Intra–muscular Nodular Fasciitis Presenting as Swelling in Neck: Challenging Entity for Diagnosis
Sankappa P. Sinhasan1, Bharathi K.V.2, Ramachandra V. Bhat3, Basavanandaswamy C. Hartimath4
1 Associate Professor, Department of Pathology, Indira Gandhi Medical College & Research Institute, Pondicherry, India.
2 Assistant Professor, Department of Pathology, Indira Gandhi Medical College & Research Institute, Pondicherry, India.
3 Professor, Department of Pathology, Indira Gandhi Medical College & Research Institute, Pondicherry, India.
4 Associate Professor, Department of Surgery, Indira Gandhi Medical College & Research Institute, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sankappa P. Sinhasan, Associate Professor, Department of Pathology, Indira Gandhi Medical College & Research Institute (IGMC & RI), Pondicherry—605 009, India. Mobile: +91 9442551998, 094480 61975, E-mail – drspsinhasan@gmail.com
The diagnosis of Nodular Fasciitis is a very challenging on cytological aspirations. Even in histopathological sections, it can be sometimes be mistaken for soft tissue sarcomas due to its high cellularity, presence of mitotic figures, poor circumscription and degenerative myxoid areas. Most commonly, nodular fasciitis is seen on extremities; and sub-cutaneous form is most common. We are hereby reporting a case of nodular fasciitis at a rare site (head and neck area) in its rare form (intra-muscular type: originating within sternocleidomastoid muscle), which was clinically suspected as a malignancy arising from solitary thyroid nodule. Cytological diagnosis was issued as benign spindle cell lesion (where chances of a misdiagnosis as malignant are very high), thereby preventing radical surgery. It was subsequently confirmed as intra-muscular nodular fasciitis after histopathological examination.
Neck swelling, Spindle cell lesion, Fine Needle Aspiration Cytology (FNAC), Intra-muscular nodular fasciitis
Case Report
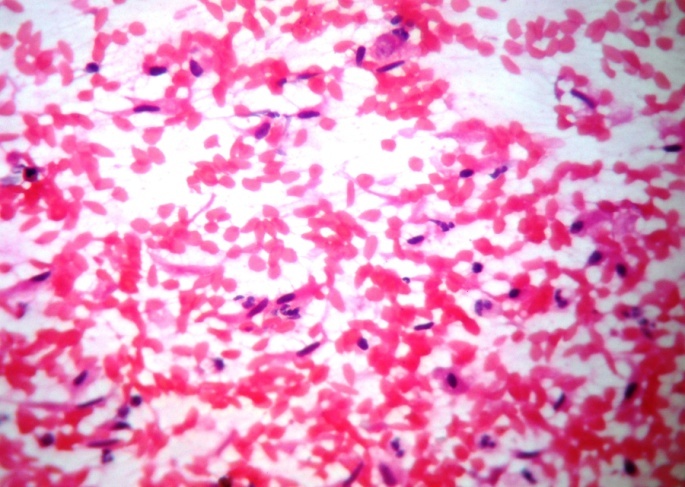
A 45-year-old lady presented with a swelling in neck of 2 months duration, to Surgical Outpatients Department. There was no significant past medical history and there was no history of any trauma. The case was referred directly to our Cytology Section, where we received a requisition letter for Fine Needle Aspiration (FNA) with a clinical diagnosis of “Solitary Thyroid Nodule –right side with a suspicion of a Thyroid Malignancy”. On examination, a slightly tender swelling was noted over right side of neck, measuring 3 × 2 cm, firm in consistency, with ill defined borders and which did not move with deglutition [Table/Fig-1]. FNA was carried out with the prior impression that the nodule originated from right lobe of thyroid and smears were prepared. Cytological examination of the multiple smears studied, showed moderately cellular smears composed of predominantly spindle cells [Table/Fig-2], having oval to spindle shaped nuclei scattered singly or in loose cohesive clusters against a haemorrhagic background. The cells had moderate amount of wispy cytoplasm. Many naked, stripped nuclei were seen. There was also sparse lymphocytic infiltration in the background. We had a suspicion of medullary carcinoma of thyroid in view of presence of spindle cells, and as we thought that the lesion arose from right lobe of thyroid; but there was neither evidence of thyroid follicular epithelial cell clusters nor of presence of colloid in the background. Cytological impression of benign spindle cell lesion was issued and a biopsy was requested, for further confirmation regarding histogenesis and further typing of lesion, as we were not sure about the origin of the lesion.
