UTIs are the most common serious bacterial infections which are seen during infancy [1]. Prevalence of UTIs is 1-3% in girls and it is 1% in boys [2]. Paediatric UTI are associated with high morbidity and long term complications like renal scarring, hypertension and chronic renal failure [3]. The diagnosis of UTIs is difficult in the neonatal period, because the signs and symptoms are non-specific in this age group. Renal calculi, obstructive uropathy (posterior urethral valves), vesicourethral reflux and voiding disorders can lead to urinary stasis and they may predispose to the development of recurrent UTIs and their complications [4].
Materials and Methods
The present retrospective study was carried out in the Department of Microbiology for a period of 3 years, from January 2007 to December 2010. A total number of 1575 urine samples from children who were suspected of having UTIs were received from among both inpatients as well as outpatients who approached our hospital, Smt. Kashibai Navale Medical College and General Hospital, Narhe, Pune, India. Samples were midstream urine specimens, catheterized urine samples and supra pubic aspirates. Screening of urine for significant bacteriuria was done by gram staining the samples. Urine culture was done by a semi-quantitative technique. Urine (0.001ml) was cultured by using a calibrated bacteriological loop on blood agar and Mac Conkey’s agar. Recommendations of Kass [6] were followed, for distinguishing active UTIs from contaminations. Presence of 105 bacteria/ml of urine indicated an active urinary infection and so, this level was called significant bacteriuria. After an overnight incubation at 37°C, number of colonies which were obtained were counted and they were multiplied by 1000, to obtain the colony forming units (cfu)/ml. For suprapubic samples, any numbers of colonies were considered as significant [7].
Isolates were identified by gram staining, motility tests and routine biochemical reactions. Antibiotic sensitivity was performed by using Kirby Bauer disc diffusion method by following the Clinical Laboratory Standards Institute (CLSI) guidelines [8]. All Enterobacteriaceae and Acinetobacter spp. were tested against the first line agents: amikacin (30μg), ampicillin (10μg ), cefotaxime (30μg), trimethoprim-sulphamethoxazole(1.25-23.75μg), gentamicin (10μg), nitrofurantoin (300μg), norfloxacin (10μg) and doxycycline (30μg). For gram positive cocci, penicillin (1U), cefazolin (30μg), ciprofloxacin (5μg), nitrofurantoin (300μg), norfloxacin (10μg), doxycycline (30μg), vancomycin (30μg), teicoplanin (30μg) were used. Pseudomonas aeruginosa was tested against amikacin (30μg), gentamicin (10μg), ceftazidime, (30μg), carbenicillin (100μg) piperacillin (100μg) and ciprofloxacin (5μg). Second line antibiotics were tested only for organisms who were resistant to all 1st line antimicrobials or if it was specifically requested for by the attending physician. These included; imipenem (10μg), cefepime (30μg), ofloxacin (5μg) and piperacillin-tazobactam (100/10μg). Extended spectrum β lactamase (ESBL) production in Escherichia coli and Klebsiella pneumoniae was tested as per CLSI guidelines [8]. For all Enterobacteriaceae, Acinetobacter spp. and Pseudomonas isolates, E. coli ATCC 25922, E. coli ATCC 35218 and P. aeruginosa ATCC 27853 were used as controls.
Results
Out of the 1575 clinical specimens which were tested, 390 were culture positive (24.76%), 444 showed insignificant growth of organisms, i.e., due to contamination of urine samples and 741 were culture negative.
Overall, infection rate was higher in 0-1 year age group among males [Table/Fig-1]. Among females, the infection rate was higher in the age group of 6-12 years.
Age distribution in males and females with UTI
| Age groups (months/years) | Sex (No., %) | Total (No., %) |
|---|
| Males | Females |
|---|
| 0-1 | 101 (25.89) | 46 (11.79) | 147 (37.7) |
| 2-5 | 58 (14.87) | 72 (18.46) | 130 (33.3) |
| 6-12 | 40 (10.25) | 73 (18.71) | 113 (29) |
| Total | 199 (51.03) | 191 (48.97) | 390 (100) |
Escherichia coli (45.12%) was the commonest uropathogen which was isolated in all age groups, followed by Klebsiella species (18.71%) and Enterococcus species (9.23%) [Table/Fig-2].
