Root End Generation: An Unsung Characteristic Property of MTA-A Case Report
Seema Dixit1, Ashutosh Dixit2, Pravin Kumar3, Saurabh Arora4
1Professor, Department of Conservative Dentistry & Endodontics,Seema Dental College, Rishikesh, India.
2Professor, Department of Periodontics,Seema Dental College,, Rishikesh, India.
3Professor & HOD, Department of Conservative Dentistry & Endodontics,Seema Dental College, Rishikesh, India.
4Senior Lecturer, Department of Conservative Dentistry & Endodontics,Seema Dental College, Rishikesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Seema Dixit, 1/3, Semal Road, Shiprasuncity, Indirapuram, Ghaziabad, Uttar Pradesh, India.
Phone: 9818696704,
E-mail: seemadixit247@gmail.com
Management of immature teeth with necrotic pulp and periapical lesion has long presented a challenge. The treatment of choice for such teeth is apexification, which is induction of apical closure to produce more favorable conditions for conventional canal obturation. Traditionally, calcium hydroxide has been used for the apexification of immature permanent teeth, however, Mineral Trioxide Aggregate (MTA) holds significant promise not only as an alternative to multiple treatment visits with calcium hydroxide but also having the potential to induce root end development, eventually forming a completed root apex. This case report presents a successful healing and apexification with the use of calcium hydroxide and MTA. A 5-year follow-up revealed root development with MTA.
Apexification, Hertwig’s Epithelial Root Sheath, Calcium Hydroxide, Mineral Trioxide Aggregate
Case Report
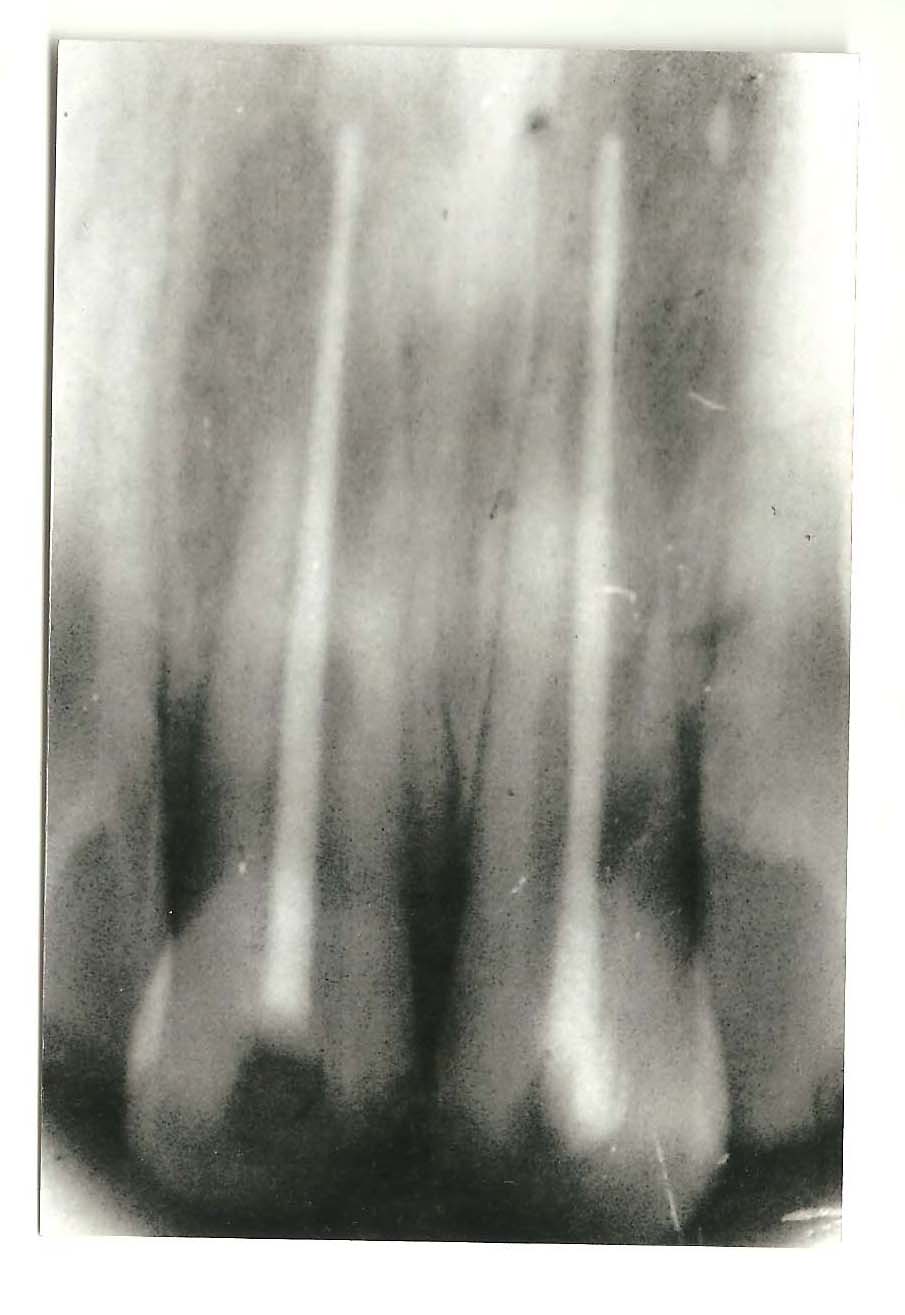
A 15-year-old male patient came to the Department of Conservative Dentistry and Endodontics, ITS Dental College, Muradnagar, India with complaint of pain and swelling in upper anterior region. On oral examination, a soft fluctuant swelling was present in the upper facial vestibule. No coronal restoration was present in either 11 or 21 and they were tender. There was a history of trauma and root canal treatment 7 years back. Radiographic examination revealed single cone placed in 11 & 21, root resorption that was visible in both the teeths, open apices in both teeth, irregular canal anatomy in 11 and large periradicular lesions were present in both 11 & 21 [Table/Fig-1]. A treatment plan was finalized to place MTA in 11 and Metapex in 21. Although, difficult but it was decided to place MTA in the apical area through the root canal as consent for surgical approach could not be obtained.