A slightly tender swelling was noted over right side of neck measuring 3X2 cm mimicking origin from right lobe of thyroid

Cytological examination showing spindle cells having oval nucleus scattered singly and loose cohesive clusters against hemorrhagic background (Pap stain, 20 X magnification)
Meanwhile, surgeon asked for a USG of the lesion, which revealed that the lesion was hypoechoic and that it measured 2.5 × 2.5 cm, without any calcification or necrotic changes, and that it arose from the lower end of sternocleidomastoid muscle. The thyroid gland was away from the lesion and it was found to be normal on imaging. The lesion was treated with local excision and it was sent for a histopathological examination.
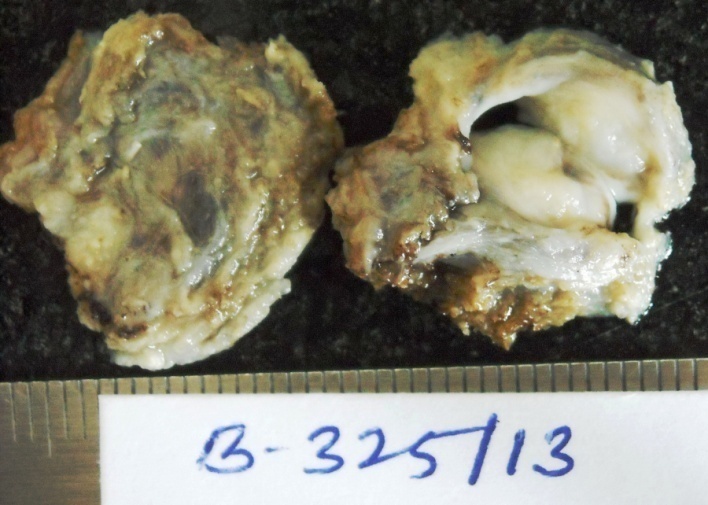
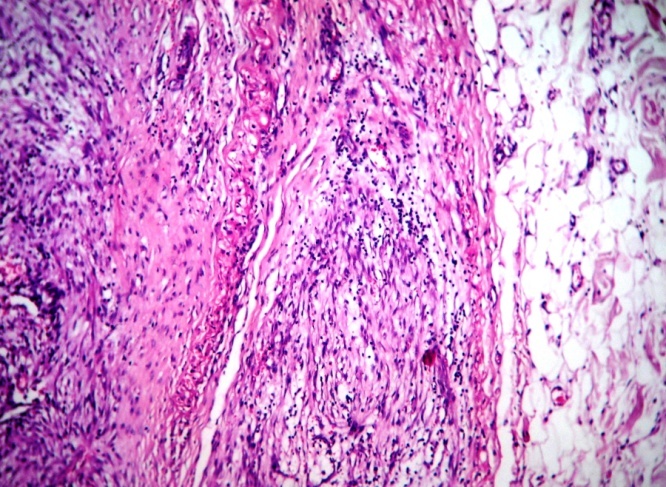
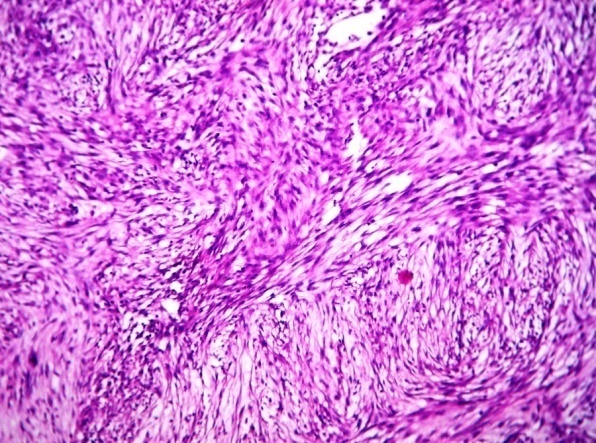
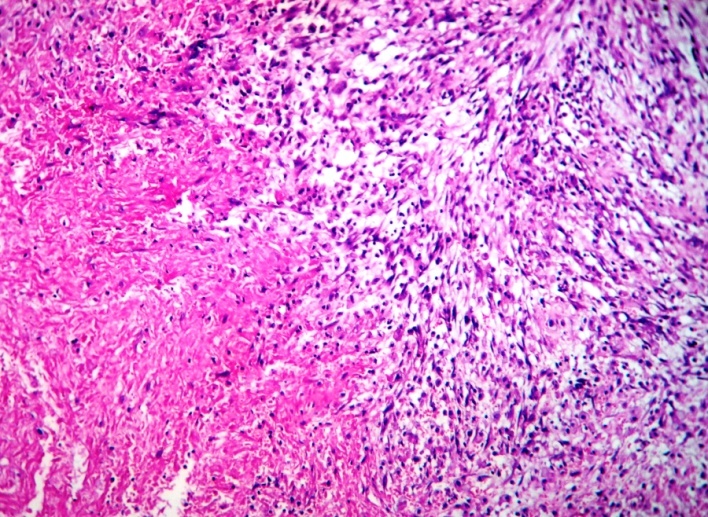
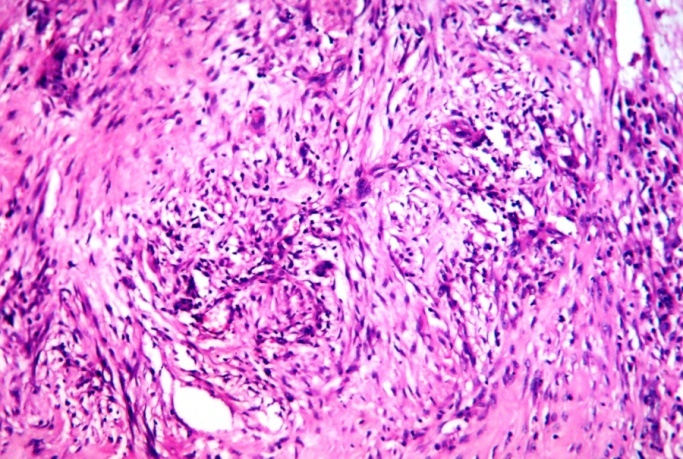
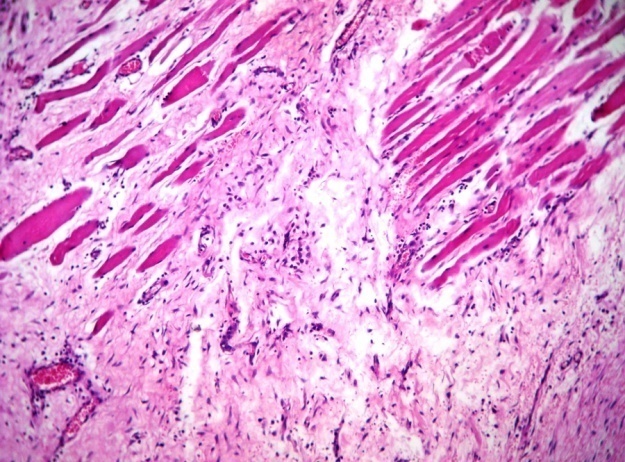
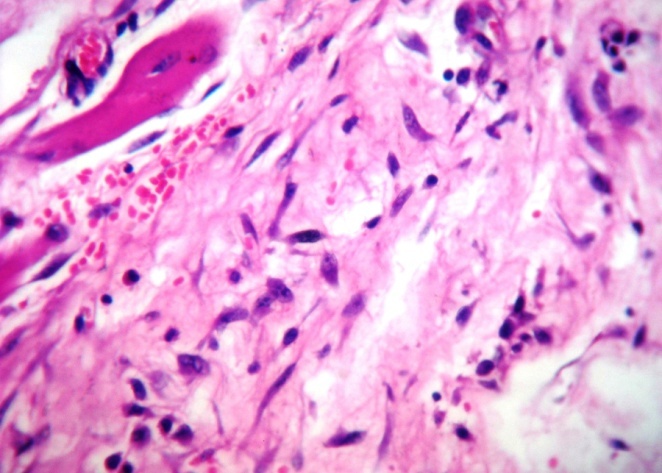
We received a nodular lesion grossly measuring 2.5 × 2.5 × 2 cm, appearing partially capsulated and surrounded by skeletal muscle fibres [Table/Fig-3]. Cut section of the lesion showed mainly gelatinous areas with foci of haemorrhages which were probably FNA induced. On histological examination, multiple sections studied showed partially encapsulated tumour [Table/Fig-4] composed predominantly of spindle to oval cells, with Storiform pattern of arrangement [Table/Fig-5] and intersecting bundles. These tumour cells were packed in the fibrocollagenous stroma which was myxoid at some foci. Sparse lymphocytic