Intra-ocular calcifications can occur due to a variety of reasons. In cataract, the lovely lens gets calcified and the bright beautiful world becomes dark and dreadful. Cataract comes in various forms like; congenital, traumatic and senile. Asteroid Hyalosis (AH) occurs because of the accumulation of calcium soaps in vitreous of the eyes. Although it is asymptomatic and unilateral, it is seen more often in diabetic patients. Tumours of eye like retinoblastoma and optic nerve meningioma too are known to show calcifications. This review has focussed on imaging appearances of intra-ocular calcifications, a small process in a small organ that nevertheless has a wide impact on the entire organs.
Intraocular calcifications, Cataract, Asteroid Hyalosis, Retinoblastoma, Meningioma
Introduction
We all can enjoy the beauties of the world so long as our eyes are away from dreaded calcifications – their processes and determinants. But once calcification sets in any part of the eye; it is bound to make its presence felt.
The three main ways in which the intra-ocular calcifications manifest in our eyes are: Cataract, AH and Calcifications in tumours related to eye.
Cataract
A cataract is defined as an abnormal opacity of any portion of the lens, regardless of visual acuity. In some advanced cases of cataracts in which good fundus visualisation is not possible, an ultrasound examination provides better assessment of the posterior segment of the globe.
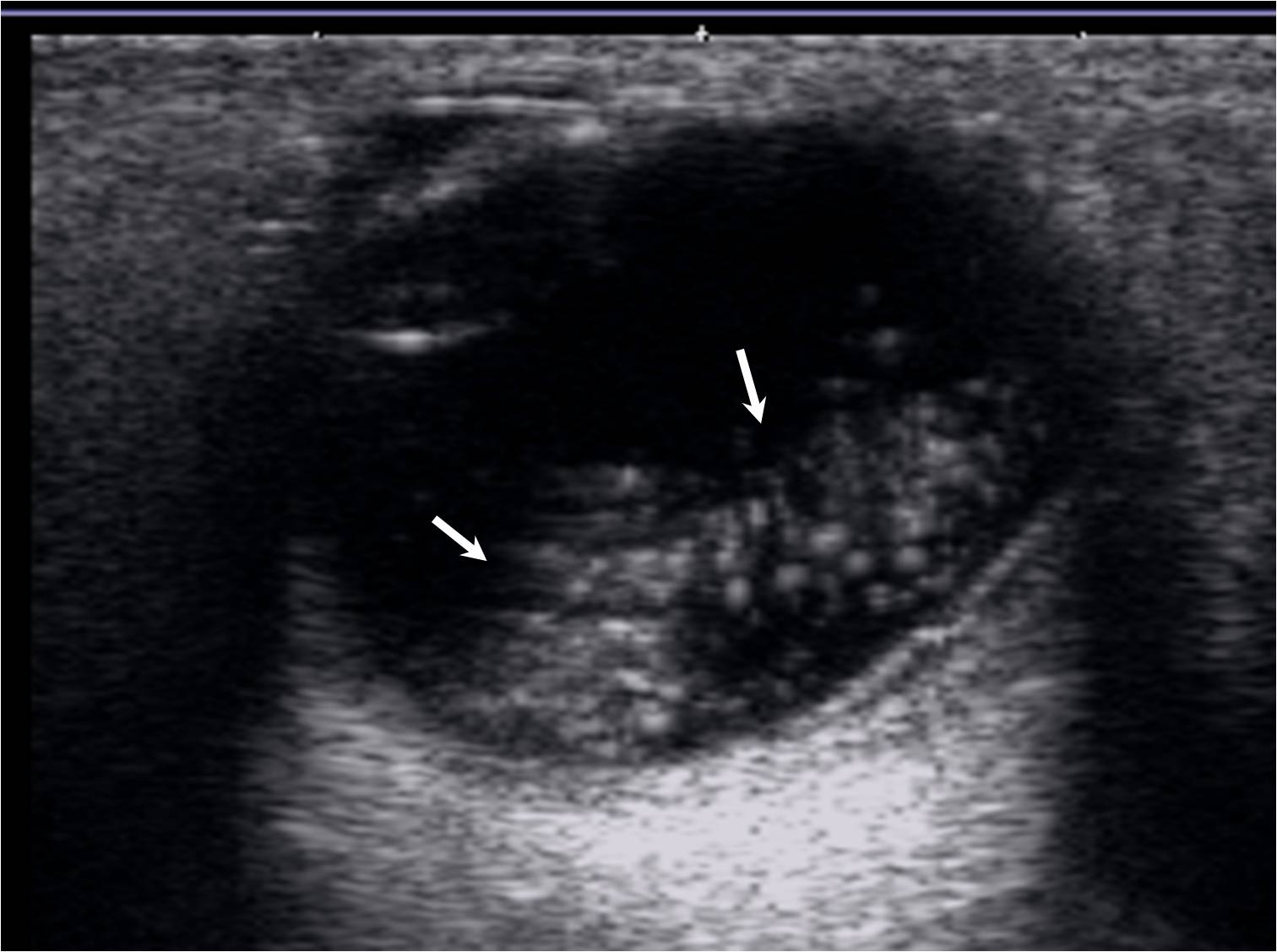
On ultrasound; a cataractous lens appears swollen than normal and it becomes echogenic due to calcification. Common causes of cataract are Congenital eg. TORCHeS infections [Table/Fig-1], Senile or Degenerative or Age related changes [Table/Fig-2] or a Post traumatic sequel as a result of dislocation [Table/Fig-3].
