Giant Cell Fibroma: A Case Report with Immunohistochemical Markers
Samson Jimson1, Sudha Jimson2
1Professor, Department of Oral & Maxillofacial Surgery,Tagore Dental College & Hospital,Rathinamangalam, Vandalur PO and Research Scholar, Bharath University, Chennai, Tamil Nadu, India..
2Reader, Department of Oral & Maxillofacial Pathology,Sree Balaji Dental College& Hospital,Rathinamangalam, Vandalur PO, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Samson Jimson,Professor, Department of Oral & Maxillofacial Surgery, Tagore Dental College & Hospital, Rathinamangalam, Vandalur PO, Chennai-600127, India.
Phone: 9940309211,
E-mail: jimsons@tagoredch.in
Giant cell fibroma may mimic fibroma of the gingiva, but have distinctive histopathological difference. Immunohistochemical markers are required to diagnose GCF. It may occur at any age but most often in the third decade of life. It may be often asymptomatic but may not be esthetic if present in the anterior region of the jaw. Surgical excision should be performed, and the prognosis is good. However long term follow-up is required to check for any recurrence. The most common gingival enlargements like fibroma and granuloma may be mistaken for GCF. We present a case report with histopathological markers used to diagnose GCF.
Giant cell, Fibroma, Gingiva, Vimentin
Introduction
Giant cell fibromas (GCFs) are a separate category under fibromas, that was first discovered by Weathers and Callihan in 1974. Eversole and Rovin compared 279 fibrous hyperplastic lesions that were categorized into four types, namely pyogenic granuloma, peripheral gingival fibroma, peripheral giant cell granuloma, and peripheral ossifying fibroma. All of them showed distinct characters in histopathological identification, but they were clinically found to be indistinguishable [1]. Giant cell fibroma was designated due to its stellate fibroblasts with multinucleated giant cells. Giant cell fibromas have equal sex distribution in first three decades of life [2]. They are most often seen in Caucasians [3]. Generally, fibrous hyperplasias are reactive lesions rather than neoplastic proliferations. GCFs were once thought to be viral induced, but this statement was not justified. Hence, they were believed to arise from a stimulus which was of unexplained origin [4]. Clinically, they may be sessile or pedunculated, affecting the gingival, with mandible being most common site than maxilla [5]. Histologically, such lesions exhibits spindle or stellate shaped fibroblasts with mono, bi or multinucleated fibroblasts with hyperplastic epithelium [6]. Here, we are reporting about a patient with a peripheral giant cell fibroma with clinical characteristics, histopathologic features under H and E and immune histochemical staining, along with literature review [7].
Case Report
A 25-year-old male patient reported to our centre with a gingival enlargement in the right mandibular, lateral incisor to second premolar region. Clinical history revealed that the patient had the growth since 5 years. It was asymptomatic, except for some discomfort which he felt during eating. Patient was a non-smoker and a nonalcoholic. His past medical history revealed a trauma which he had undergone 8 years back.
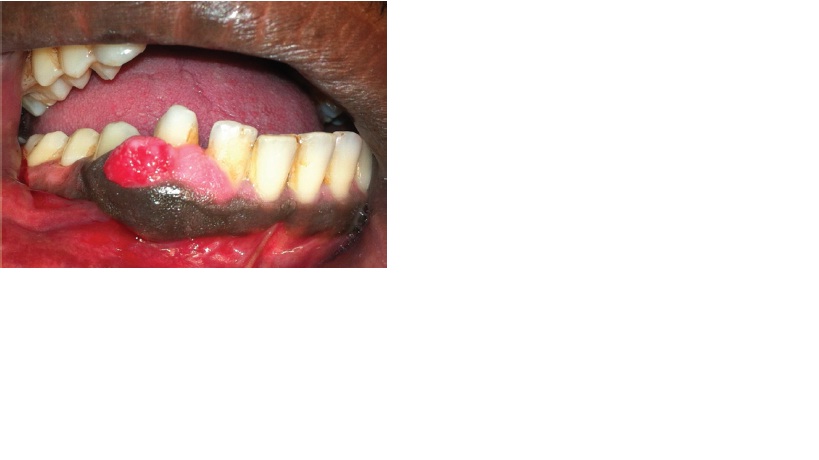
On extra oral examination, no obvious facial swelling was seen, neither were the submandibular or submental lymph nodes enlarged or palpable.Intraoral examination revealed a reddish gingival growth extending from 42 to 45 region [Table/Fig-1]. It was 1.5cm × 0.8 cms in size. On palpation, it was found to be sessile and it covered 3/4th of the crowns. Bleeding on probing was present in relation to the gingival enlargements. None of the teeth involved were carious. Mouth opening was normal and routine blood and radiographic examinations showed no abnormalities. A provisional diagnosis of gingival hyperplasia was given and a differential diagnosis of pyogenic granuloma was also considered.
