The most accurate method which can be used for assessing Alveolar Bone Level (ABL) is to elevate the flap and measure the bone level directly and hence, it is considered to be the gold standard [1]. However, this method and other invasive clinical methods like transgingival probing/Bone Sounding (BS) [2–5] cause discomfort to the patients and they can damage the tissues. Therefore, many studies have been conducted to find an alternative method that can be used to assess the ABL both clinically and radiographically, with accuracy and reliability.
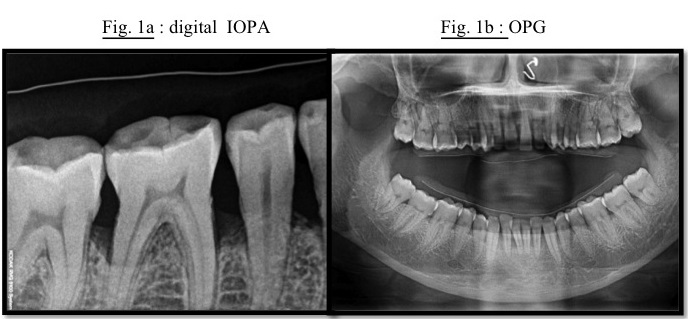
In routine dental practice, 10-14 IOPAs (Intra-oral periapical radiographs) and panoramic radiographs (OPG) are the most established imaging techniques [6,7]. However they tend to underestimate the bone loss and they also often tend to obscure defects, dehiscences, etc., especially when they are placed behind structures like roots, or when they are present on the lingual/palatal plates.
These shortcomings of all the 2D representations of the 3D alveolar bone, tooth and soft tissue, have been overcome with Dentascan [8–10], which provides 3D images that facilitate the transition of dental imaging from initial diagnosis to image guidance throughout the treatment phase.
A Dentascan examination is a specialized type of computed tomography study (CT or “CAT” scan) which is performed on a conventional CT scanner, which is used to obtain true cross-sections of the mandible and maxilla from the easily obtained CT scans of the patients. The dentascan formats standard axial CT scans into 3 planes: axial, (coronal) panoramic, and oblique sagittal (or cross-sectional) imaging [11,12].
As compared to Dentascan, the newer CBCT (Cone beam computed tomography) technology is much more cost-effective. CBCT also has reduced patient exposure to radiation as compared to Dentascan [13]. However, till date, the availability of novel CBCT in several Indian cities is a major hindrance, restricting its routine use in periodontics. Though Dentascan is expensive, recently, in-expensive X-ray tubes, decreased complexity, high quality flat panel detector systems and powerful personal computers have made this technique more affordable and practical, in routine dental practice and a natural fit in periodontal imaging. However, no study, to the best of our knowledge, has till date compared this novel technique with conventional radiographic and clinical techniques.
Hence, we carried out this study, the aim of which was to evaluate the reliability and accuracy of BS and radiographic bone measures and to compare them with Open Bone Measurements (OBM). The secondary objectives were to compare the clinical and radiographic measurements with OBM during surgery; to compare the measurements of ABL by various radiographic techniques like Dentascan, IOPA and OPG and to thereby obtain the most reliable and accurate radiographic technique; to compare the measurements of radiographic techniques with those of clinical BS; to evaluate lingual alveolar bone level by BS, dentascan and to compare them with OBM; and to compare the site-specific correlations between the various diagnostic techniques.
Material and Methods
Physically healthy patients with chronic periodontitis and those who were scheduled for open flap debridement were selected from the Department of Periodontics, KMSDCH. Prior to the commencement of the study, approval was obtained from institutional ethics committee and informed consents were obtained from the participants. Patients with a contra-indication for radiation exposure, eg: any significant, pre-existing lung disease, particularly where diffusing capacity was reduced, other conditions like pulmonary tuberculosis, cardiomyopathy, connective tissue disorders (SLE, scleroderma, etc) with significant vasculitis, individuals who were given a prior administration of radiation therapy to the same part, were excluded. Patients who were not willing to participate in the study and patients with presence of any underlying medical conditions, such as immunosuppression or diabetes; pregnancy; and medically compromised conditions that could put them at risk for periodontal surgery, were also excluded. The procedures which were followed in this study were in accordance with the ethical standards of the Sumandeep Vidyapeeth Ethical Committee and with the Helsinki Declaration of 1975 that was revised in 2000.