B Scan showing Bilateral Congenital Cataract
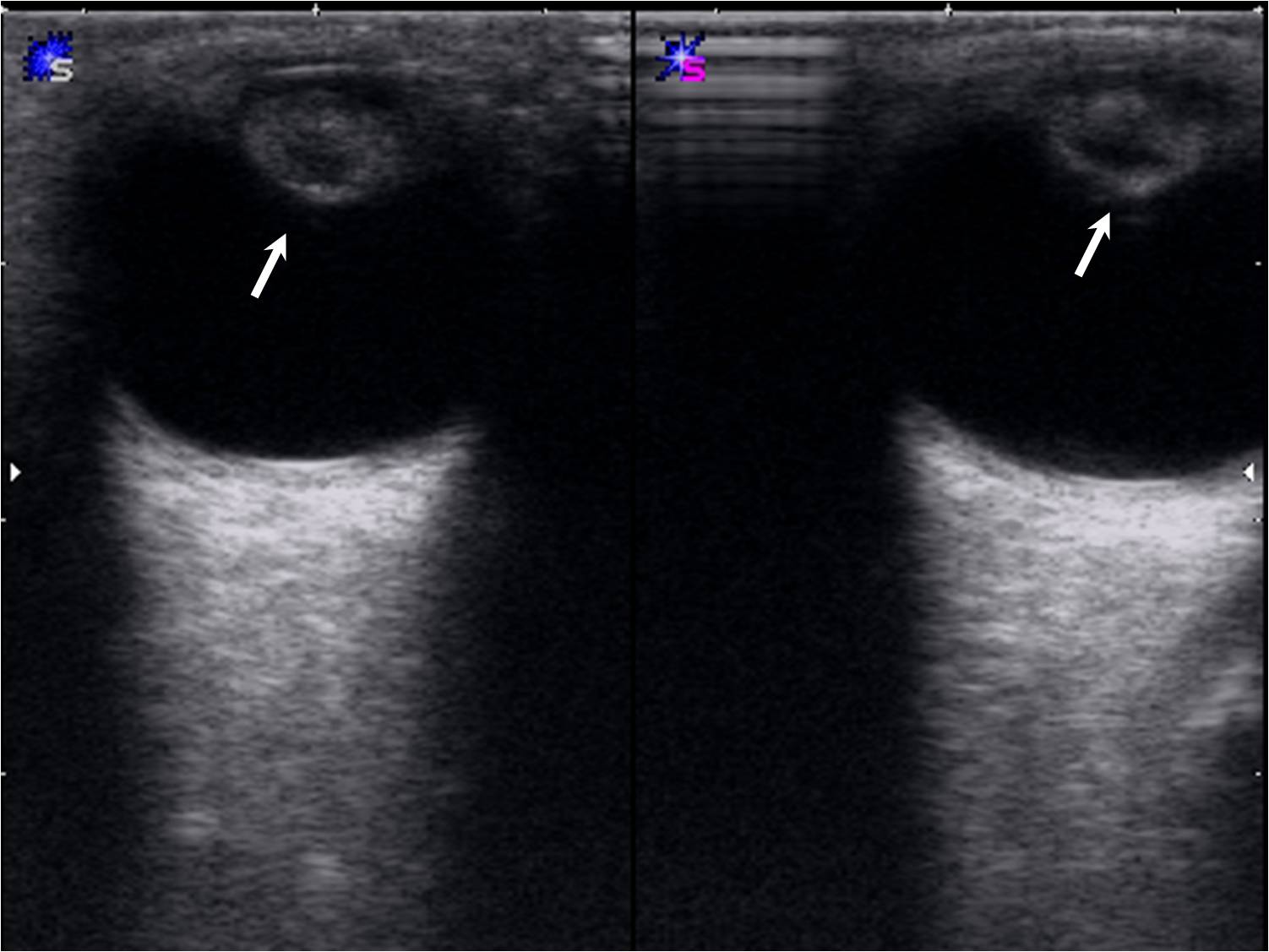
B Scan showing Bilateral Senile Cataract
B Scan showing Post traumatic dislocated Cataractous Lens
It is the primary cause of reversible blindness all over the world [1–3]. A number of factors stand in the way of treatment for cataract; prominent among them being emotional factors [4]. Ultrasonographic evaluations are often used in cataract campaigns and it is particularly indicated in cases in which the posterior pole cannot be examined through normal optometric methods.
Ultrasound is a non-invasive, painless imaging method that can be done at a doctor’s clinic on adults as well as children [5]. Ultrasonic evaluation of the posterior segment in patients with opacities is vital, to determine the most suitable type of surgery [6, 7].
Ultrasound not only diagnoses cataract, but it also reveals in the eye, abnormalities that could compromise the function of the eye after surgery. The most common of these abnormalities are vitreous opacities (12.1%), followed by retinal detachment (9.3%). The patients with these anomalies should not be considered for cataract surgery and they should be guided to adequate treatment for the detected disease. Thus, preoperative ultrasonography has a definitive role of in patients with dense cataracts [8–10].
Asteroid Hyalosis
AH is the occurrence of calcium soaps suspended in the vitreous of one or both eyes. Although invisible to the naked unaided eye, non-invasive Ocular Ultrasound and Fundoscopy can demonstrate them beautifully.
