Thyroid nodules are rare in children and adolescents, affecting 1% to 2% of the paediatric population, at large [1]. However it has been shown that”, “Incidence of malignancy in paediatric thyroid nodules is high and the risk of surgical complication significant” [2]. Various studies have also found that, “Incidence of cancer in solitary nodules ranges from 14% to 40% as compared to 5% in adults” [3]. Benign lesions have to be differentiated from malignant lesions as they are managed in a different way. Fine needle aspiration is very useful as a screening test for thyroid nodules. Its utility has increased significantly in recent years, particularly because of the availability of ultrasound guided techniques, which allow detection and aspiration of smaller and deep-seated nodules. Consequently, more thyroid cancers are diagnosed at an early stage. The main role of thyroid Fine Needle Aspiration Cytology (FNAC) is to help triage patients for either surgery or conservative management. Patients with FNAC diagnosis that suggest neoplasia and malignancy are managed surgically, whereas, patients with FNAC diagnosis that favour a benign lesion can be followed clinically [4].
Among adults the use of FNAC has reduced the number of patients who have undergone surgery for benign thyroid disease and increased the yield of malignancy in surgical specimens from 5-10% to as much as 30% to 50% [5]. But, FNAC of the thyroid gland has not been used extensively in children, even though it has been safe and effectively used in the assessment of thyroid nodules in adults [4,5].
A few studies discuss the role of FNAC in the management of paediatric and adolescent thyroid disease [6–14] and its reliability in selecting patients for surgical exploration. The purpose of this study is to highlight the cytomorphological spectrum seen in paediatric and adolescent thyroid aspirates and to compare the findings with the other studies.
Materials and Methods
The present study was undertaken in the Department of Pathology, Mysore Medical College and Research Institute, Mysore, Karnataka, India from January 2009 to December 2012 (4 years). Among 4560 thyroid FNACs, 284 were performed on patients who were less than 21 years old.
Fine needle aspiration was performed by the pathologist using a 23 gauge needle attached to a disposable 10ml syringe. The aspirated material was expressed onto slides and smears were prepared. Half of the smears were immediately fixed in 95% ethyl alcohol for subsequent Papanicoloau and Haematoxylin and Eosin staining. The remaining smears were air-dried and stained by May-Grunwald-Giemsa Stain.
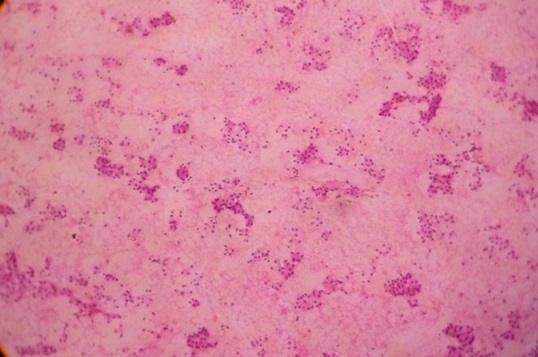
FNAC results were categorized as benign, suspicious for a neoplasm, neoplastic and unsatisfactory. The aspirates were classified as “Benign NOS” (Not otherwise specified) when they were characterized by colloid and 6 or more groups of benign follicular cells. “Cystic change” was reported when macrophages with or without hemosiderin were identified. “Hyperplasia” was characterised by fire-flare appearance of the follicular cells. “Thyroiditis” was reported, when there was Askanazy change and lymphocytic infiltrate. The aspirates under the category of “Suspicious for malignancy” included those with features suggestive but not diagnostic of a Papillary carcinoma. Suspicious lesions also, included aspirates that were interpreted as “Follicular lesion” [Table/Fig-1] when it was difficult to differentiate a hyperplastic nodule from a follicular neoplasm or a follicular variant of Papillary carcinoma.
FNAC Follicular Neoplasm (H & E x 10x)
FNAC Papillary Carcinoma Thyroid (H & E x 10x)
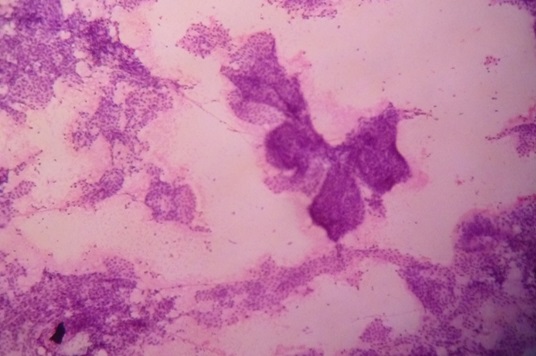
The aspirates categorized as “Neoplastic” included those with the morphologic features diagnostic of a Papillary carcinoma [Table/Fig-2]. The “Unsatisfactory aspirates” had fewer than 5 groups of follicular cells in each aspirate. A cyto-histologic correlation was attempted wherever possible.