infiltration was seen to be admixed with these tumour cells. Areas of extensive necrosis and haemorrhages were noted [Table/Fig-6]. Many multi-nucleated tumour giant cells [Table/Fig-7] were also noted, especially at highly cellular areas. The tumour cells showed infiltration into the surrounding muscle fibres [Table/Fig-8], but the entire tumour lesion lay within the muscle planes. Higher magnification of tumour revealed spindle to oval cells having hyperchromatic nuclei with open chromatin and pinpoint but prominent nucleoli. Cytoplasm was scant to moderate, with tapering at the nuclear ends. Stroma showed bands of collagen as well as myxoid areas and focal extravasation of red blood cells [Table/Fig-9]. Histological diagnosis of intra-muscular Nodular fasciitis was issued and further confirmation by immunohistochemistry was advised. The six months follow-up after the resection of tumour, was uneventful.
Gross specimen: Nodular lesion appearing partially capsulated, surrounded by skeletal muscle fibres and cut section showing myxoid areas with foci of hemorrhages
Histopathological examination showing partially encapsulated Tumour composed of spindle cells with foci of lymphocytic infiltration (H & E, 10 X magnification)
Tumour composed predominantly spindle to oval cells with Storiform arrangement and intersecting bundles(H & E, 10 X magnification).
Extensive areas of necrosis and hemorrhages admixed Tumour cell clusters (H & E, 10 X magnification)
Formation of many multinucleated Tumour giant cells at the highly cellular areas (H & E, 20 X magnification)
