Immunodeficiency associated Burkitt’s lymphoma is the most common in patients with HIV/AIDS. It accounts for 30-40% of Non–Hodgkin’s lymphomas and may be the first sign of underlying immunosuppression. This report illustrates a case of Burkitt’s lymphoma of maxillary alveolar ridge, which was the first manifestation in an HIV positive patient, with a brief discussion on clinicopathologic features, aetiopathogenesis and treatment.
Case Report
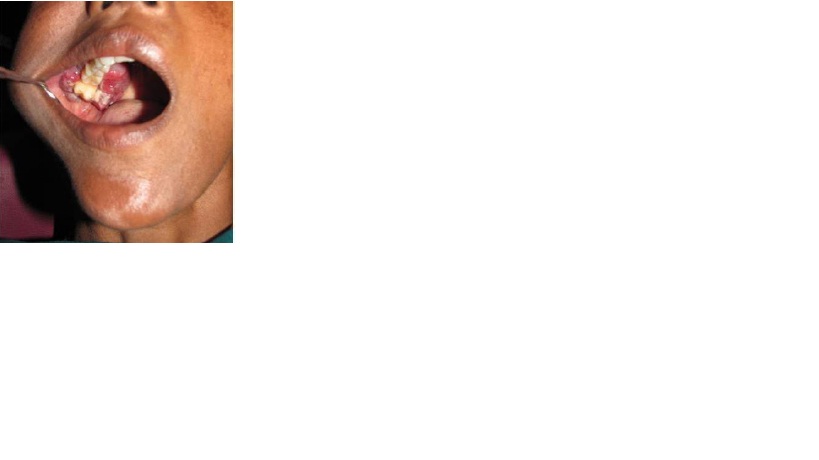
A 38–year–old female patient was reported to the Department of Oral Medicine and Radiology with a chief complaint of painless growth on the upper right back tooth region, which had been there since 6 months . Initially, it had started as small peanut sized lesion, which had gradually increased to the present size. Past medical and dental histories were non–contributory. On intra–oral examination, it was seen that there was a solitary, multinodular, erythematous growth of size 4 × 6cm, anteroposteriorly extending from 14-18 region and mediolaterally involving both the buccal vestibule and palate in 14-18 region [Table/Fig-1]. On palpation, the lesion was found to be firm in consistency, fixed to the underlying tissues, non–tender and bleeding. Mobility of the teeth was associated with the lesion.
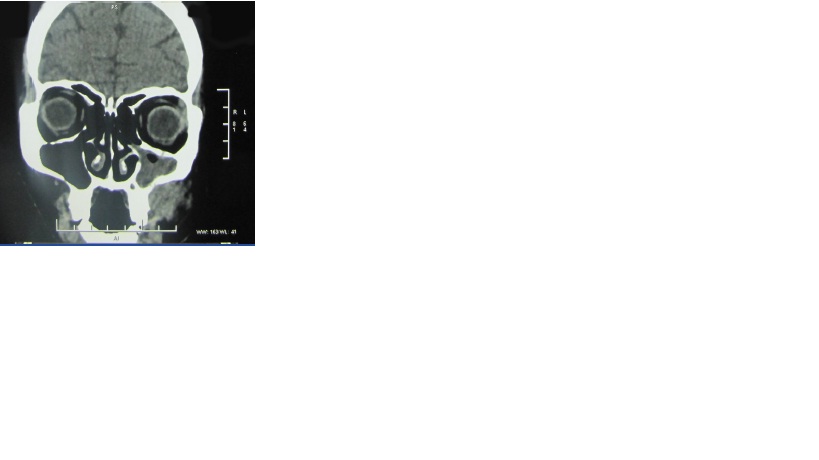
CT scan revealed a well defined irregular homogenous enhancing lesion in the maxilla, with the epicentre of the lesion in the posterior right alveolar groove (involving the last molar),causing destruction of the pterygoid plate and displacement of the last molar [Table/Fig-2].Patient was found to be reactive to HIV1 antibodies by Tridot test, which was further confirmed by Western blot. Based CD20on these clinical and radiologic findings, a provisional diagnosis of a malignant neoplasm arising from the maxillary alveolar ridge and a differential diagnosis of a nodular variant of squamous cell carcinoma, Burkitt’s lymphoma, fibrosarcoma, were given.