The treatment started with the removal of gutta percha from 11 & 21 and establishing drainage for the purulent hemorrhagic discharge. Once the discharge ceased, working length determination was done [Table/Fig-2]. Teeth were irrigated copiously with sodium hypochlorite. Canals were dried with paper points. Calcium hydroxide powder was mixed with saline solution to form a paste and placed in 11 & 21 with lentulospiral fillers. Access cavities were sealed with the temporary filling material Cavit G. Patient was recalled after two weeks. After two weeks, the cavit G was removed from the 11 the canal appeared clean and dry with no signs of exudate. The canal was irrigated with sodium hypochlorite and dried with paper points. MTA was placed in 11 by using Messing gun and condensed using hand plugger. A wet cotton was placed in the canal & canal was sealed with cavit G. A radiograph was taken to confirm the placement of MTA. Due to irregularities present in the canal, MTA of adequate thickness (3mm) could not be placed properly. In case of 21, the root canal procedure was undertaken as specified earlier, till the drying of the canal. After the canal was dried, metapex syringe was inserted till the working length and injected till the metapex was visible on the canal orifice. Metapex was further condensed using hand plugger. A cotton pellet was placed in the chamber and access was sealed with cavit G.
Patient was recalled after 24 hours. Next day, 11 was opened, wet cotton pellet removed and integrity of MTA was verified using a #30 file. Although, apical plug was present, thickness of MTA was not sufficient (3 mm) to prevent microleakage, metapex dressing was placed to sterilize the canal in 11 [Table/Fig-3]. The patient was instructed to return 2 weeks later for the continuation of treatment. For some reason, the patient did not report back as instructed. Six months later the patient returned to the Department for continuation of the treatment. Patient was asymptomatic, having no pain, no swelling. Intra-orally, temporary restoration was intact, no tenderness to percussion was observed in 11 & 21. A periapical radiograph was exposed to evaluate the periapical condition and revealed some healing of the periapical lesions in relation to 11 & 21.
