Aesthetic Rehabilitation of Discoloured Nonvital Anterior tooth with Carbamide Peroxide Bleaching: Case Series
Gautam P Badole11, Manjusha M Warhadpande2, Rakesh N Bahadure3, Shital G Badole4
1Senior Lecturer, Department of Conservative Dentistry & Endodontics,VSPM’s Dental College & Research Center, Nagpur, India.
2Associate Professor, Department of Conservative Dentistry & Endodontics,Government Dental College & Hospital, Nagpur, India.
3Senior Lecturer, Department of Pedodontics and Preventive Dentistry,Sharad Pawar Dental College, Sawangi, Wardha, India.
4BDSVSPM’s Dental College & Research Center,, Nagpur, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gautam P. Badole, Senior Lecturer, Department of Conservative Dentistry & Endodontics, VSPM’s Dental College & Research Center, Nagpur, Maharashtra– 440019, India.
Phone: 9665410655,
E-mail: badole_g15@yahoo.co.in
Discolouration of teeth, especially the anteriores, can result in considerably cosmetic impairment in person. Combine effects of intrinsic and extrinsic colour determines the appearance of teeth. Whitening of teeth with bleaching is a more conservative therapeutic method than full crowns, veneers or composite restorations which is more invasive and expensive. Among bleaching techniques, in office bleaching with carbamide peroxide provide superior aesthetic result in short period of time with no adverse effects. This paper presents case series of tooth discolouration in non-vital tooth which was successfully bleached using 35 % carbamide peroxide. After 1 year follow up the prognosis was good with no reversal of tooth discolouration. This case report allows the better understanding of the concept of nonvital tooth bleaching with carbamide peroxide which gives a non-invasive alternative for aesthetic purpose in preserving the natural tooth structure.
Bleaching, Carbamide peroxide, Discolouration, Non-vital tooth
Case 1
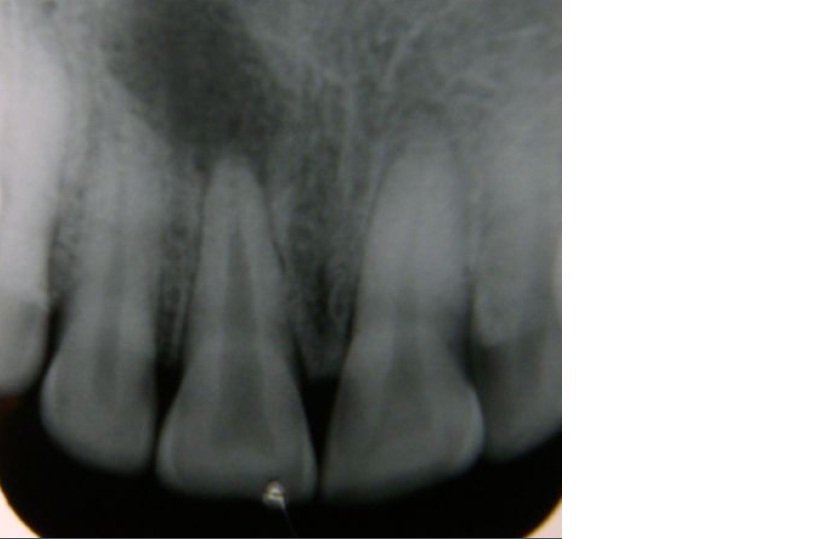
A 35 year old female patient was reported to the department of conservative dentistry and endodontics with complaint of discoloured upper anterior teeth. Patient had history of trauma with anterior teeth 5 years back. Intraoral examination revealed brown discoloured maxillary right central incisor [Table/Fig-1]. An intraoral radiograph showed large periapical lesion with 11 [Table/Fig-2]. Periapical cyst was diagnosed with 11. Non-surgical management with endodontic treatment and in office bleaching was planned. Access opening and complete biomechanical preparation was completed. Calcium hydroxide (RC Cal; Prime Dental Products, Thane, India.) intracanal medicament was placed and recalled the patient after three weeks. Obturation with lateral condensation was done and recalled after seven days for bleaching procedure. Gutta-percha filling was removed from the access cavity to 2 mm bellow cemento-enamel juction with gates glidden drill (Dentsply Maillefer, Ballaigues, Switzerland). A plug of resin modified glass ionomer (GC Fuji PLUS, GC Corporation, Tokiyo, Japan.) was placed over the gutta-percha in cervical region to prevent percolation of bleaching agent in apical area. Opalescence gel (Ultradent, St. Louis, MO, USA), containing 35% carbamide peroxide was used for bleaching. OpalDam was applied and cure for 20 second over gingiva as well as 2 mm over the adjacent the tooth for protection of gingiva. Opalescence gel was applied inside the pulp chamber as well as over labial surface and kept for 30 minutes [Table/Fig-3]. Material was removed from the tooth and thoroughly rinsed with water. The access cavity was sealed with IRM cement (Dentsply De Trey GmbH, Konstanz, Germany.) and patient was recalled after 72 hours for evaluation. Same procedure was performed in second visit as slight discolouration was present with 11. Two sittings of bleaching procedure showed complete removal of stains from the tooth and present colour was comparable to adjacent tooth [Table/Fig-4]. Coronal access cavity was sealed with composite resin (3M Dental Products, St Paul, MN, USA.). One year evaluation of patient showed complete healing of periapical lesion and no significant shade regression was observed [Table/Fig-5a,Table/Fig-5b].
Discoloured maxillary right central incisor