Sensitivity, Specificity and Accuracy of FNAC, in diagnosing thyroid malignancy in correlation to the final histological diagnosis were calculated for statistical analysis.
The cases which were diagnosed “Suspicious” or “Malignant” by cytology and were found to have a malignant lesion at surgery were considered, “True positive”. The “True negative”, cases comprised of lesions considered as “benign”, including follicular adenoma, which were also benign on Histopathology of the resected specimen. Cases with benign cytological diagnosis that were found to be malignant at surgery were included in the “false negative category”. The patients with “suspicious” or “malignant” cytology and benign histology were considered false positives.
Results
Out of the 284 FNACs of palpable thyroid lesions in the pediatric and adolescent age-group, 259 (91.1%) were females and 25 (8.9%) were males. The patients age ranged from 7 to 21 years. The distribution of female and male patients in different age groups is shown in [Table/Fig-3]. The female to male ratio was 10.4:1. The genderwise distribution of the thyroid lesions is shown in [Table/Fig-4]. In age group of 7 to less than 12 years, 7 cases (64%) were reported as benign and 4 cases (36%) as thyroiditis. Out of these 2 were male patients with a benign cytology. In the age group of 12 to less than 16 years, 13 (25%) and 39 (75%) cases were reported as benign cytology and thyroditis, respectively. Eight were male patients (3 with benign cytology and 5 with thyroiditis). In the age-group of 16 to less than 19 years; 33(40%); 46 (56%), 1(1.2%), 2(2.8%) cases were reported as benign cytology, thyroiditis, suspicious cytology and papillary carcinoma. In the age-group of 19-21 years; 36(31%), 65(56%), 11(9.5%), 4(3.5%) cases were reported as benign cytology, thyroiditis, suspicious and papillary carcinoma respectively.
Comparison of age distribution between males and females presenting with enlarged thyroid
| Years | Total No. of Cases | Satisfactory Aspirates | Unsatisfactory Aspirates | No. of Females | No. of Males |
|---|
| 7 - <12 | 14 (4.9%) | 11 (4.2%) | 3 (13.04%) | 12 (4.6%) | 2 (8%) |
| 12 < 16 | 58 (20.4%) | 52 (19.9%) | 6 (26.08%) | 47 (18.1%) | 11 (44%) |
| 16 - < 19 | 89 (31.3%) | 82 (31.4%) | 7 (30.4%) | 85 (32.8%) | 4 (1.6%) |
| 19 – 21 | 123 (43.3%) | 116 (44.4%) | 7 (30.4%) | 115 (44.4%) | 8 (32%) |
| Total | 284 | 261 (91.9%) | 23 (8.1%) | 259 (91.1%) | 25 (8.9%) |
Distribution of thyroid lesions in satisfactory fine needle aspirates in various age groups
| Age Group (Years) | Total No. of Satisfactory Aspirates | Benign Cytology | Thyroiditis | Suspicious Cytology | Papillary Carcinoma |
|---|
| ? Follicular | ? Papillary |
|---|
| 7 <12 | 11 (4.2%) {9, 3.7%} [2, 9.5%] | 7 (7.8%) {5, 6.4%} [2, 18.2%] | 4 (2.6%) | | | |
| 12 <16 | 52 (19.9%) {44, 18.3%} [8, 38.1%] | 13 (14.6%) {10, 12.8%} [3, 27.3%] | 39 (25.3%) {34, 23.3%} [5, 62.5%] | | | |
| 16 <19 | 82 (31.4%) {78, 32.5%} [4, 19%] | 33 (37%) {31, 39.8%} [2, 18.2%] | 46 (29.9%) {44, 30.1%} [2, 25%] | 1 (10%) | | 2 (33.4%) |
| 19 <21 | 116 (44.4%) {111, 46.2%}[7, 33.3%] | 36 (40.4%) {32, 41%} [4, 36.4%] | 65 (42.2%) {64, 43.9%} [1, 12.5%] | 9 (90%) {7, 87.5%} [2, 100%] | 2 (100%) | 4 (66.6%) |
| Total | 261 {240, 91.9%}[21, 8.1%] | 89 (34.1%) {78, 29.9%} [11, 4.2%] | 154 (59%) {146, 56%} [8, 3%] | 10 (3.8%) {8, 3%} [2, 0.7%] | 2 (0.8%) | 6 (2.3%) |
Numbers in ( ) indicate percentage
Numbers in { } indicate female cases and the percentage of aspirates in females
Numbers in [ ] indicate male cases and the percentage of aspirates in males
Benign cytology was reported in 34.2% aspirates, out of which 29% were in females and 4.2% were in males. Thyroiditis was reported in 154(59%) cases, out of which 56% were in females and 3.1% were in males. Suspicious cytology was reported in 12 cases (4.5%), out of which 3.8% were females and 0.7% males. Carcinoma was reported in 6 cases (2.3%) and all were females. Majority of the lesions were in the 19-21 years age group.