Initial therapy consisted of oral hygiene instructions, scaling and root planning. Following that, radiographs – Digital IOPA [Table/Fig-1a] and OPG [Table/Fig-1b], and dentascan [Table/Fig-2a, 2b, 2c] with customized pre-fabricated acrylic stents in-situ were taken.
(a): digital IOPA; (b): OPG # Distance between ligature wire & alveolar crest
(a): Dentascan - coronal view; (b) Dentascan – axial view
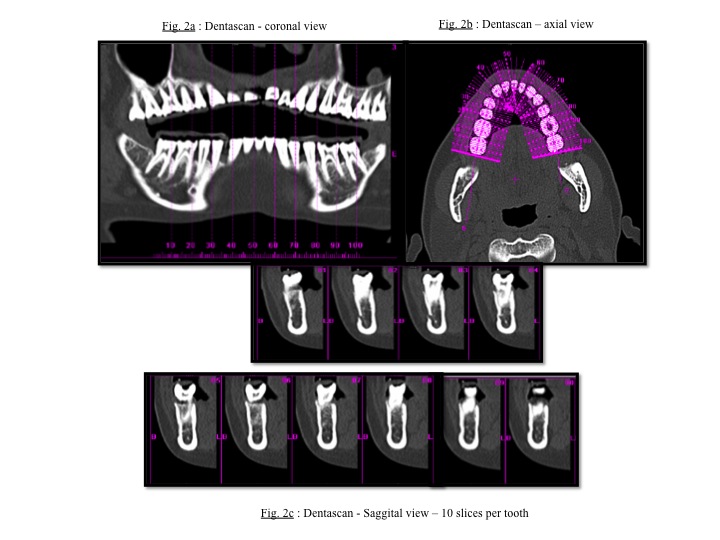
These customized acrylic stents with occluso-apical grooves had thin ligature wires ligated on their occlusal surfaces, which were placed bucally/labially. For IOPA and OPG, the distance between the thin ligature wire and the alveolar crest was measured by using the digital-Kodak imaging software, 6.8.6.0. For dentascan, the distance between the cross-section (white- radio -opaque dot on the dentascan [Table/Fig-2c]) of the thin ligature wire and the alveolar crest was measured with the help of the DICOM-CYNGO software. Once the measurements were taken, the stents were stored on the study casts, to minimize distortion.
Following this, on the 2nd visit, BS was performed after giving local anaesthesia and before the surgery [Table/Fig-3a]. The mesial and distal sites at the buccal and lingual aspects of the selected teeth were included in the recordings with the help of UNC15 probe, which was inserted and forced towards the bone and was made to contact it. Readings were then recorded with reference to the ligature wire of the customized stent by one investigator.
(a): Transgingival probing (BS) (b): Open bone measurement (OBM)
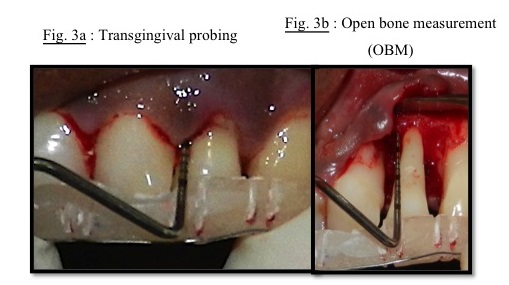
In the same visit, trained periodontal surgeons carried out the open flap surgical procedure. OBM was recorded with UNC15 probe after the placement of stent in the same position as that which was maintained during BS by the same periodontist [Table/Fig-3b]. Observers were blinded while they recorded all the parameters. Further surgical procedure was carried out and sutures were put and standard post-surgical protocol was followed.
Statistics
Required sample size was estimated using Open Epi software. (α=0.05, power=0.8, largest difference to be detected = 0.5, SD=1.0, no.of groups=5, sample size per group=41). Statistical analysis of the collected data was done using Student’s paired t-test and ANOVA test to identify the significance in the differences between the different diagnostic groups. The correlation between various techniques was evaluated using Pearson’s correlation co-efficient.
Results
A total of 205 sites were selected. Only OBM and BS showed agreement amongst them, as there was no statistically significant difference between them. (p>=0.05, for both buccal as well as lingual sites.) A statistically significant difference was seen between OBM and all the radiographic techniques (p< 0.05) and also there was no agreement amongst the 3 radiographic techniques (p< 0.05) [Table/Fig-4].