The cavit G was removed from 21. The root canal was irrigated with copious amount NaOCl followed by saline solution. The metapex was removed by using H-file and copious irrigation with NaOCl repeatedly. The canal was finally rinsed with 17% EDTA. The formation of apical barrier was confirmed by using No. 25 file. There was a soft but definite stop. The canal was dried by using paper point. A customized GP was prepared by rolling three # 80 2% GP between the glass slab & taking the impression of canal. The canal was obturated with customized GP combined with root canal sealer.
Same procedure was followed for 11. The residual metapex was removed from canal. Irrigation with copious amount of 5% NaOCl & alternating with saline was done. Final rinse with 17% EDTA was done. In 11 due to irregularities of canal, customized GP could not be prepared so lateral condensation of GP was done [Table/Fig-4]. Both the teeth were permanently restored followed by crown preparation and placement. Follow up radiograph were taken after 1 [Table/Fig-5], 2 [Table/Fig-6], 3, 4 and 5 [Table/Fig-7] years. Follow up visits revealed absence of clinical symptoms and reduction in periapical rarefaction and adequate function.






Discussion
Traumatic injuries to permanent teeth occur in 30% of children (Andreasen JO et al.,) [1]. The majority of these incidents occurs before root formation is complete and may result in pulp inflammation and necrosis (Andreasen JO and Andreasen FM) [2]. The completion of root development occurs up to 3 years after eruption of the tooth [3]. The treatment of pulpal injury during this period provides significant challenge for the clinician. The treatment depends upon the vitality of the affected pulp. If the pulp is vital-Apexogenesis is perfomed to encourage continued physiological development and formation of the root end. If pulp has become non-vital- Apexification is performed [4]. The main challenge in performing root canal treatment in teeth with necrotic pulps and wide-open apices is to obtain an optimal apical seal. The wide foramen requires a large volume of filling material that may extrude from root canal into peri-apical tissues creating foreign-body responses and eventually compromising the apical seal (Rafter M) [5].
Several procedures by utilizing different materials have been recommended to induce root-end barrier formation. Apexification with calcium hydroxide is the most commonly advocated therapy for immature teeth with non-vital pulp and the healing rate has been reported to be high [6]. However, calcium hydroxide apexification technique has a number of disadvantages like prolonged treatment time ranging from 3-24 months [6], require multiple visits for either reapplication of Ca(OH)2 or to check its presence inside the root canal [7]. In addition Andreasen et al., reported that the fracture strength of immature teeth may be reduced by long-term calcium hydroxide treatment [8].
One alternative for calcium hydroxide apexification is a single- step technique by using an artificial apical barrier. The one-visit apexification has been described as the non-surgical compaction of a biocompatible material into the apical end of the root canal, thus, creating an apical stop and enabling immediate filling of the root canal [8].
A number of materials have been proposed for this purpose including tri-calcium phosphate, freeze dried bone, freeze dried dentin, collagen calcium phosphate [9]. Over the last decade, MTA has been researched extensively and has been suggested as a preferred material for one-visit apexification. Felippe WT et al (2006) reported that MTA, when applied as an apical plug favoured apexification and peri-apical healing, regardless of the prior use of calcium hydroxide paste [10].
The major limitation in this apexification technique is the duration of the therapy which ranges from 3-21 months. The duration depends 292on factors such as size of the apical opening, the traumatic displacement of the tooth and the repositioning methods used [11].
A permanent treatment plug is preferable to limit reinfection that could cause apical periodontitis and inhibit canal closure. The importance of the coronal seal was shown by Tronstad L et al., who found the highest success rate in teeth diagnosed with good endodontics and good coronal restorations. The rate dropped by 10% in teeth with good endodontics and poor restorations and in teeth with poor endodontics and good restorations, the success rate dropped even further [12].
With the MTA apical plug technique, one-step obturation after short canal disinfection with calcium hydroxide could be performed. The MTA mixture created artificial stop to the filling material. MTA has good sealing ability, good marginal adaptation, a high degree of biocompatibility and reasonable setting time. MTA can be used in the presence of moisture in the root canal [13]. Witherspoon and Ham K asserted that MTA provides scaffolding for the formation of hard tissue and the potential of a better biological seal [14].