Periapical radiolucency with maxillary right central incisor
Opal Dam and Opalescence gel was placed over gingiva and tooth surface

Maxillary right central incisor after bleaching

No significant colour change was seen after one year

Healing of periapical lesion

Discoloured maxillary left central incisor

Significant colour change after bleaching

Discoloured maxillary right central incisor

Significant colour change after bleaching

Case 2
A 29–year–old female patient was reported to the department of conservative dentistry and endodontics with complaint of discoloured upper anterior teeth. Patient had history of trauma with anterior teeth 3 years back and she had taken root canal treatment for the same. Intraoral examination revealed brown discoloured maxillary left central incisor [Table/Fig-6]. An intraoral radiograph showed obturation and normal periapical tissue with 21. In office bleaching with 35 % carbamide peroxide (Opalescence gel, Ultradent, St. Louis, MO, USA) was decided for this patient and similar bleaching procedure was performed as described in above case. Tooth showed significant changes in shade after 72 hours [Table/Fig-7].
Case 3
Similar case of a 19–year–old male patient reported with complaint of discoloured tooth and history of trauma with maxillary right central incisor one year back. Patient had taken root canal treatment with the same tooth [Table/Fig-8a]. Single visit of 35 % carbamide peroxide(Opalescence gel, Ultradent, St. Louis, MO, USA) in office bleaching showed significant changes in shade of 11 [Table/Fig-8b]. There was no significant shade reversal observed in both the cases i.e. 2nd & 3rd, after three months of follow up period.
Discussion
Bleaching of discoloured nonvital teeth was first described during the middle of the 19th century advocating different chemical agents [1]. An early description of the use of hydrogen peroxide for bleaching was reported by Harlan [2]. Action of hydrogen peroxide is mainly due to reactive oxygen through the formation of free radicals [3]. Thermocatalytic technique was used to bleach nonvital teeth as the application of heat increases the bleaching properties of hydrogen peroxide by accelerating the bleaching reaction [1]. Today the thermocatalytic technique and high concentration of hydrogen peroxide is used less due to increase risk of external cervical resorption [4]. Exact mechanism of resorption in bleached tooth has not yet been adequately explained. There is speculation that hydrogen peroxide diffuses through dentinal tubules, cementum, periodontal ligament and reach to periradicular bone and directly induces an inflammatory resorption process [5]. There are different predisposing factor for diffusion of hydrogen peroxide to cervical tissue. Patients those had bleaching therapy at young age [6], application of heat (thermocatalytic method) [7] and natural anatomic defects at CEJ also responsible for diffusion of hydrogen peroxide into periradicular tissue [8]. Also the sealing of root filling with 2mm layer of glass ionomer cement at CEJ is essential to prevent radicular penetration of bleaching agents [9].
An alternative to thermocatalytic bleaching is the walking bleach technique with sodium perborate–hydrogen peroxide solution which did not show any cervical resorption even after 1 year [4]. More recently carbamide peroxide is the choice of material for intracoronal bleaching due to low levels of extraradicular diffusion and its effectiveness [10].