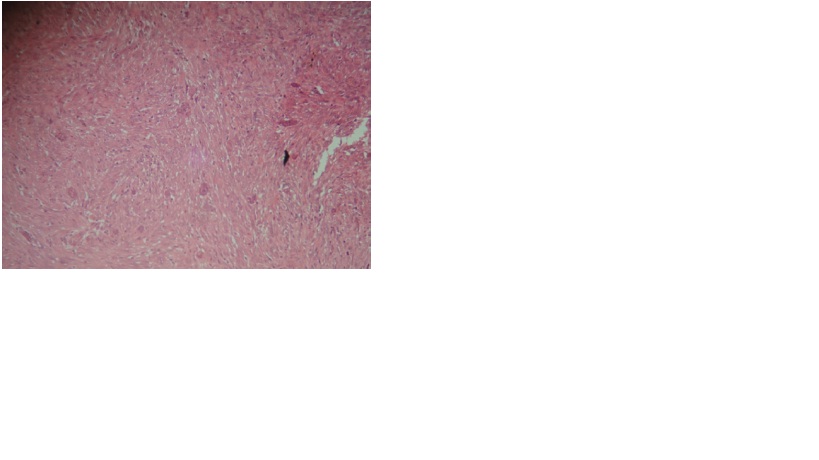
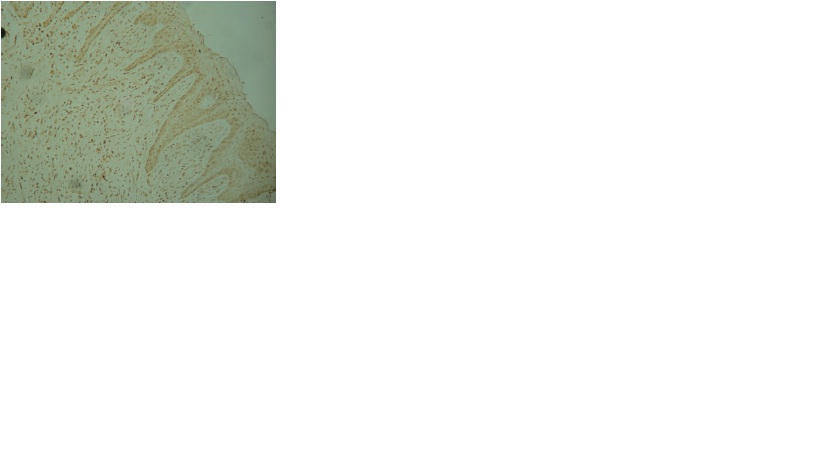
An excisional biopsy was performed under local anaesthesia and specimen sent for histopathological examination. The healing was PCNAnon eventful and patient did not report any complaints. Macroscopic details showed irregular, multiple soft tissue specimens that were brownish white in colour and firm in consistency. Microscopic findings showed hyperplastic epithelium with elongated rete ridges [Table/Fig-2]. The connective tissue stroma was fibrous, with plump stellate fibroblasts with multinucleated giant cells being scattered throughout [Table/Fig-3]. Inflammatory component was very minimal and a final diagnosis of a peripheral giant cell fibroma was made. Immunohistochemical staining was done, which showed positivity for vimentin and negativity for desmin [Table/Fig-4]. PCNA was also done for the proliferation, which showed intense staining [Table/Fig-5].