Thirty one patients underwent thyroidectomy. Out of the 20 patients with benign cytological diagnosis, 19 cases were benign on histology and 1 case had a histological diagnosis of Papillary carcinoma. 6 cases were suspicious for follicular neoplasm on cytology, one was Adenomatous hyperplasia and 5 cases were follicular adenomas on histopathology. One case of papillary carcinoma on cytology was Hashimotos on histopathology. Four cases cytologically diagnosed as papillary carcinomas were Papillary carcinoma on histopathological examination.
The diagnostic accuracy of FNAC was 90% with a Sensitivity of 96% and Specificity of 66%. The positive and negative predictive values were 66% and 96% respectively.
Of the 2 false positive cases, one was follicular lesion on cytology but was diagnosed as Adenomatous hyperplasia on histopathology. Another case was diagnosed as papillary carcinoma on cytology but was Hashimoto’s thyroiditis on HPE. One false negative case was Hyperplastic goitre on cytology but was papillary carcinoma on HPE. Four true positive cases were diagnosed as papillary carcinoma both on cytology and histopathology. Twenty four cases were true negative out of which 5 cases were follicular adenoma, 6 cases were thyroiditis and 13 cases were nodular colloid goitre, and Adenomatous hyperplasia on HPE.
Discussion
Thyroid nodular disease comprises a wide spectrum of disorders, including a solitary nodule, multinodular goiter, nodular goiter observed in autoimmune thyroiditis and thyroid neoplasms [15].
In adults, FNAC has become a part of the routine evaluation of thyroid nodules. Chang et al., [9], noted in their study that since its introduction, the percentage of patients that have undergone thyroidectomy has decreased by 25% to 50% with the use of FNAC [7]. But, FNAC has been underutilized for evaluation of thyroid nodules in the young because of the possibility of complications and the need for sedation. They, also observed that sedation is rarely required and no complication have arisen. They opined that FNAC is a relatively simple procedure with few complications [9] Our study shows concurrent observations.
Thyroid nodules are quite common in the general population, but the vast majority of these nodules are benign [16]. By isolating the pediatric population, the prevalence of thyroid nodules becomes 10 fold lower, ranging between 1 to 2% [17].
Managing pediatric patients with thyroid nodules can be challenging. The diagnostic approach to pediatric thyroid nodules, depends on the differentiation between benign and malignant lesions in order to avoid thyroidectomy for a benign nodule. A high percentage of these patients harbour malignancies and thus, require surgical intervention but these procedures are challenged by anasthesia, small neck size and age etc. Therefore accurate pre-operative diagnosis is paramount [18].
In adult population, FNAC has evolved as a sensitive screening tool to limit the number of thyroid resection. Cited limitations are those related to sampling technique, the skill of the aspirator, experience of the cytopathologist and difficulty in differentiating benign Hurthle cell and follicular tumors from their malignant twins [19].
A few series reported on the utility of FNAC in children and adolescent patients. Comparison of the various series reported shows that benign nodules significantly outnumber those that are malignant [Table/Fig-5].