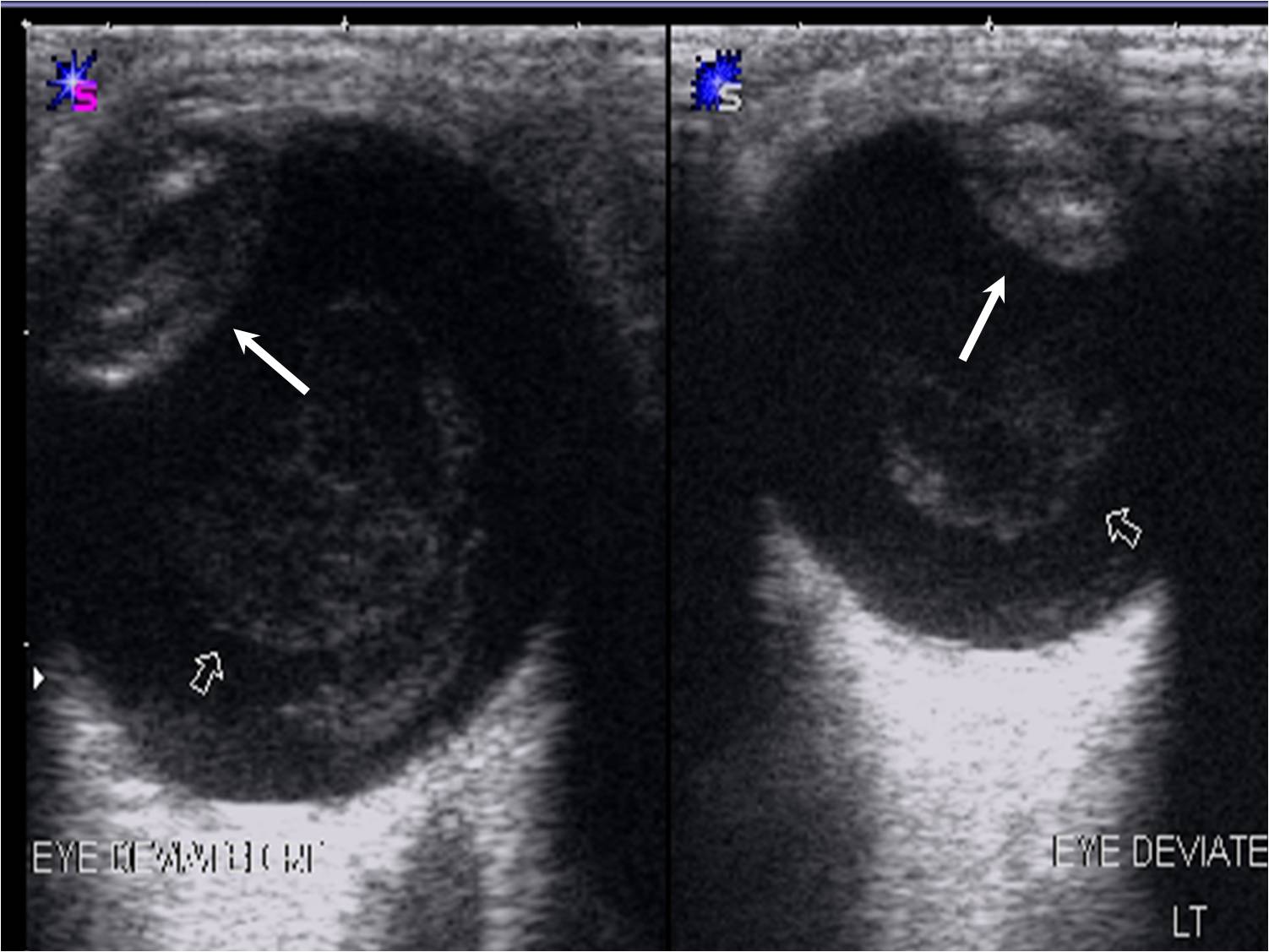
High spikes are seen on the A scan vector. On B scan imaging [11–20], normal posterior segment of eye appears clean and echo free [Table/Fig-4]. In presence of AH, discrete mobile points like bright echoes without any posterior acoustic shadowing [Table/Fig-4] and which have considerable after movements [Table/Fig-5] are seen in the vitreous. The media appears hazy on fundoscopy and AH is seen as shiny highly refractive bodies in the vitreous. Although the exact aetiology is unknown, it has been reported in 30 -70% of diabetics [11, 20].
On B scan, normal vitreous is echo free as seen in left eye, whereas the Asteroid Hyalosis is seen as bright echoes in vitreous in right eye
B Scan showing after movements of Asteroid Hyalosis following eye movement
Although it usually causes no severe visual disturbances, its health impacts can be considerable when it exists in association with other local abnormalities like cataract or degenerative changes.
Calcifications in Ocular Tumours
Retinoblastoma is a small round-cell tumour of neuroepithelial cell origin, and the commonest childhood intraocular malignancy [21, 22]. Approximately 200 cases are diagnosed per year in the United States. The average age at diagnosis is 18 months, with 80% of cases occurring before age of 3-4 years [21]. Approximately 30% of cases are bilateral and they are typically diagnosed earlier than unilateral cases. Lesions may be synchronous, metachronous, unifocal, or multifocal. Most (90%) new cases of retinoblastoma are sporadic and only 10% are inherited. Inherited retinoblastoma has an autosomal dominant pattern of inheritance, with 80-100% penetrance. Sporadic lesions usually result from spontaneous mutations [21].
Diagnosis is typically made by doing an ophthalmologic examination, being prompted by leukocoria or “white reflex” [21,23], which is seen in 60% of patients [23]. Leukocoria is associated with large tumours or total retinal detachment [21]. Until recently, imaging techniques have lacked resolution capabilities that could approach an ophthalmologic examination.