Comparing the buccal and lingual measurements for various techniques.
| Technique | n | Mean (mm) | Std. Deviation (mm) | p |
|---|
| Comparing OBM and BS |
| Buccal | OBM | 149 | 15.72 | 2.73 | 0.48 |
| BS | 151 | 15.94 | 2.71 |
| Lingual | OBM | 148 | 16.22 | 2.85 | 0.48 |
| BS | 152 | 15.99 | 2.95 |
| Comparing OBM and dentascan |
| Buccal | OBM | 149 | 15.72 | 2.73 | < 0.001 |
| Dentascan | 147 | 13.46 | 2.23 |
| Lingual | OBM | 148 | 16.22 | 2.85 | < 0.001 |
| Dentascan | 147 | 13.11 | 2.52 |
| Comparing OBM and OPG |
| Buccal | OBM | 149 | 15.72 | 2.73 | < 0.001 |
| OPG | 154 | 11.48 | 2.20 |
| Comparing OBM and IOPA |
| Buccal | OBM | 149 | 15.72 | 2.73 | < 0.001 |
| IOPA | 154 | 14.68 | 2.42 |
| Comparing Dentascan and IOPA |
| Buccal | Dentascan | 147 | 13.46 | 2.23 | < 0.001 |
| IOPA | 154 | 14.68 | 2.42 |
| Comparing Dentascan and OPG |
| Buccal | Dentascan | 147 | 13.46 | 2.23 | < 0.001 |
| OPG | 154 | 11.48 | 2.20 |
n = sample size, OBM = Open bone measurement, BS = Transgingival probing, IOPA = intra-oral periapical radiographs, OPG = orthopantogram, p = p-value
Though significant comparisons weren’t obtained for most of the techniques, however, we could establish significant correlations between many comparisons using the Pearson’s correlation co-efficient test. The greatest correlation was established for disto-lingual and disto-buccal sites of BS and OBM, and for disto-buccal sites of IOPA and OBM, and IOPA and BS. This was followed by a decent agreement for mesio-buccal sites, between dentascan and OBM measures, followed by mesio-lingual measures between dentascan & BS. For mesio-lingual sites, BS also showed correlation with OBM lingually, and with IOPA buccally [Table/Fig-5 and 6].
Pearson correlation co-efficient for buccal sites
| Correlating disto-buccal sites for all the techniques |
|---|
| | OBM_Buccal | BS_Buccal | D_Buccal | OPG_Buccal | IOPA_Buccal |
|---|
| OBM_Buccal | Pearson Correlation | 1 | .443* | -.155 | .054 | .745** |
| P | | .04 | .52 | .82 | < 0.001 |
| N | 21 | 21 | 20 | 21 | 21 |
| BS_Buccal | Pearson Correlation | .443* | 1 | -.106 | .419 | .654** |
| P | .04 | | .66 | .06 | .001 |
| N | 21 | 21 | 20 | 21 | 21 |
| D_Buccal | Pearson Correlation | -.155 | -.106 | 1 | .083 | -.156 |
| P | .52 | .65 | | .72 | .50 |
| N | 20 | 20 | 21 | 21 | 21 |
| OPG_Buccal | Pearson Correlation | .054 | .419 | .083 | 1 | .234 |
| P | .82 | .06 | .72 | | .30 |
| N | 21 | 21 | 21 | 22 | 22 |
| IOPA_Buccal | Pearson Correlation | .745** | .654** | -.156 | .234 | 1 |
| P | < 0.001 | .001 | .50 | .30 | |
| N | 21 | 21 | 21 | 22 | 22 |
| Correlating mesio-buccal sites for all the techniques |
| | OBM_Buccal | BS_Buccal | D_Buccal | OPG_Buccal | IOPA_Buccal |
| OBM_Buccal | Pearson Correlation | 1 | .204 | .544* | .032 | .384 |
| P | | .38 | .02 | .90 | .09 |
| N | 21 | 21 | 19 | 21 | 21 |
| BS_Buccal | Pearson Correlation | .204 | 1 | .120 | .098 | .449* |
| P | .38 | | .63 | .66 | .04 |
| N | 21 | 22 | 19 | 22 | 22 |
| D_Buccal | Pearson Correlation | .544* | .120 | 1 | .131 | .184 |
| P | .02 | .63 | | .60 | .45 |
| N | 19 | 19 | 19 | 19 | 19 |
| OPG_Buccal | Pearson Correlation | .032 | .098 | .131 | 1 | .020 |
| P | .89 | .66 | .60 | | .93 |
| N | 21 | 22 | 19 | 22 | 22 |
| IOPA_Buccal | Pearson Correlation | .384 | .449* | .184 | .020 | 1 |
| P | .09 | .04 | .45 | .93 | |
| N | 21 | 22 | 19 | 22 | 22 |
* indicates significance at the 0.05 level
** indicates significance at the 0.01 level
Pearson correlation co-efficient for lingual sites
| Correlating disto-lingual sites for all the techniques |
|---|
| | OBM_Lingual | BS_Lingual | D_Lingual |
|---|
| OBM_Lingual | Pearson Correlation | 1 | .582** | .343 |
| P | | .01 | .14 |
| N | 20 | 20 | 20 |
| BS_Lingual | Pearson Correlation | .582** | 1 | .386 |
| P | .01 | | .08 |
| N | 20 | 22 | 21 |
| D_Lingual | Pearson Correlation | .343 | .386 | 1 |
| P | .14 | .08 | |
| N | 20 | 21 | 21 |
| Correlating mesio-lingual sites for all the techniques |
| | OBM_Lingual | BS_Lingual | D_Lingual |
| OBM_Lingual | Pearson Correlation | 1 | .529* | .394 |
| P | | .01 | .10 |
| N | 21 | 21 | 19 |
| BS_Lingual | Pearson Correlation | .529* | 1 | .477* |
| P | .01 | | .04 |
| N | 21 | 22 | 19 |
| D_Lingual | Pearson Correlation | .394 | .477* | 1 |
