Depression is not a normal ageing process and it poses a serious public health problem. The phenomenology and aetiology of geriatric depression are very heterogeneous and they range from biological to social, environmental, interpersonal and psychological factors. Depression not only complicates the chronic diseases among the elderly group, but also leads to higher functional impairment and disability, increased expenditure on health and increased mortality [4]. This underlies the need for the provision of mental health care at primary and secondary levels, for a better access to services and increased outreach, which involves various degrees of integration. It is necessary to provide holistic and continuous patient care within and between levels of care. One of the models is “Mental health at primary health care”-wherein the services are located on site but are not integrated with general health care services [5].
This study was undertaken in such a setting, to estimate the proportion of depression in the middle aged and elderly populations which attended a rural health care setting, to find whether there was a significant difference between the middle aged and elderly populations and to find the factors which were associated with depression and presence of co-morbidities with depression.
Methods
Nitte Rural Psychiatry project is being run by an expert team of psychiatrists from the Department of Psychiatry, K S Hegde hospital since 2007 in a rural area of Karkala taluk. The services which are provided here include outpatient consultancy by trained psychiatrists which is assisted by a psychologist, with a provision of free drugs, referral services for hospitalization, family support and counselling services, community rehabilitation, field surveys, health education and other community based activities which are conducted by a psychiatry social worker, psychologist and a community nurse.
A secondary descriptive analysis of the data that has been maintained in the form of outpatient records at the centre was undertaken while maintaining complete anonymity of the patients. The basic socio-demographic data like age, gender, socio economic status, religion, education and occupation, along with the details of psychiatric diagnosis, associated co-morbidity and substance abuse or dependence, if any, were collected. The study was conducted for a period of 2 months from August to September 2011 and the study subjects included all the middle aged and elderly adult patients who attended and were diagnosed with depression/dysthymia. Patients with diagnoses other than depression/ dysthymia and who were not of the requisite age group were excluded. Elderly were defined as persons who were aged 60 years; young old, middle old and old old were defined as persons who were aged 60-69 years, 70-79 years and above 80 years respectively and the middle aged were defined as persons who were aged 41-59 years.
Data was entered and managed in Excel and the analysis was done by using SPSS, version 17.0. The statistical analyses done were: percentages for proportions, Chi square test for correlates of depression in elderly adults and Z-test for comparison of depression between the two groups of study population.
Results
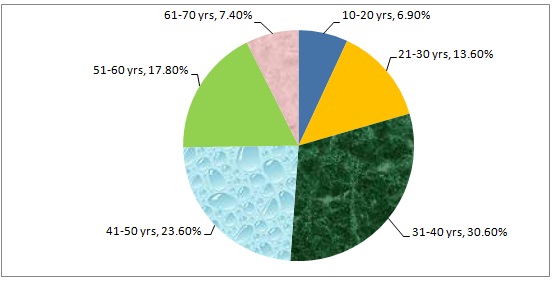
Among all the persons who attended the OPD, depression was the most common diagnosis, with 350 cases (32.3%), followed by schizophrenia (11.6%) and alcohol dependence (9.8%). As shown in [Table/Fig-1], proportion of depression was highest (30.6%) among those aged 31-40 years and least (6.9%) in those aged 10-20 years.
The most common diagnoses among the elderly were mood disorders (40%), with depression being the most common among the mood disorders (86%). The proportion of depression among the middle aged was 126 cases (28.97%); among which 88 cases were females (69.84%) and 38 were males (30.15%). The proportion of depression/dysthymia among elderly age group was 62 cases (36.47%); among which 40 cases were females (64.5%) and 22 cases were males (35.48%). Z-value which was calculated with a p value of 0.05 was 3.98; there was a significant difference in the proportion of depression among the elderly and the middle aged groups.
Among the elderly who were diagnosed with depression/dysthymia, a majority 39 (62.9%) were married, while 21 (33.9%) were widows/widowers. A majority of the elderly depressed patients were Hindus (95.2%), unoccupied (74.2%), educated up to primary school (74.2%) and belonged to lower socio economic class (82.35). Seven patients consumed alcohol, among which one was a case of dependence. Five were beedi smokers and eight were pan chewers (one case was of nicotine dependence). A majority (56.5%) of the depressed elderly patients had no co-morbidities. Hypertension was the most common co-morbidity among the rest (19.4%) of the patients.
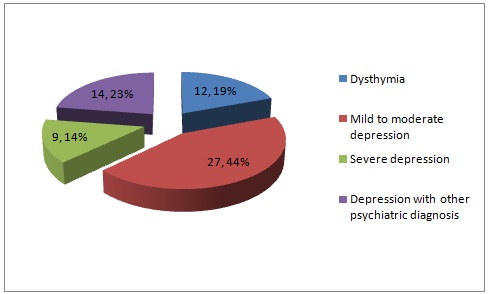
As shown in [Table/Fig-2], most of the elderly depressed patients suffered from mild to moderate depression (47%) and the next common diagnosis was dysthymia (19%). There were seven cases of psychotic depression, one case of depression with panic disorder and one case of depression with Alcohol Dependence Syndrome (ADS).