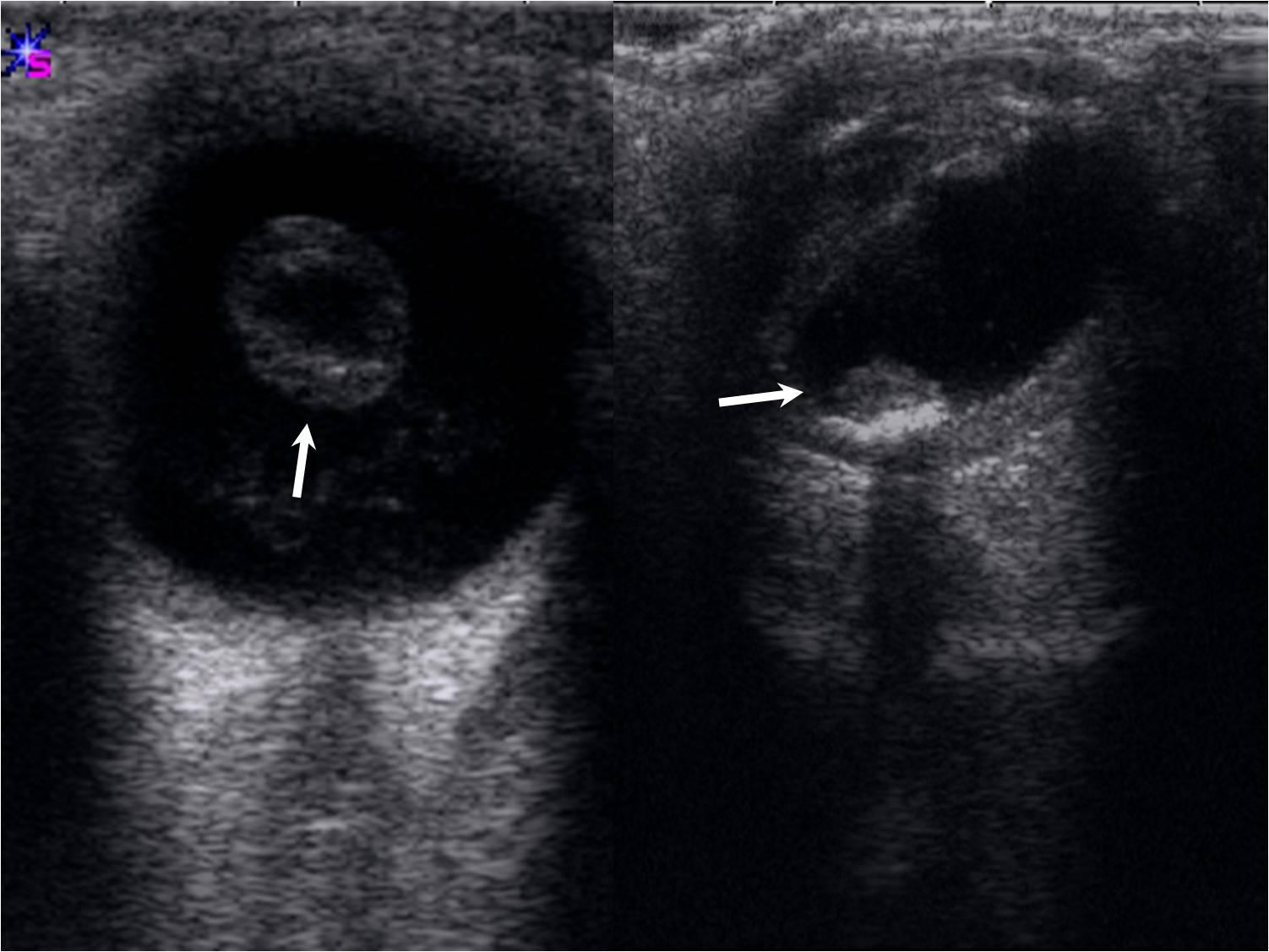
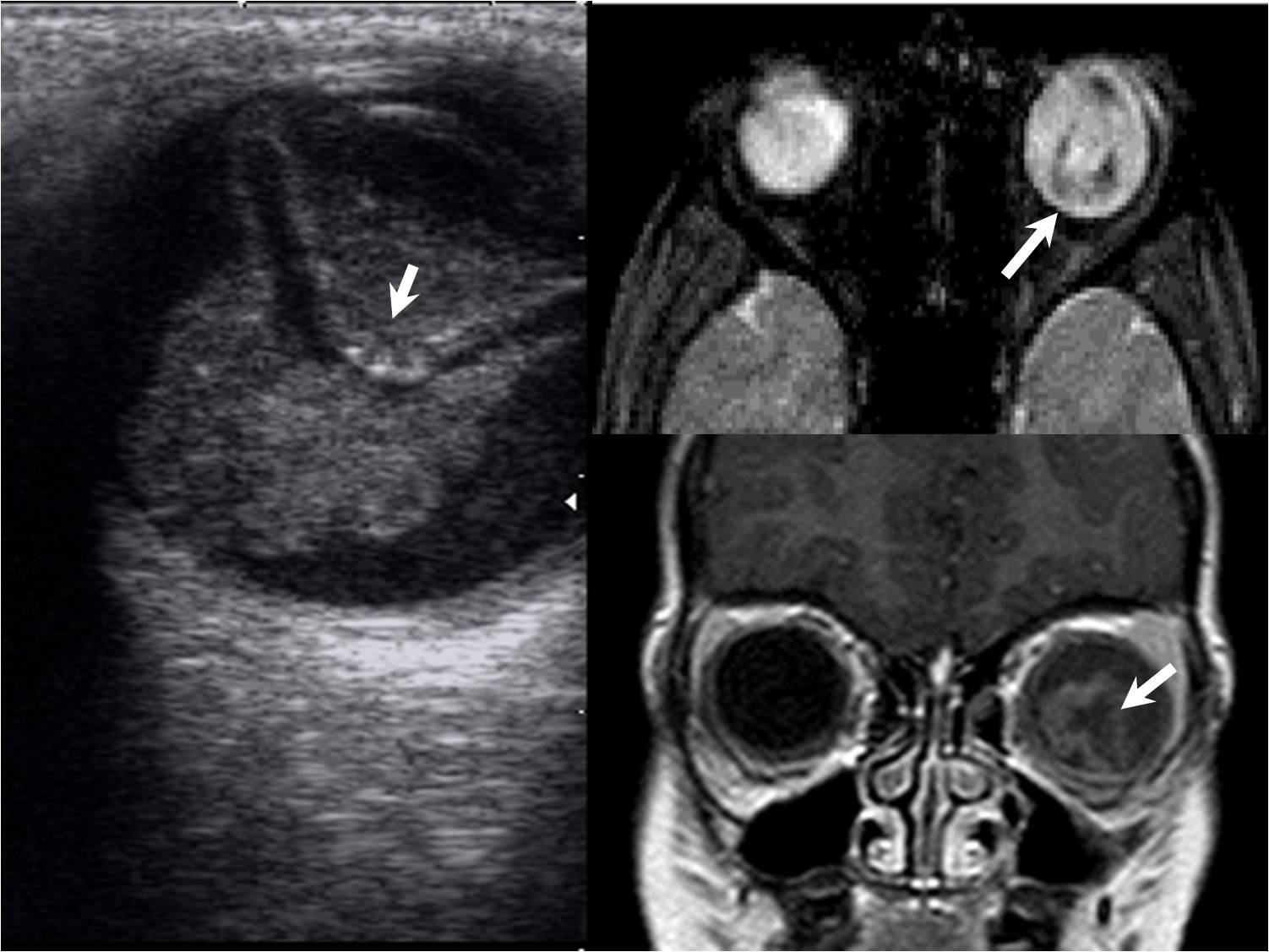
On high resolution ultrasound [Table/Fig-6], the tumour appears as an echogenic soft-tissue mass with various degrees of calcification [22]. MR imaging [Table/Fig-6] or CT best delineates the resulting intracranial spread [21]. Colour Doppler imaging can identify and monitor tumour viability.
USG and MRI showing calcifications in Retinoblastoma