| P | .10 | .04 | |
| N | 19 | 19 | 19 |
** indicates significance at the 0.01 level
* indicates significance at the 0.05 level
Discussion
The results of this study showed that only BS could be compared with the gold standard-OBM. This was in agreement with the study which was done by Yun JH et al., [14], in which he evaluated the BS and radiographic measurements for 24 infrabony defects, and compared them with OBM, and concluded that, BS is a reliable method for the assessment of the actual bone level, following any type of periodontal regenerative therapy. Similar results were obtained from 38 first molars by Hyung-Young et al., [5], where, they concluded that the BS measurement was a reliable method for the assessment of the actual bone level, following any type of periodontal regenerative therapy. Ursell et al., [2], also showed the same results. Akesson et al., [1], did a study which considered 237 sites, compared marginal bone levels for the techniques like Panoramic, bitewing, periapical and bone probing. They concluded that probing bone level before surgery was the most accurate one, deviating at most 5% from the true value, followed by periapical radiography, which was more accurate than panoramic and bitewing radiography (p < 0.001). Though our study showed similar result with the BS, however, similar results with the radiographic techniques couldn’t be obtained.
Our present study failed to show any positive comparison between radiographic measurements and the gold standard-OBM. One of the reasons for such a result, might be the fact that we opted for digital periapical radiography instead of conventional radiographs. In this study, Kodak imaging software, 6.8.6.0 was used to analyze the amount of ABL. Daniel M et al., showed that digital radiography was less diagnostically accurate as compared to conventional radiography. Moreover, digital enhancement may provide information that is diagnostically misleading. Also, in, Renvert et al., [4] showed that the radiographic bone height had a lower degree of correlation with the bone height which was measured during surgery, than the results of probing before surgery. Another reason for having no agreement with clinical techniques might be the fact that till date, there isn’t any specific method to standardize digital radiographic technique. Our study also failed to show any association between IOPA and OPG. This result was in agreement with the results of study done by Ti-Sun Kim et al., Their justification for this was that the population that they selected in their study, which comprised of chronic and aggressive periodontitis patients. This population was quite similar to our study population of chronic periodontitis patients, who were otherwise scheduled for surgery. Disagreement between OPG and IOPA tends to increase with an increase in the amount of bone loss, which was apparent in our chronic periodontitis patients. Most of the recent dentascan studies focus on its implication in implant dentistry. Unlike our study, direct comparisons amongst several radiographic techniques hadn’t been made. Lingeshwar D et al., [15], stated that CT scan was one of the upcoming diagnostic modalities in dentistry. HP. Bhatia et al., [16], in his review article written on Dentascan, also stated that unlike previous imaging techniques, the oblique sagittal view of Dentascan permitted the evaluation of distinct buccal and lingual cortical bone margins, as well as clear visualization of internal structures, such as the incisive and inferior alveolar canals. In contrast to these articles, our clinical study failed to show any superiority of Dentascan over digital IOPA, as well as any correlation with the clinical measurements. One of the reasons for no agreement with other radiographic or clinical measurements is the rounding off, of the measured values in all the techniques. BS and OBM gave values in mm (e.g.: 9 mm). However, the radiographic techniques like OPG gave values in 10th of the decimal (e.g.: 9.1). The digital IOPA gave a value in 100th of the decimal (e.g.: 9.15). Dentascan gave values in 1000th of the decimal (e.g.: 9.157). Thus, the maximum amount of rounding had to be done in case of the dentascan measurements. This gave rise to measurement discrepancies.