According to [Table/Fig-3], age and gender were significantly associated with the presence of depression. Depression was more common among the young old and females. As shown in [Table/Fig-4], age and gender showed a significant association with the presence of co-morbid conditions among those elderly who were diagnosed with any form of depression or dysthymia. Males and the young old with depression were more likely to suffer from co-morbid medical conditions.
Distribution of all diagnosed depression cases according to age
Distribution of the elderly population according to types of depression
Socio- demographic factors associated with depression
| Socio Demographic Factors | Diagnosis | Total | | p value |
|---|
| Any Form of Depression/Dysthymia | No Depression |
|---|
| Age group (in years) | 60-69 | 40 (58.8%) | 68 (62.9%) | 108 (63.5%) | X2=8.494 | 0.000 (Highly significant) |
| 70-79 | 25 (47.2%) | 28 (52.8%) | 53 (31.2%) |
| 80 and above | 1 (11.1%) | 8 (88.9%) | 9 (5.3%) |
| Total | 66 (38.8%) | 104 (61.2%) | 170 |
| Gender | Male | 22 (33.3%) | 44 (66.7%) | 66 (38.8%) | X2=8.49 | 0.004 (Highly significant) |
| Female | 44 (42.3%) | 60 (57.7%) | 104 (61.2%) |
| Total | 66 (38.8%) | 104 (61.2%) | 170 |
Socio–demographic factors associated with co–morbid conditions in the depressed elderly
| Socio Demographic Factor | Co-Morbid Medical Conditions | Total | | p value |
|---|
| Present | Absent |
|---|
| Gender | Male | 9 (40.9%) | 13 (59.1%) | 22 (35.5%) | X2=16.516 | .022 (significant) |
| Female | 6 (15%) | 34 (85%) | 40 (64.5%) |
| Total | 15 (24.2%) | 47 (75.8%) | 62 |
| Age group (in years) | 60-69 | 9 (23%) | 30 (77%) | (62.9%) | X2 = 35.065 | .000 (Highly significant) |
| 70-79 | 6 (27.3%) | 16 (72.7%) | 22 (35.5%) |
| 80 and above | 0 | 1 (100%) | 1 (1.6%) |
| Total | 15 (24.2%) | 47 (75.8%) | 62 |
Discussion
Mood disorders were the most common diagnoses among elderly patients in the present study, with depression alone contributing to 86% of the mood disorders. In the present study, elderly patients were more likely to suffer from depression as compared to the middle aged. This difference was statistically significant; this was similar to findings of other studies which were done among geriatric patients in psychiatry healthcare and old age homes [6–8]. However, some studies [9] found that a majority of the patients with psychiatric morbidity were in the age group of 16-45 years and that most were suffering from severe mental illness; of which bipolar affective disorder (45%) and schizophrenia (35.9%) were the two most common ones. This may point to a trend where depressive disorders are more common in elderly and psychotic disorders are more common in the young. However, there are yet some studies [7, 10] which concluded that there was no gradual increase in psychiatric morbidity with age.
The socio-demographic profiles of the elderly depressed patients in the present study showed that a majority of the depressed elderly patients were married and educated up to primary school and that they belonged to lower socio economic statuses. This was similar to the findings of other studies [6,7]. However, the present study did not explore into associations between these socio-demographic factors in detail and hence, definite conclusions cannot be drawn as to the statistical significance of this observation.
The prevalence and pattern of co-morbidities among elderly depressed patients who attended primary care in our study were similar to those which were seen various other studies [6–8], with hypertension and diabetes being the most common co-morbidities. The presence of co-morbidities may lead to disabilities which further the depression. In the present study, young old and males were more likely to have co-morbid conditions with depression. When chronic diseases are experienced at younger age groups, the resultant disability may contribute to the development of depression. Similar results have been found in other studies in various settings [11].
Earlier studies [11, 12] which were done on depression among the elderly in primary care settings showed prevalence to range from 5 to 10%, which was much lower than ours; the reason could probably be that our study was conducted in a community mental health setting with integration of mental health into primary care, which may have led to a higher intake of depressed and mentally ill elderly patients. Also, recent studies which have been done on integration of mental health into primary health care settings are fewer in Indian set up, though community based studies are there in plenty. Studies which were done on psychiatry tertiary care in India have shown comparable prevalence rates as in the present study [6, 7].
The present study showed a significantly higher prevalence of depression in females, which was corroborated by other studies [10, 12, 13] though there are some hospital based studies [14] that showed that depressed and non–depressed patients were not significantly different with regards to gender. The present study found that mild to moderate depression and dysthymia were the most common forms of depression, which was in contrast to thefindings of a study which was done on primary care [10], which showed that major depression (6.5%) was more common than minor depression (5.2%) and dysthymia (0.9%).