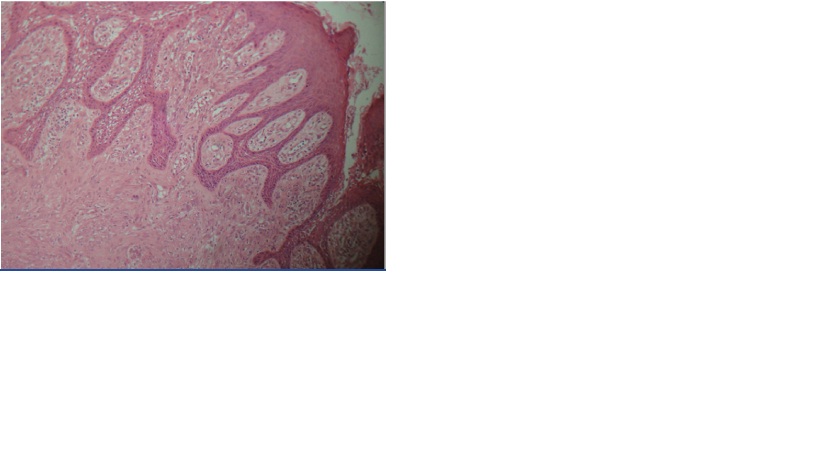
H&E under 40 X showing giant cells

Discussion
Giant cell fibroma is an entity which is separate from other fibrous lesions. Although the clinical behaviour and epidemiology of most of the non-neoplastic fibrous growths are similar, their histopathological features help in distinguishing them. Peripheral giant cell fibroma occurs in younger age group according to the literature, mandible being the most common site. It represents about 2-5% of all fibrous proliferations [8]. The aetiology of GCF, according to many reports, suggests that minor trauma can trigger development of the lesion and that it is characterized by functional changes in fibroblastic cells [9]. Clinically, it appears pebbly. GCF can be considered as differential diagnosis in fibrous hyperplastic lesions occurring in children. Regezi et al found that the presence of stellate cells was dependent on the pattern of collagen in the lamina propria and that stellate cells were most often found in oral lesions presenting on the gingival or palate, where the sub mucosa consisted mainly of lamina propria [10]. Weathers and Calihan revealed the structure under light microscope and concluded that the dominant cells in the GCF were unique and so GCF has its own standard of classification. The common sites are gingiva, tongue and the palate in the oral cavity. Apart from the oral cavity, the other site of occurrence is the nose, at which site the lesion differs histologically by the presence of larger stellate fibroblasts and a tendency to recur [11]. GCF differs from others fibromas in that the fibroblasts appear larger and stellate, but they not being hyper chromatic. GCF is similar to ossifying fibroma clinically, with same hue, but it can be differentiated histologically with the presence of islands of osteogenic cells in ossifying fibroma. Savage and Monsour [12] retrospectively reviewed the histologic features of all lesions designated as fibrous or fibro epithelial polyps over a 10-year period. They concluded that the histologic features were not sufficiently unusual or characteristic in normal or pathologic tissues, to warrant grouping of the lesions as a separate and distinct entity.
Ultrastuctural studies have shown that the multinucleated giant cells and stellate cells were unusual fibroblasts [13].
Immunohistochemical studies have revealed that giant fibroblasts showed negative reactivity for cytokeratin, neurofilament, HHF, CD68, HLA DR, tryptase, Leukocyte common antigen and S-100, and positivity for vimentin only, which was consistent with the findings of our case, suggesting a fibroblastic phenotype [14]. Desmin shows negative reactivity for giant cells, thus eliminating the possibility of a myofibroblastic origin, as was seen in our case.