In the present case, apexification was done by using both calcium hydroxide in 21 and MTA in 11. Both the teeth showed healing but healing was more complete in the tooth treated with MTA. One peculiar finding observed with MTA was the formation of root apex. There are a number of reports of continued apical development in spite of a necrotic pulp. Yang SF et al., reported a case in which apical barrier formation was accompanied by a separate disto-apically growing root [15]. Similarly Soares J et al., reported a case of calcium hydroxide apexification associated with apical root development. The reason of root development was stated to be the reactivation of Hertwig’s epithelial root sheath remnants which in turn promoted the root formation genetically programmed for that tooth [16].
Both clinical and radiographic follow ups in the present case showed healing of periapical tissues but more complete healing with MTA.
Conclusion
MTA apical plug method is an effective and a successful method of apexification because of the less treatment time required, fewer number of appointments and radiographs and better fracture resistance after the treatment of non-vital immature permanent teeth.
[1]. JO Andreasen, LK Bakland, RC Matras, FM Andreasen, Traumatic intrusion of permanent teeth Part 1. An epidemiological study of 216 intruded permanent teeth 2006 22:83-9. [Google Scholar]
[2]. JO Andreasen, FM Andreasen, Textbook and color atlas of traumatic injuries to the teeth 1994 3rd EditionCopenhagenMunksgaard [Google Scholar]
[3]. SN Bhasker, Orban’s oral histology and embryology 1991 11th EditionSt. Louis, Mosby [Google Scholar]
[4]. American Association of Endodontists. Glossary of endodontic terms 2003 7th EditionChicagoAmerican Association of Endodontists [Google Scholar]
[5]. Apexification Rafter M, A reviewDent Traumatol 2005 21:1-8. [Google Scholar]
[6]. JC Steiner, PR Dow, GM Cathy, Inducing root end closure of non-vital permanent teeth.J Dent Child 1968 35:57-9. [Google Scholar]
[7]. AL Frank, Therapy for the divergent pulpless tooth by continued apical formationJ Am Dent Assoc 1996 72:87-93. [Google Scholar]
[8]. JO Andreasen, B Farik, EC Munksgaard, Long-term Ca(OH)2 as a root canal dressing may increase risk of root fracture.Dent Traumatol 2002 18:134-37. [Google Scholar]
[9]. TH Steinig, JD Regan, JL Gutmann, The use and predictable placement of mineral trioxide aggregate in one- visit apexification casesAus Endod J 2003 29:34-42. [Google Scholar]
[10]. WT Felippe, MCS Felippe, MCS Rocha, The effect of mineral trioxide aggregate on the apexification and periapical healing of the teeth with incomplete root formationJ Am Dent Assoc 2006 72:87-93. [Google Scholar]
[11]. Z Metzer, M Solomonov, E Mass, Calcium hydroxide retention in wide root canals with flaring apicesDent Traumatol 2001 :17-86. [Google Scholar]
[12]. L Tronstad, K Asbjornsen, I Pedersen, HM Ericksen, Influence of coronal restorations of the periapical health of endodontically treated teethEndod Dent Traumatol 2000 16:218-21. [Google Scholar]
[13]. V Giuliani, T Baccetti, R Pace, G Pagavino, The use of MTA in teeth with necrotic pulps and open apices.Dent Traumatol 2002 18:217-21. [Google Scholar]
[14]. DE Witherspoon, K Ham, One visit apexification: technique for inducing root end barrier formation in apical closures.Pract Proced Aesthet Dent 2001 13:455-60. [Google Scholar]
[15]. SF Yang, ZP Yang, KW Chang, Continuing root formation following apexification treatmentEndod Dent Traumatol 1990 6:232-5. [Google Scholar]
[16]. J Soares, S Santos, C Cesar, P Silva, M Sa, F Silveira, E Nunes, Calcium hydroxide induced apexification with apical root development: a clinical case reportInt Endod J 2008 41:710-9. [Google Scholar]