Organisms isolated in different age groups
| Organisms | 0-1 | 2-5 | 6-12 | Total (%) |
|---|
| Escherichia coli | 74 | 54 | 48 | 176(45.12) |
| Klebsiella species | 40 | 17 | 16 | 73(18.71) |
| Enterococcus species | 15 | 12 | 09 | 36(9.23) |
| Pseudomonas species | 02 | 06 | 10 | 18(04.61) |
| Citrobacter species | 03 | 12 | 03 | 18(04.61) |
| Acinetobacter species | 02 | 06 | 09 | 17(04.35) |
| Streptococcus species | 01 | 05 | 10 | 16(04.10) |
| Proteus species | 03 | 07 | 04 | 14(03.58) |
| Staphylococcus aureus | 01 | 07 | 03 | 11(02.82) |
| Candida species | 06 | 03 | 01 | 10(02.56) |
| Salmonella typhi | 00 | 01 | 00 | 01(0.25) |
| Total | 147 | 130 | 113 | 390 |
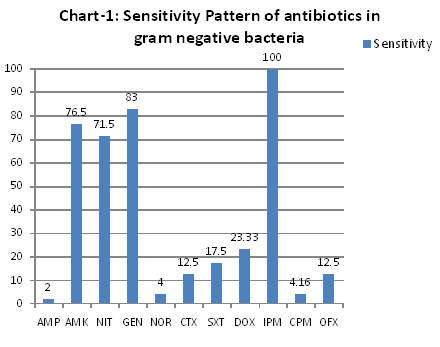
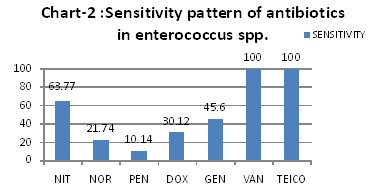
Antibiotic susceptibility pattern among gram negative bacilli was as shown in [Table/Fig-3]. Among the first line antibiotics, higher sensitivity was observed against gentamicin, amikacin and nitrofurantoin. Maximum resistance was seen against ampicillin and norfloxacin. Among the second line antibiotics, all strains were sensitive to impenem. ESBL positivity was 6% in Escherichia coli and Klebsiella spp. Among Enterococci, resistance was not seen with vancomycin and teicoplanin (100% sensitivity) and a higher susceptibility was observed with nitrofurantoin (63.77%) [Table/Fig-4].
Sensitivity pattern of antibiotics in gram negative bacteria
[AMP= Ampicillin, AMK= Amikacin, NIT= Nitrofurantoin, GEN= Gentamicin, NOR= Norfloxacin, CTX= Cefotaxime, SXT= Co-trimoxazole, DOX= Doxycycline, IMP=Imipenem, CPM= Cefepime, OFX= Ofloxacin]
Sensitivity Pattern of antibiotics in Enterococcus spp.
[NIT= Nitrofurantoin, NOR= Norfloxacin, PEN= Penicillin, DOX= Doxycycline, GEN=Gentamicin, VAN=Vancomycin, TEICO= Teicoplanin]
Discussion
UTIs are one of the most common bacterial diseases in infants and children. Our hospital also caters to a significant number of children who present with UTIs, which could be estimated from 24.76% culture positivity which was seen in our study.
Frequency of UTIs in children varies according to age and sex. According to previous reports, [2,5,7] incidence of UTIs was highest in the first year of life. In the present study also, maximum infection (37.7%) was observed in the first year of life. A female preponderance with a male to female ratio of 1:10 has been reported in patients with UTIs, who were aged beyond 1-2 years [5,9]. In our study also, females were affected more after the first year of life.
Gram negative organisms are the most commonly isolated organisms, with Escherichia coli (E. coli) accounting for 70 to 90% of infections [10]. In our study, Escherichia coli (45.12%), followed by Klebsiella species (18.71%) and Enterococcus species (9.23%), were isolated from most of the samples. Similar results were observed in other studies also [7,11,12].
There is a trend towards increasing resistance to the commonly used antimicrobial agents for the treatment of paediatric UTIs. In our study, antibiotic susceptibility which was seen against the gram negative uropathogens showed high resistance to ampicillin (98%), norfloxacin (96%) and co-trimoxazole (82.5%). They showed low resistance to gentamicin (17%), amikacin (23.5%) and nitrofurantoin (28.5%). These findings signified that ampicillin and co-trimoxazole which were commonly used for empirical therapy were now showing resistance in our region. This may be due to selection pressure of antibiotics. The studies from various regions, which were done during the past few years, also showed similar resistance patterns among uropathogens which caused paediatric UTIs [1,10–17].
Among gram positive organisms, Enterococcus spp (9.23%) were predominant isolates. All Enterococcus spp. strains were sensitive to vancomycin and teicoplanin (100%). A higher susceptibility was seen against nitrofurantoin (63.77%). These results were consistent with those of Rudy M et al., [16] and Miskeen PA et al., [18] studies.
Thus, results of our study indicated that the presence of Escherichia coli as the aetiological agent and as a major uropathogen in children had not changed. But antibiotic susceptibility pattern had markedly changed. Drugs which were frequently used in the treatment of UTIs were now showing considerable resistance. This may have happened due to selection pressure of antibiotics. To avoid this situation, surveillance of antibiotic resistance patterns should be done periodically and an antibiotic policy should be made accordingly, for a better patient management.
Conclusion
This study concludes that E.coli is the predominant aetiological agent of UTIs which are seen in children. Ampicillin and co-trimoxazole which are commonly given as empirical treatment are now showing increased resistance. Due to low resistance to nitrofurantoin, amikacin and gentamicin, these may be considered as alternative drug therapies. Thus, trend of antibiotic susceptibility pattern should be detected periodically, to select the appropriate regimen for the treatment of UTIs.