In present cases, 35 % carbamide peroxide was used as a bleaching material and placed on labial surface as well as in the pulp chamber because it is recommended that pulp chamber should accessible during bleaching procedure for proper penetration of material into discoloured tooth [1]. High concentration of bleaching agent promote faster tooth bleaching than lower concentrations of carbamide peroxide which takes longer time to bleach teeth but eventually achieve the same results as higher concentrations [11,12]. Carrasco et al., [13] reported that 37% carbamide peroxide as an intracoronal bleaching increased dentinal permeability, which was not observed for 27% carbamide peroxide.
35 % Carbamide peroxide when come in contact with water breaks into 23- 25% of urea and 10-12% of hydrogen peroxide [14]. Urea is capable of penetrating enamel and affecting the interprismatic region [15]. It is also capable of attacking the protein structure and denatures it. Structural alterations may occur in enamel proteins such as enamelin and amelogenin, thus urea increases the permeability of enamel to peroxides and free radicals [16]. Initial faster rate of bleaching was observed with higher concentration of carbamide peroxide [17]. The efficacy of hydrogen peroxide containing products are approximately the same when compared with carbamide peroxide containing products with equivalent or similar hydrogen peroxide content either tested in–vitro [18] or in –vivo [19]. Lim MY et al., in their study found that 35 % carbamide peroxide and 35 % hydrogen peroxide were equally effective for intracoronal bleaching [20].
The effect of carbamide peroxide on enamel surface after bleaching was studied by investigators and found there is no alteration of the surface texture of enamel or slight increase in enamel porosity immediately following treatment which is reversed after 6 months as observed in follow up examination [21,22]. Lewinstein et al., observed a slight reduction in enamel surface microhardness following 35% carbamide peroxide treatment on human enamel which was completely reversed when treated with 0.05% fluoride solution [23]. Carbamide peroxide was effective against mild to moderate fluorotic stains but more time is required to assimilate with the normal enamel in surrounding, due to different responses of sound and fluorotic enamel to the bleaching regimes [24]. Single bleaching therapy seems to be satisfying nonabrasive approach in cases of mild or moderate fluorosis[24].
Thus, non–vital tooth office bleaching with carbamide peroxide is a relatively fast method in whitening the discoloured tooth and equally effective to hydrogen peroxide with less complications of external cervical resorption.
Conclusion
From the present cases it was concluded that, 35% carbamide peroxide was effective as in office bleaching of discoloured nonvital teeth with significant improvement in colour of teeth in relatively short working time. Also the bleaching procedure is more economical and less invasive than other invasive tooth whitening procedures. This technique provides minimum risk of complications and more promising results.
[1]. RA Howell, Bleaching discoloured root-filled teethBr Dent J 1980 148:159-62. [Google Scholar]
[2]. AW Harlan, The removal of stains from teeth caused by administration of medical agents and the bleaching of pulpless toothAm J Dent Sci 1884/1885 18(521):355-61. [Google Scholar]
[3]. Z Gregus, CD (1995) Klaassen, Mechanisms of toxicity. In: Cassarett and Doull’s Toxicology, the basic science of poisons. Klaassen CDeditor New YorkMcGraw-Hill Companies Inc.:35-74. [Google Scholar]
[4]. S Madison, R Walton, Cervical root resorption following bleaching of endodontically treated teeth.J Endod 1990 16:570-74. [Google Scholar]