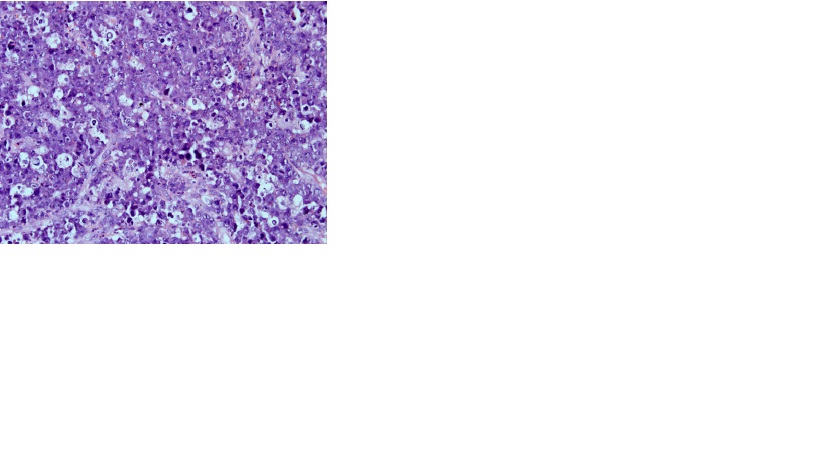
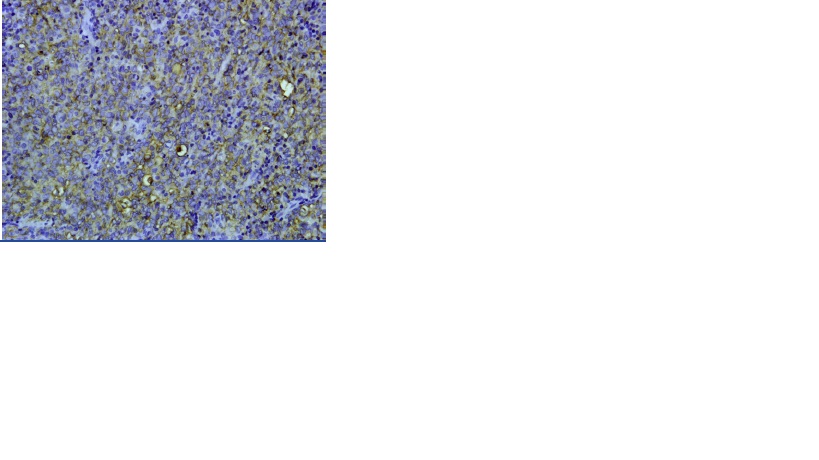
Incisional biopsy of the intra–oral mass was performed with special care and the tissue was sent for histopathologic examination. The tissue was routinely fixed, processed and stained with Haematoxylin and Eosin. On histopathological examination, it showed sheets of anaplastic round cells with an altered nuclear cytoplasmic ratio, nuclear hyperchromatism and abnormal mitotic figures in fibrovascular connective tissue stroma. Admixed among these, neoplastic lymphocytes and macrophages with clear cytoplasm were seen, which gave the appearance of starry- sky [Table/Fig-3]. The cytoplasm of these macrophages was laden with apoptotic bodies, which was suggestive of tingible body macrophages. Immunohistochemistry was performed with a panel of markers and the lesion exhibited positivity for CD20 (B cell marker, [Table/Fig-4]).
Based on the clinical, histological, radiological and immunohistochemical findings, a final diagnosis of Burkitt’s lymphoma was given and the patient was referred to a regional oncology centre for further treatment.
Intra-oral clinical aspect - an asymptomatic tumor-like mass on the right maxillary alveolar ridge
CT scan : coronal view showing mass in maxilla causing destruction of the pterygoid plate
Burkitt’s lymphoma- note pleomorphic lymphocytes and macrophages with a clear cytoplasm containing apoptotic cell bodies giving the appearence of Starry-sky
Immunohistochemistry positive with CD20on
Discussion
Burkitt’s Lymphoma (BL) is a highly aggressive form of Non–Hodgkin’s lymphoma which was first described in 1958 by Dennis Burkitt in Africa. He noticed a unique, rapidly growing jaw malignancy in children, especially in areas endemic for malaria, with greater rainfall and as well as in individuals with immunodeficiency [1]. The aetiology of BL was obscure and in 1964, Epstein Barr virus was identified in the cultured cell lines of this tumour. This was the first description of a virus which was involved in the pathogenesis of a tumour in the humans [2]. A further possible cause was chromosomal translocation that resulted in dysregulation of c-MYC oncogene [3].