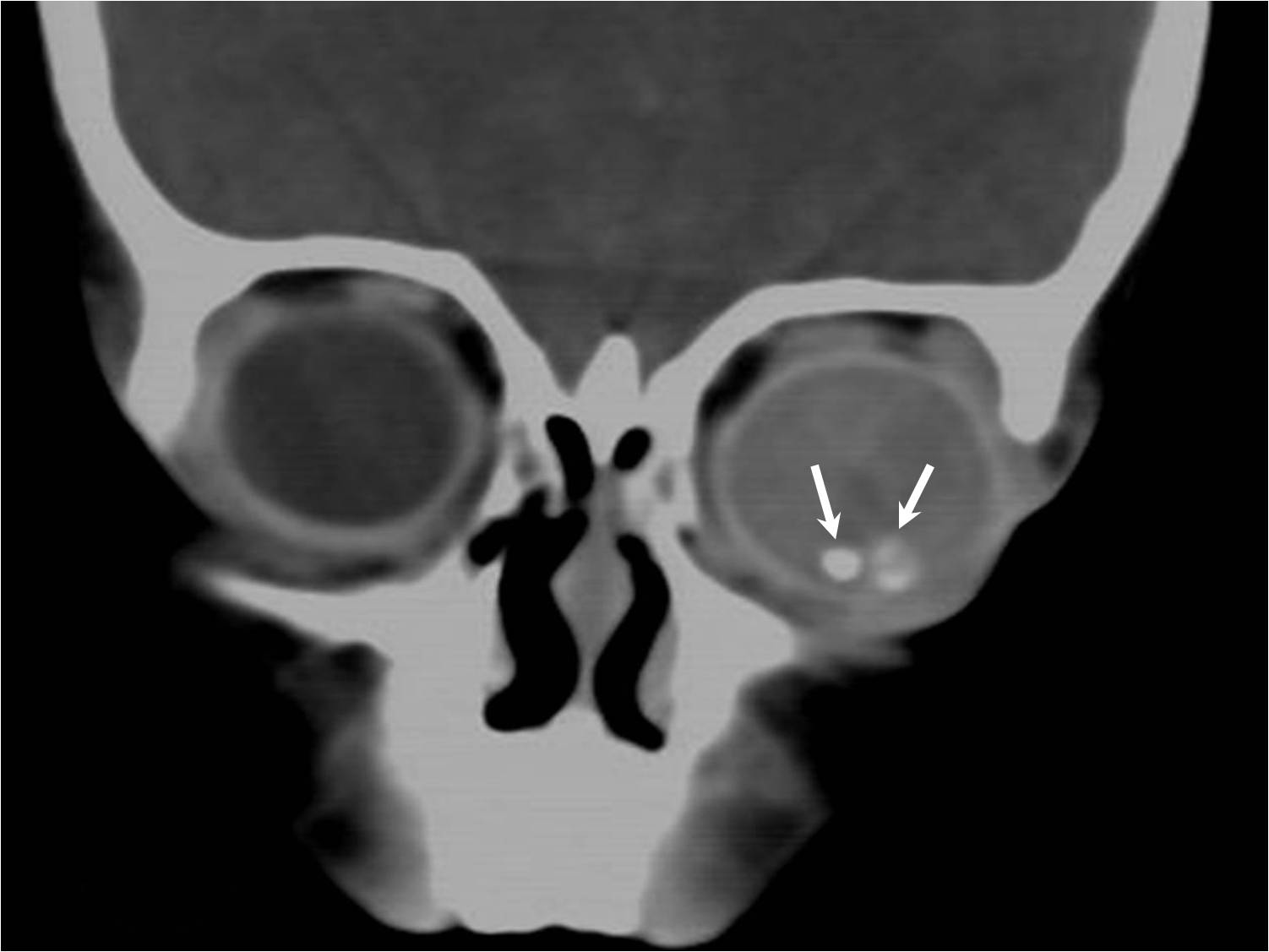
On CT [Table/Fig-7], retinoblastoma is characterised by enhancing intermediate-density soft-tissue mass or masses, with varying degrees of calcification. Retinoblastoma contracts, calcifies, and becomes hypo vascular in response to therapy [24]. Treatment includes enucleation for unilateral disease and radiation therapy with or without enucleation for bilateral disease.
