference was not statistically significant.
Sabry and colleagues have compared the efficacy of pre-emptive gabapentin and paracetamol in adenotonsillectomies [13]. They found premptive gabapentin to be more efficacious compared to paractemol, but unlike our study they used oral paracetamol. While oral bioavailability is good (63–89%), early plasma concentrations following oral administration may vary, and in some cases concentrations may remain subtherapeutic for a significant period [8]. Also, there may be a large variation in individual levels, as found in a previous study [18].
In another study, [19] 300 patients, posted for laparoscopic cholecystectomy were grouped into pre-emptive and post-operative paracetamol groups and the analgesic efficacy was compared with a placebo group. Similar to our study, they found that time to first analgesic requirement was significantly longer in the pre-emptive. Total analgesic consumption and post-operative VAS pain scores recorded were significantly lower in the group in which paracetamol was pre-emptively used.
In our study, the time first analgesic requirement was significantly longer in Group I (P = 0.0329). We believe that pre-emptively delivered paracetamol in group I prevented central sensitization, so its analgesic effect continued longer than its effect period. This is substantiated by the fact that the VAS scores recorded in the immediate post-operative period till the 12th hour are significantly lower. The VAS scores recorded were lower in every time frame till the 12 th hour .This led to reduced tramadol consumption in the first 24 hours. The reduction in total tramadol consumption may also be due to the opioid sparing effect of pre-emptive paracetamol which has been seen in other studies as well [9,19].
Adverse effects of tramadol, nausea in particular, are dose-dependent and therefore considerably more likely to appear if the loading dose is high [20]. In our patients initial VAS scores were lower in Group I compared to Group II. Hence we believe that use of pre-emptive paracetamol can reduce the loading dose of tramadol. The reduction of this dose during the first days of treatment is an important factor in improving tolerability. The most common adverse effects of tramadol are nausea, vomiting, dizziness, fatigue, sweating, dry mouth, drowsiness and orthostatic hypotension [21]. In our patients, only nausea and vomiting were observed. The incidence of side effects was equal in both the groups. Even though number of patients who experienced these side effects was similar, patients in Group II experienced more episodes of nausea and vomiting and required greater dose of rescue antiemetic. There were no observed episodes of respiratory depression or hypotension. This was possibly because no patient in either group received tramadol in excess of maximum daily dose of 400 mg.
Conclusion
Our findings indicate that pre-emptively administered iv paracetamol 1g in patients undergoing FESS ensures an effective analgesia during the post-operative period, increases the time to first analgesic requirement and reduces tramadol consumption. Therefore, we believe that in comparison to paracetamol 1g administered intra-operatively, paracetamol administered pre-emptively can provide better analgesia in the post-operative period in FESS.
Data expressed as mean (SD). Statistically significant if p <0.05