[5]. GS Heithersay, Invasive cervical resorption: analysis of potential predisposing factors.Quintessence Int 1999 30:83-95. [Google Scholar]
[6]. GS Heithersay, SW Dahlstrom, PD Marin, Incidence of invasive cervical resorption inbleached root-filled teethAust Dent J 1994 39:82-87. [Google Scholar]
[7]. I Rotstein, Y Torek, I Lewinstein, Effect of bleaching time and temperature on the radicular penetration of hydrogen peroxideEndod Dent Traumatol 1991 7:196-198. [Google Scholar]
[8]. AR Ten Cate, Oral histology: development, structure, and function 1985 2nd editionMosbySt Louis,MO [Google Scholar]
[9]. I Rotstein, D Zyskind, I Lewinstein, N Bamberger, Effect of different protective base materials on hydrogen peroxide leakage during intracoronal bleaching invitro. J Endod. 1992 18:114-47. [Google Scholar]
[10]. MY Lim, SO Lum, RS Poh, GP Lee, KC Lim, KC. An in vitro comparison of the bleaching efficacy of 35% carbamide peroxide with established intracoronal bleaching agentsInt Endod J 2004 37:483-88. [Google Scholar]
[11]. RH Leonard, A Sharma, VB Sharma, Use of different concentrations of carbamide peroxide for bleaching teeth: an in vitro study.Quintessence Int. 1998 29:503-37. [Google Scholar]
[12]. A Braun, S Jepsen, F Krause, Spectrophotometric and visual evaluation of vital tooth bleaching employing different carbamide peroxide concentrationsDent Mater. 2007 23:165-69. [Google Scholar]
[13]. LD Carrasco, IC Fröner, SA Corona, JD Pécora, Effect of internal bleaching agents on dentinal permeability of non-vital teeth: quantitative assessmentDent Traumatol 2003 19:85-89. [Google Scholar]
[14]. VB Haywood, HO Heymann, Nightguard vital bleachingQuintessence Int 1989 20:173-6. [Google Scholar]
[15]. J Aereuds, WL Jogenbloed, et al – Interaction of urea and human enamelCaries Research 1984 18:17-24. [Google Scholar]
[16]. M Goldberg, J Areuds, WL Jogenbloed, et al – Action of urea solution on human enamel surfacesCaries Research 1983 17:106-12. [Google Scholar]
[17]. BA Matis, Y Wang, T Jiang, GJ Eckert, Extended at-home bleaching of tetracyclinestained teeth with different concentrations of carbamide peroxideQuintessence Int 2002 33:645-55. [Google Scholar]
[18]. A Joiner, G Thakker, In vitro evaluation of a novel 6% hydrogen peroxide tooth whitening product.Journal of Dentistry 2004 32 (Suppl. 1):19-25. [Google Scholar]
[19]. PW Kihn, DM Barnes, E Romberg, K Peterson, A clinical evaluation of 10 percent vs 15 percent carbamide peroxide tooth-whitening agentsJ Am Dent Assoc 2000 131:1478-84. [Google Scholar]
[20]. MY Lim, SO Lum, RS Poh, GP Lee, KC Lim, An in vitro comparison of the bleaching efficacy of 35% carbamide peroxide with established intracoronal bleaching agents.Int Endod J 2004 Jul 37:483-88. [Google Scholar]
[21]. RH Leonard, JC Eagle, GE Garland, KP Matthews, AL Rudd, C Phillips, Nightguard vital bleaching and its effect on enamel surface morphologyJ Esthet Restor Dent 2001 13:132-39. [Google Scholar]
[22]. M Turkun, F Sevgican, Y Pehlivan, BO Aktener, Effects of 10% carbamide peroxide on the enamel surfacemorphology: a scanning electron microscopy studyJ Esthet Restor Dent. 2002 14:238-44. [Google Scholar]
[23]. I Lewinstein, N Fuhrer, N Churaru, H Cardash, Effect of different peroxide bleaching regimens and subsequent fluoridation on the hardness of human enamel and dentin.J Prosthet Dent. 2004 92:337-42. [Google Scholar]
[24]. M Knösel, R Attin, K Becker, A randomized CIE L *a*b* evaluation of external bleaching therapy effects on fluorotic enamel stains.Quintessence Int 2008 39:391-99. [Google Scholar]