The three clinical variants of Burkitt’s lymphoma, described by the World health organization, are endemic, sporadic and immunodeficiency associated types [4]. Endemic Burkitt’s lymphoma refers to those cases occurring in African children, involving bones of the jaws, kidneys, GIT, ovaries and breast. Sporadic Burkitt’s lymphoma occurs worldwide, with no specific geographic or climatic association. It accounts for 1–2% of lymphomas in adults and for 40% of lymphomas in children in U.S. with involvement of abdomen and ileocecal areas. Immunodeficiency associated Burkitt’s lymphoma mainly occurs in patients infected with HIV and in allograft recipients. It accounts for 30-40% of Non-Hodgkin’s lymphomas which occur in HIV positive patients [5].
Non–Hodgkin’s lymphomas of the B cell type are the second most common neoplasms which occur in HIV positive patients, the first type being Kaposis sarcoma [6]. 90% of the HIV associated Non–Hodgkin’s lymphomas are high grade, extra–nodal, small non– cleaved cell lymphomas of B cell origin and which involve oral cavity, digestive tract and CNS [7].
A majority of AIDS related oral Non-Hodgkin’s lymphomas are aggressive Burkitt’s lymphomas, large cell lymphomas or immunoblastic lymphomas that are associated with Epstein Barr virus [6]. Burkitt’s lymphoma was 1000 times more common in HIV positive individuals and often in AIDS defining criterion [8,9]. In our case also, the lesion was first manifestation. HIV patients with Burkitt’s lymphoma are usually younger as compared to patients with diffuse large B cell lymphomas and they have CD4 counts greater than 200 cells/μl. In our case also, the patient was younger and she had a CD4 count of about 450 cells/μl.
Usually, BL manifests as a soft tissue mass with or without ulceration, tissue necrosis and it occurs commonly on gingiva, palate and alveolar mucosa, with rapid growth and destruction [10–12]. Our case also, clinically and radiographically revealed a massively expansile lesion involving the maxilla. The earliest clinical sign of Burkitt’s lymphoma of jaws is mobility and exfoliation of the teeth, which are associated with the lesion [13]. We also observed similar features.
HIV infection causes polyclonal activation of B cells in an uncontrolled manner. The genetic instability of EBV positive, aberrantly regulated B cells leads to a risk of c-myc rearrangement and then, to lymphoma [14]. In 80% of the cases, there is presence of translocation between c-myc gene and the IgH gene t(8;14) and in 20% of cases, there is a translocation between c-myc and kappa or lambda light chain t(2;8) or t(8,22) [5]. C-myc rearrangement is a crucial event in lymphoma genesis.
Histologically, WHO has classified BL into three variants i.e., classical Burkitt’s lymphoma. Burkitt’s lymphoma with plasmacytoid differentiation and atypical Burkitt’s or Burkitt’s like lymphoma [4]. Classical Burkitt’s lymphoma is found in endemic and sporadic cases associated with children, whereas BL with plasmacytoid differentiation tends to occur in cases with immunodeficiency. But in our case, we found the histopathologic picture of classical Burkitt’s lymphoma. It is characterized by a mass of diffuse, neoplastic, non–cleaved B- lymphocytes admixed with histiocytes, giving the appearance of “starry-sky”.
Neoplastic lymphocytes were uniform, medium sized with round nuclei and multiple nucleoli. Numerous mitotic figures were seen. Admixed among the lymphocytes were numerous tangible body macrophages with apoptotic debris, giving a picture of “starrysky” [5].
Immunohistochemically, BL typically expresses surface IgM, pan B cell antigens including CD19, CD20, CD22 and CD 79a and it co-expresses CD10, Bcl-6, CD43 and p53, but not CD5, CD23, Bcl-2, CD 138 or TdT [15]. Our case showed positivity for CD 20, a B cell marker and it showed negativity for CD3.
Sporadic and immunodeficiency associated BL is less sensitive to chemotherapy as compared to endemic BL, indicating that its prognosis is poor. HAART (Highly active anti retroviral therapy) may improve the outcome, thus allowing the patients to tolerate full dose chemotherapy [16]. HIV patients require intensive treatment with transfusion and antibiotic therapy.