Coronal CT scan image showing calcifications in Retinoblastoma
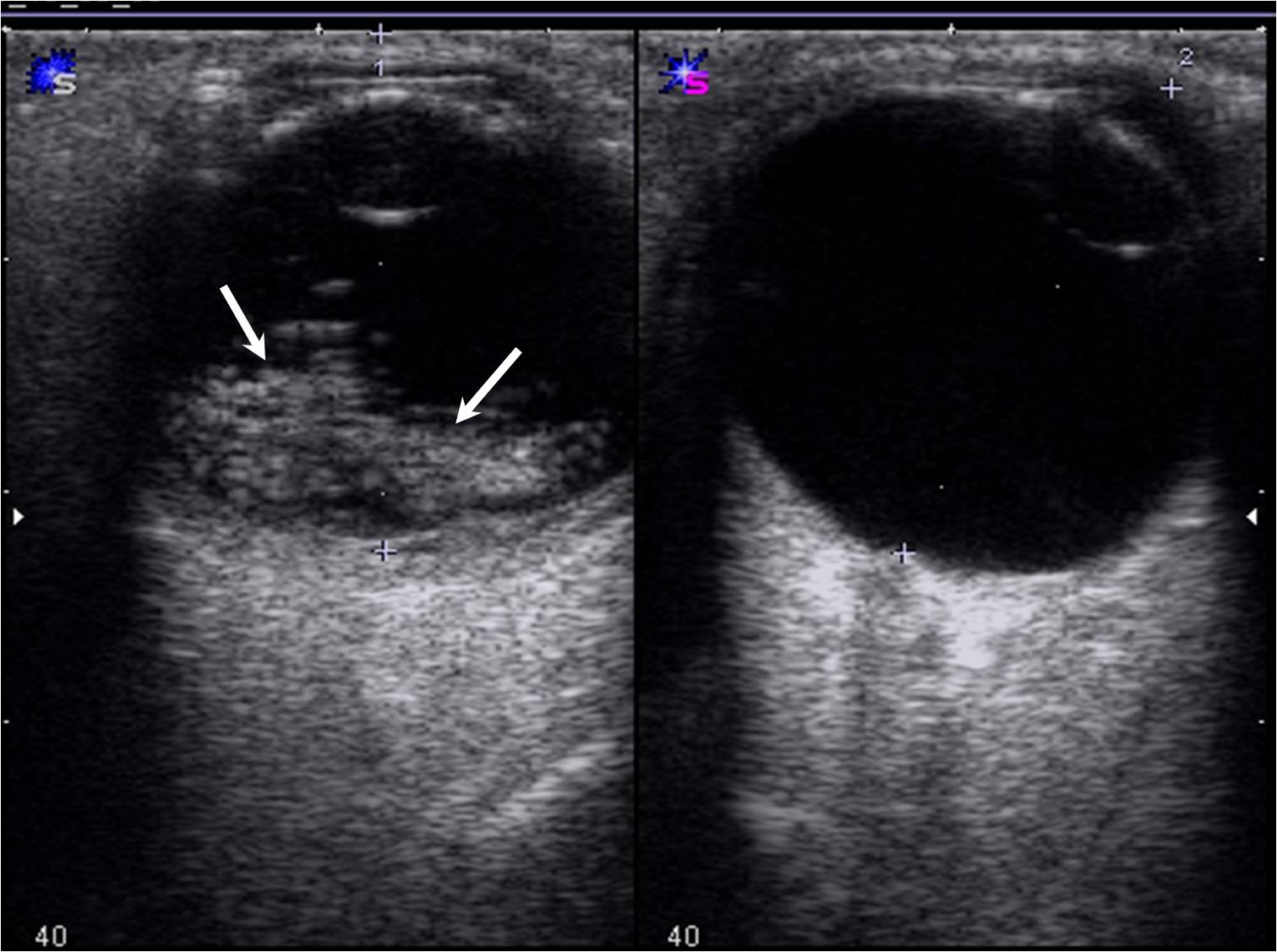
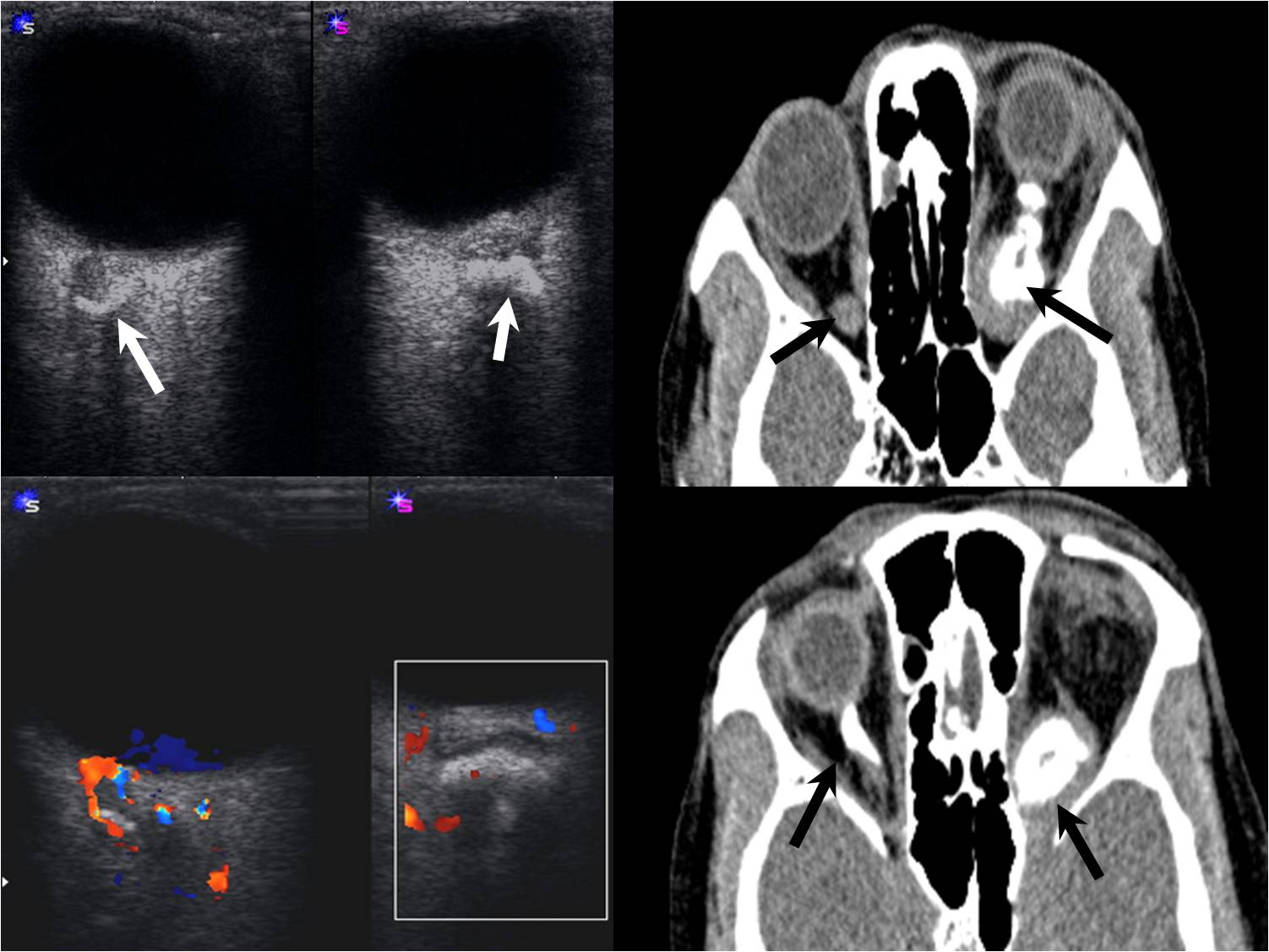
Other tumours of eye like optic nerve meningiomas are also demonstrated on USG [Table/Fig-8] as well as on CT scans [Table/Fig-8] due to their calcifications [25, 26].
USG and CT images showing calcifications in Optic Nerve Meningioma
Impact of Intra-Ocular Calcification on The Health of The Individual
Cataract affects the visual acuity and it can lead to progressive blindness in cases of Senile Cataracts and to developmental blindness in cases of Congenital Cataracts. Traumatic Cataracts can lead to instantaneous blindness. Hence, all types of cataracts are best treated to preserve optimum function of the eyes.
Although, AH does not impair vision; nevertheless, its association with diabetes must prompt one to keep an adequate follow up for earliest detection and timely management of dreaded diabetes. Calcifications seen in tumours need to be treated, not as separate entities, but as part of the tumour treatment only, depending on the tumour staging.
In conclusion, intraocular calcifications are quite distressing but they are diagnosable with the available array of imaging modalities. Though they can be detected by routine methods, one must also know about some newer methods of diagnosis, like Energy dispersive X-ray spectroscopy and optical coherence tomography (OCT), which can even diagnose the calcification of hydrogel Intra Ocular Lens as well [27, 28]. Moreover, it must also be remembered that advances in technology have made ultrasound and MRI as accurate as CT scan for detection of calcifications. In MRI, a high-resolution gradient-echo T2-weighted sequence showed promising results regarding detection of calcifications and it has been shown to be more effective than spin-echo techniques [29,30].