The Tumour cells showing infiltration into the surrounding muscle fibres and the entire Tumour lesion confined within the muscle plane (H & E, 20 X magnification).
Cells displaying hyperchromatic nucleus, with open chromatin, pinpoint prominent nucleoli. Note extravasation of red blood cells in myxoid and collagenous stroma with lymphocytic infiltration (H & E, 40 X magnification)
Discussion
Nodular fasciitis is believed to occur as an unusual proliferation of myofibroblasts, triggered by local injuries or inflammatory processes. Although it is clearly a benign process, the precise cause of this proliferative lesion is unknown. The myofibroblast is thought to be the cell of origin. It was first described earlier as subcutaneous pseudosarcomatous fibromatosis. Subsequent reports confirmed the benign nature of this proliferation, and this disease was renamed as pseudosarcomatous fasciitis, which was later changed to nodular fasciitis [1]. Nodular fasciitis is defined by the World Health Organization as a benign and reactive fibroblastic growth extending from the superficial fascia into the subcutaneous tissue or muscle. The pathogenesis might involve a local reactive or inflammatory process of fibrous connective tissue [2].
Nodular fasciitis accounts for 0.025% of all pathologic diagnosis. The tumours are equally distributed between genders and are more common in the third to fifth decades of life. Lesions are small, solitary, and are commonly located on extremities, occasionally on the trunk (27–29%), followed by the back and chest wall (15–18%) and the upper arm (12%). They occurvery rarely in the head and neck region [2].