Comparative analysis of study results of FNAC in children and adolescents { } = Number of aspirates.
| Series | No. of Cases | Sex | Mean Age (Year) | Ae Range (Year) | FNA Results |
|---|
| M (%) | F (%) | Benign (%) | Malignant (%) | Suspicious (%) | Insufficient (%) |
| Arda et al., (2001) [11] | 46 | 9(19) | 37(81) | 9 | 5-16 | 38 (82) | 3(7) | 3(7) | 2(4) |
| Al-Shaikh et al., (2001) [12] | 41 | 35(85) | 6(15) | 13 | 0.3-13 | 30 (73) | 2(5) | 6(15) | 3(7) |
| Khurana et al., (1999) [7] | 57 | 11 (19) | 46(81) | 17 | 9-20 | 36 (63) | 7(12) | 14(25) | 0 |
| Lugo-Vicente et al., (1998) [13] | 24 | 4(17) | 20 (83) | 15 | 9-18 | 11 (61) | 2(11) | 2(11) | 3(17) |
| Degnan et al., (1996) [6] | 18 | 4(22) | 14(78) | 14 | 8-18 | 7(41) | 2(12) | 7(41) | 1 (6) |
| Raab et al., (1995) [14] | 57 | 8(14) | 49 (86) | 13 | 1-18 | 51 (77) | 4(6) | 8(12) | 3(5) |
| Chang et al., (2006) [9] | 51 | 13(25) | 38(75) | 17 | 2-21 | 45 (74) | 6(10) | 5(8) | 4(7) |
| Hosler et al., (2006) [10] | 82{101} | 19(23) | 63 (77) | 15 | 8-18 | 48 (48) | 40 (40)* | | 13(13) |
| Amrikachi et al., (2005) [8] | 218 | 23(12) | 162(88) | 17 | 10-21 | 119(54) | 17(8) | 20 (9) | 62 (28) |
| Kapila et al., (2010) [23] | 792 | 68 (9) | 724(91) | 17 | 4-21 | 699 (88) | 20(2.7) | 26(3.5) | 47 (6) |
| Present study | 284 | 25 (9) | 259(91) | 17 | 7-21 | 243 (86) | 6 (2) | 12 (4) | 23 (8) |
*Includes both malignant and suspicious aspirates
In our study, Sensitivity was 96%, Specificity 66%, Accuracy 90%. Similar results were observed by Amrikachi et al., [8] who had 100% Sensitivity and Specificity of 65%. In the study by Chang et al., [9] the Sensitivity was 100%, Specificity 63%, Accuracy was 81%. Corrias et al., [20], noted Sensitivity, Specificity, Accuracy of 95%, 86.3% and 90.4% respectively.
In the false positive case in our study, the presence of nuclear grooves and syncytial fragments mislead to a cytological diagnosis of papillary carcinoma. The nuclear grooves are non-specific features which can be seen, even in cases of Hashimoto’s thyroiditis, nodular hyperplasia with oncocytes, follicular adenoma or Hurthle cell adenoma [21].
In another false positive case, a nodular hyperplasia was misdiagnosed as follicular adenoma on cytology, since high cellularity and microfollicular pattern were seen in the smears. Yang et al., [4] suggested that, the most important clue in differentiating follicular neoplasm from nodular hyperplasia was the presence of abundant blood containing microfollicles in the follicular neoplasm [22]. However, macrofollicular adenomas have far lower microvessel density than microfollicular nodules because the space occupied by the large colloid lakes are devoid of blood vessels. Therefore, macrofollicular adenomas may be diagnosed as nodular hyperplasia by FNAC. Likewise, a discrete but unencapsulated microfollicular nodule may be diagnosed as “follicular neoplasm” by FNAC resulting in excision of non-neoplastic nodules [9].
In one false negative case a Papillary carcinoma was misdiagnosed as hyperplastic nodule on cytology. This was, because the tiny focus of papillary carcinoma was not aspirated during FNAC. Limitations of FNAC include, the aspirator’s expertise which affects sampling and the experience of the cytopathologist interpreting the specimen. Both may affect the number of false positives and false negatives.
Radiological imaging, serological and molecular studies have made major advances in the last decade in the diagnosis and management of patients with thyroid diseases. However, to date, there is no single appropriate non invasive diagnostic test in clinical medicine that can accurately, in a timely and cost effective manner distinguish benign (mostly approached nonsurgically) from malignant (mostly managed surgically) nodules, except FNAC [24].
Conclusion
FNAC is a good screening test for thyroid nodules, in children and adolescents because of its high sensitivity. The results of our study indicate that the majority of paediatric thyroid enlargements are benign and that, surgery is necessary in only a select number of patients but detection of malignant or suspicious cells is a definite indication for surgery. However, a negative FNAC must be viewed with caution and patients with negative FNAB results should have a close clinical follow up.
Numbers in ( ) indicate percentage
Numbers in { } indicate female cases and the percentage of aspirates in females
Numbers in [ ] indicate male cases and the percentage of aspirates in males
*Includes both malignant and suspicious aspirates