[1]. Thylefors B, Négrel AD, Pararajasegaram R, Dadzie KY, Global data on blindnessBull World Health Organ 1995 73:115-21. [Google Scholar]
[2]. Resnikoff S, Pararajasegaram R, Blindness prevention programmes: past, present and futureBull World Health Organ 2001 79:222-26. [Google Scholar]
[3]. Thylefors B, Resnikoff S, Progress in the control of world blindness and future perspectivesSanté 1998 8:140-43. [Google Scholar]
[4]. Marback R, Temporini E, Kara Júnior N, Emotional factors prior to cataract surgeryClinics 2007 62:433-38. [Google Scholar]
[5]. Walsh A, Métodos e técnicas de exame. In: Abreu G, editorUltra-sonografia ocular: atlas e texto 2002 3rd edRio de JaneiroCultura Médica:13-18. [Google Scholar]
[6]. Nassaralla Jr JJ, Nassaralla BA, The role of ecography before catarct surgeryRev Bras Oftalmol 2003 62:480-84. [Google Scholar]
[7]. Byrne SF, Green RL, Orbital Tumors. In: Byme SF, Green RL, editorsUltrasound of the Eye and Orbit 1992 St. LouisMosby Year Book:53-58. [Google Scholar]
[8]. Marcio Henrique Mendes, Alberto Jorge Betinjane, Adhele de Sá Cavalcante, Cheng Te Cheng, Newton Kara-José, Ultrasonographic findings in patients examined in cataract detection and treatment campaigns: A retrospective studyClinics 2009 64(7):637-40. [Google Scholar]
[9]. Rosen E, Patient workup for cataract surgery. In: Yanoff M, Duker JS, editorsOphthalmology 1999 LondonMosby International:181-84. [Google Scholar]
[10]. Anteby II, Blumenthal EZ, Zamir E, Waindin P, The role of preoperative ultrasonography for patients with dense cataract: a retrospective study of 509 casesOphthalmic Surg Laser 1998 29:114-18. [Google Scholar]
[11]. The Sankara Nethralaya Atlas of Ophthalmic Ultrasound 2006 First editionNew DelhiJaypee Brothers Medical Publishers (P) Ltd:56-57. [Google Scholar]
[12]. Allison KL, Price J, Odin LJ, Asteroid hyalosis and axial length measurement using automated biometryCataract Refract Surg 1991 17:181-86. [Google Scholar]
[13]. Byrne SF, Green RL, Ultrasound of the eye and orbit 2002 2 nd edSt. LouisMosby, Inc [Google Scholar]
[14]. Ultrasonography of the EYE and Orbit 2006 19106Second EditionPennsylvania, USALippincot Williams and Wilkins:76-77. [Google Scholar]
[15]. Jaffe N, The Vitreous in Clinical Ophthalmology 1969 St. LouisMosby [Google Scholar]
[16]. Cosgrove D, Meire H, Dewbury K, Clinical Ultrasound a comprehensive textAbdominal and General Ultrasound 2001 Vol. 2Second editionChurchill LivingstoneHarcourt Publishers Limited:673-74.Edinburgh: London W1P OLP [Google Scholar]
[17]. Sutton D, Fielding JA, Textbook of Radiology and Imaging 2008 Volume 2London W1T 4LPElsevier. Churchill Livingstone:1558-59. [Google Scholar]
[18]. McLeod D, Restori M, Rapid B-scanning in ophthalmology. In: Barnett E, Morley P, edsClinical Diagnostic Ultrasound 1985 OxfordBlackwell Scientific:111-120. [Google Scholar]
[19]. Coleman DJ, Lizzy FL, Jack RL, Ultrasonography of the eye and orbit 1977 PhiladelphiaLea and Febiger [Google Scholar]
[20]. McLeod D, Restori M, Ultrasonic examination in severe diabetic eye diseaseBr J Ophthalmol 1979 63:533-538. [Google Scholar]
[21]. Donaldson SS, Egbert PR, Lee W-H, Retinoblastoma. In: Pizzo PA, Poplack DG, edsPrinciples and Practice of Pediatric Oncology 1993 2nd edPhiladelphiaLippincott:683-96. [Google Scholar]
[22]. Kaufman LM, Mafee MF, Song CD, Retinoblastoma and simulating lesions: role of CT, MR imaging and use of Gd-DTPA contrast enhancementRadiol Clin North Am 1998 36:101--17. [Google Scholar]
[23]. Remit FG, Slovis TL, Baker JD, Orbital sonography in childrenPediatr Radiol 1996 26:245-58. [Google Scholar]
[24]. Abramson DH, McCormick B, Fass D, Retinoblastoma: the long-term appearance of irradiated ocular lesionsCancer 1991 67:2753-55. [Google Scholar]
[25]. Bhende Muna, Gopal Shriram, Gogi Anuj, Sharma Tarun, Gopal Lingam, Gopal Lekha, The Shankara Netralaya Atlas of Ophthalmic ultrasound (1st edition)Optic Nerve Disorders 9 :261-78. [Google Scholar]
[26]. Turbin Roger E, Pokorny Kathryn, Diagnosis and Treatment of Orbital Optic Nerve Sheath Meningioma University of Medicine and Dentistry of New JerseyNew Jersey Medical School Cancer Control 2004 11(5):334-41. [Google Scholar]
[27]. Macky TA, Werner L, Soliman MM, Pandey SK, Izak AM, Apple DJ, Opacification of two hydrophilic acrylic intraocular lenses 3 months after implantationOphthalmic Surg Laser Imaging 2003 34:197-202. [Google Scholar]
[28]. Hatou S, Inoue M, Kurosaka D, Hida YR, Shinoda K, Oguchi Y, Evaluation of calcification of a hydrogel intraocular lens by optical coherence tomographyJ Cataract Refract Surg 2004 30:1590-92. [Google Scholar]
[29]. Galluzzi P, Hadjistilianou T, Cerase A, Is CT still useful in the study protocol of retinoblastoma?AJNR Am J Neuroradiol 2009 30:1760-65. [Google Scholar]
[30]. Lemke AJ, Kazi I, Mergner U, Retinoblastoma – MR appearance using a surface coil in comparison with histopathological resultsEur Radiol 2007 17:49-60. [Google Scholar]