Nodular fasciitis occurs in three forms: Sub–cutaneous, fascial and intra-muscular. The sub–cutaneous form is most common, followed by the fascial form, with the intra-muscular form being the least common. The sub–cutaneous form occurs three to ten times more commonly than the other subtypes and it typically presents as a sub–cutaneous nodule. The intra-muscular form is typically larger in size and therefore, as a result of its size and deep location, it is clinically more likely to suggest a soft tissue malignancy. The fascial form is less well-circumscribed, similar to the intra-muscular form, and it may have a stellate appearance as a result of its growth pattern [2].
Diagnosis of Nodular fasciitis is very challenging, and it is often mistaken for a sarcoma because of its rapid growth, rich cellularity, and high mitotic activity, poorly circumscribed nature, which may result in it being easily misdiagnosed as a sarcomatous lesion like malignant fibrous histiocytoma or fibrosarcoma [3,4]. Diagnosis of Nodular fasciitis is very challenging, especially on cytological smears. However, in our case, the cellularity was less and features of anaplasia were not evident on cytology smears. Hence, we safeguarded our self by calling the lesion as a benign spindle cell lesion and requested a histopathological confirmation. Radiologic imaging modalities such as ultrasonography and computed tomography are helpful in locating the exact tumour site and in differentiating solid and cystic nature of the lesion [5]. In our case, cytology report as well as USG neck report helped the surgeon to carry out a simple resection of the tumour, thus avoiding radical surgery.
Complete, local excision is usually curative; local recurrences are rare [6]. In fact, local recurrence is so rare that it should prompt a reevaluation to confirm the diagnosis. Metastases do not occur. Response to intralesional steroid injections has also been reported [7].
Conclusion
Cytological diagnosis of nodular fasciitis shows spindle shaped mature fibroblastic cells scattered singly, along with occasional degenerated and multinucleated giant cells in a clean or haemorrhagic background. It is important to differentiate this lesion from different forms of spindle cell lesions. False positive diagnosis as fibrosarcoma is possible, due to presence of cytological anaplasia, which can be avoided by having awareness about various histological facets of nodular fasciitis. Fine-Needle Aspiration Cytology (FNAC), as a time saving, rapid and reliable diagnostic procedure, has got a bigger role to play in reassurance of anxious patients, for guiding surgeon for conservative management and for avoiding radical surgeries. Radiological investigations like USG reports, prior to FNA, are of great help to pathologist, for avoiding misdiagnoses of these lesions as malignant ones. Histopathological confirmation is mandatory for challenging lesions like nodular fasciitis and pathologists should be aware about nuclear atypia encountered in this reactive process.
[1]. Nishida Y, Tsukushi S, Wasa J, Iwata Y, Nodular Fasciitis of the Finger and Hand: Case ReportJ Hand Surg 2010 35A:1184-86. [Google Scholar]
[2]. Enzinger F, Weiss SW, Benign fibrohistiocytic Tumours. In: Weiss SW and Goldblum JR, edsSoft Tissue Tumours 2001 4th edSt. LouisMosby:441-90. [Google Scholar]
[3]. Mallina S, Rosalind S, Philip R, Harvinder S, Nodular Fasciitis: A Diagnostic DilemmaMed J Malaysia 2007 62(5):420-1. [Google Scholar]
[4]. Plaza JA, Mayerson J, Wakely PE, Nodular fasciitis of the hand: a potential diagnostic pitfall in fine-needle aspiration cytopathologyAm J Clin Pathol 2005 123:388-93. [Google Scholar]
[5]. Subramaniam P, Balakrishna R, Mahendra P, Gilhotra K, Nodular fasciitis of the oro-facial regionContemp Clin Dent 2012 April 3(Suppl1):S16-S18. [Google Scholar]
[6]. Stanley MW, Skoog L, Tani EM, Nodular fasciitis: spontaneous resolution following diagnosis by fine-needle aspirationDiagn Cytopathol 1993 9:322-24. [Google Scholar]
[7]. Hornick JL, Fletcher CD, Intra–articular nodular fasciitis—a rare lesion: Clinicopathologic analysis of a seriesAm J Surg Pathol 2006 30:237-41. [Google Scholar]