Odell et al.,[15] suggested a fibroblastic origin of the giant cell, due to the vimentin positivity which was seen in his study. In our case, we found positivity for PCNA, with variable staining intensity and negativity for Ki-67. According to Mighell et al.,[14] heterogeneity in nuclear PCNA metabolism of GCF multinucleated cells is possible and the most intensely stained nuclei may have passed through the cell cycle more recently as compared to the less immuno reactive nuclei. However, the absence of Ki-67 immuno reactivity in GCF multinucleated cells, absence of mitoses in GCF multinucleated cells and absence of either PCNA or Ki-67 immuno reactivity in PGCG multinucleated cells, are consistent with an osteoclast lineage and their formations from differentiated mononuclear cells. Immuno staining with PCNA and Ki 67 revealed that PCNA showed a variable expression and that Ki 67 showed negativity, thus stating about the possibility of giant cells to be formed from mononuclear fibroblasts. The treatment of choice for GCF in adults and adolescents is surgical excision and it is electro surgery in children. Recurrence is very rare, but certain cases have been reported, which were controlled by local measures. Periodic follow ups are essential.
Conclusion
Enormous fibrous lesions are encountered in routine dental practice. Though they are rare lesions, they should be considered in the differential diagnosis of gingival enlargements. Extensive work up and thorough investigations are mandatory for making an accurate diagnosis and for proper treatment planning, for a better outcome.
[1]. DR Weathers, MD Callihan, Giant cell fibromaOral Surg Oral Med Oral Pathol. 1982 53:582-87. [Google Scholar]
[2]. I Varghese, A Prakash, Giant cell lesions of oral cavityOral and Maxillofacial Pathology Journal. 2011 2:107-10. [Google Scholar]
[3]. RJ Vergotine, A giant cell fibroma and focal fibrous hyperplasia in a young child: a case report.Case Rep Dent 2012 2012(370242)doi: 10.1155/2012/370242 [Google Scholar]
[4]. B Sekar, D Augustine, S Murali, Giant Cell Fibroma - A Case Report With Review Of Literature.Ind J of Dent Sciences 2011 5:48-50. [Google Scholar]
[5]. J Reibel, Oral fibrous hyperplasias containing stellate and multinucleated cells.Scand J Dent Res 1982 90:217-26. [Google Scholar]
[6]. P Soujanya, M Ravikanth, GN Kumar, Giant cell fibroma of maxillary gingival-A report of case and review of literature.SRM University Journal of Dental Science 2011 2:61-64. [Google Scholar]
[7]. MS Campos, C Domaneschi, FD Nunes, I Weinfeld, Giant cell fibroma of the maxillary gingiva in children: Case report.Journal of Dentistry for Children 2010 77:174-6. [Google Scholar]
[8]. M Shah, CV Rathod, V Shah, Peripheral giant cell fibroma:A rare type of gingival overgrowth.J Indian Soc Periodontol 2012 16:275-7. [Google Scholar]
[9]. B Sabarinath, M Sivaramakrishnan, B Sivapathasundharam, Giant cell fibroma: A clinicopathologicalstudyJ Oral Maxillofac Pathol 2012 16:359-62. [Google Scholar]
[10]. JA Regezi, RM Courtney, A Kerr, “Fibrous lesions of the skin and mucous membranes which contain stellate and Multinucleated cells,”Oral Surgery Oral Medicine and Oral Pathology 1975 39:605-614. [Google Scholar]
[11]. MM Braga, ALG Carvalho, MCP Vasconcelos, PH Braz-Silva, SL Pinheiro, Giant cell Fibroma: a case report.J Clin Pedia Dentistry 2006 30:261-64. [Google Scholar]
[12]. NW Savage, PS Monsour, Oral fibrous hyperplasias and the giant cell fibromaAust Dent J 1985 30(6):405-9. [Google Scholar]
[13]. AJ Mighell, PA Robinson, WJ Hume, PCNA and Ki-67 immunoreactivity in multinucleated cells of giant cell fibroma and peripheral giant cell granuloma.J Oral Pathol Med 1996 25:193-99. [Google Scholar]
[14]. J Reibel, Oral fibrous hyperplasias containing stellate and multinucleated cells.Scand J Dent Res 1982 90:217-26. [Google Scholar]
[15]. EW Odell, C Lock, TL Lombardi, Phenotypic characterisation of stellate and giant cells in giant cell fibroma by immunocytochemistryJournal of Oral Pathol Med 1994 23:284-87. [Google Scholar]