Conclusion
Thus, intra–oral Burkitt’s lymphoma may be one of the first manifestations in an HIV positive individual. Such patients should undergo investigations of the underlying condition and they should be treated with intensive chemotherapy with continuation of HAART.
[1]. DP Burkitt, Determining the climatic limitations of a chidren’s cancer common in AfricaBr.Med J 1962 2:1019-23. [Google Scholar]
[2]. R Khanna, SR Burrows, DJ Moss, Immune regulation in Epstein- Barr virus associated diseases.Microbiol Rev 1995 59:387-405. [Google Scholar]
[3]. SS Chuang, H Ye, MQ Du, CL Lu, A Dogan, PP Hsieh, Histopathology and immunohistochemistry in distinguishing Burkitt lymphoma from diffuse large B-cell lymphoma with very high proliferation index and with or without a starry-sky pattern: a comparative study with EBER and FISHAm J Clin Pathol 2007 128(4):558-64. [Google Scholar]
[4]. J Diebold, E Jaffe, M Raphael, R Warnke, lymphoma Burkitt, In: Jaffe E, Harris N, Stein H, Vardiman J, eds. Pathology and Genetics of Tumours of Hematopoietic and Lymphoid Tissues. Lyon, France: IARC PressJournal of the Canadian Dental Association 2001 :181-84. [Google Scholar]
[5]. JA Ferry, lymphoma Burkitts, clinicopathologic features and differential diagnosisThe Oncologist 2006 11:375-58. [Google Scholar]
[6]. JB Epstein, RJ Cabay, M Glick, Oral malignancies in HIV disease: changes in disease presentation, increased understanding of molecular pathogenesis, and current management. Oral Surgery, Oral Medicine, Oral Pathology,Oral Radiology and Endodontology 2005 100(5):571-77. [Google Scholar]
[7]. M Corti, MF Villafane, L Souto, R Schtirbu, M Narbait, MD Soler, Burkitt’s lymphoma of the duodenum in a patient with AIDS.Revista da Sociedade Brasileira de Medicina Tropical 2007 40(3):338-40. [Google Scholar]
[8]. YL Kasamon, LJ Swinnen, Treatment advances in adult Burkitt lymphoma and leukaemia.Curr Opin Oncol 2004 16:429-35. [Google Scholar]
[9]. V Ajila, R Gopakumar, S Hegde, GS Babu, Intra–oral Burkitt’s lymphoma in an HIV positive patient.Indian journal of sexually transmitted diseases and AIDS 2012 33(2):118-20. [Google Scholar]
[10]. HN Kamiru, S Naidoo, Oral HIV lesions and oral health behavior in HIV positive patients attending Queen Elizabeth Hospital, Maseru, Lesotho.SADJ 2002 57:479-82. [Google Scholar]
[11]. A Iamaroon, S Pongsiriwet, P Mahanupab, R Kitikamthon, J Pintong, Oral Non-Hodgkin lymphomas: studies of EBV and p53 expression.Oral Dis 2003 9(1):14-8. [Google Scholar]
[12]. K Ajita, S Rajeev, K Sweta, Oral Non-Hodgkin’s lymphoma in patient with HIV: a case report.Pravara Med Rev 2009 4(4):24-26. [Google Scholar]
[13]. K Patil, VG Mahima, BS Jayanth, L Ambika, Burkitt’s lymphoma in an Indian girl: a case report.J Indian Soc Pedod Prev Dent 2007 25:194-9. [Google Scholar]
[14]. DM Knowles, Etiology and pathogenesis of AIDS related Non-Hodgkin’s lymphoma.Haematol Oncol Clin North Am. 2003 17:785-820. [Google Scholar]
[15]. T Burmeister, S Schwartz, HA Horst, Molecular heterogeneity of sporadic adult Burkitt- type leukemia/lymphoma as revealed by PCR and cytogenetics: correlation with morphology, immunology and clinical featuresLeukaemia 2005 19:1392-98. [Google Scholar]
[16]. VL Kasamon, LJ Swinnen, Treatment advances in adult Burkitt lymphoma and leukaemia.Current Opin Oncol 2004 16:429-35. [Google Scholar]