Though significant comparisons weren’t obtained for most of the techniques, however, we could establish significant correlations between many comparisons by using the Pearson’s correlation co-efficient test. The greatest correlation was established for distal sites between BS and OBM for lingual measurements, and for IOPA and OBM, and IOPA and BS for buccal measurements. This was followed by a decent amount of agreement for mesial sites, between dentascan and OBM for buccal measures, and between dentascan and BS for lingual measures. BS also showed correlation with OBM for lingual sites, and with IOPA for buccal sites. Overall, the correlation which was obtained was more for distal sites as compared to that which was obtained for mesial sites. These results are also in accordance with those of Ti-Sun Kim et al.,’s study which was done. They obtained more correlation for distal sites between IOPA and OPG as compared to that for the mesial sites. The reason for this again might be attributed to greater amount of bone loss on the mesial aspect, as compared to that on the distal sites.
Another drawback of this study, which may have contributed to its results, is the fact that though initially, 205 sites were selected for measuring the ABL, many of the sites couldn’t be measured due to various reasons. In OBM, only 149 sites were measured due to the fact that, since the surgeries were done quadrant wise, adjacent sites of the operated area weren’t accessed, while the neighbouring quadrant was operated. Many sites resolved after the initial phase I therapy. Similarly, for the same reason, at many sites, BS wasn’t performed (151 sites). Only 147 sites were assessed with Dentascan. Here, the main problem was the 1mm section, which was set for slicing. At many sites, the ligature wire, which was seen as a radio-opaque dot in the sagittal sections, escaped the mesial and distal slices for that tooth, i.e. the slices weren’t precise enough to show our thin reference point, which was used for measuring the ABL. Other reasons like magnification, shortening, etc. limited the OPG and IOPA sites to 154 each.
Apart form these limitations, other drawbacks of the dentascan technique itself, contributed to the overall limitations of the study. Patients were exposed to radiation every time the radioagraphic assessment was to be done (for all the 3 radiographic techniques-IOPA, OPG and Dentascan.) However, this overall radiation exposure was much less than the fatal dose of 20,000 mSV, which could lead to a cancerous risk. Also the dental tissues aren’t as susceptible to radiation damage as compared to other rapidly dividing tissues in the body [13]. Hence, the harmful effects of radiation exposure in our study could be considered to be negligible. Other few drawbacks associated with dentascan are, its cost, clarity, interpretation, limited availability of reconstructive software and chances of metallic streak artifacts, which need to be taken care of. Apart from them, special ’Digital Imaging and Communications in Medicine’ (DICOM) software is required in the computers to decode the scans. DICOM is a standard software for handling, storing, printing, and transmitting information in medical imaging.
One of the few positive points of this study is the fact that a very thin ligature wire was used as a reference point for assessing the alveolar bone level. Patients were asked to put the same stent in situ for all the techniques, prior to the recordings. Vertical grooves were made both bucally as well as lingually, on mesial and distal aspect of each tooth, for guiding the UNC15 probe each time. For dentascan, the thinnest possible slice which was available (1mm) was selected for evaluation, for greater accuracy. The sample size which was selected was quite satisfying as compared to those in other studies of similar kind, which have been mentioned earlier in the discussion. Also, there were two observers taking the measurements. One took the OBM, which is the gold standard, and the other took all other measurements of BS, OPG, IOPA and dentascan. Thus, the observers were blinded, as the other observer was unaware of the recordings of the gold standard technique.
To sum up, we can propose that the novel technique of Dentascan, fails to show any association with the surgically confirmed bone levels. Dentascan assessed measurements can’t be compared with those assessed by the conventional radiographic techniques of digital IOPA and OPG. Also, the other conventional radiographic measurements can’t be compared with the gold standard - OBM. So, we couldn’t establish any single best radiographic technique for alveolar bone assessment. Radiographic measurements also failed to show any agreement with BS.
Only BS showed agreement with OBM, for both buccal as well as lingual sites.
Inspite of failure of an agreement between the various techniques, good amount of correlation was obtained for distal sites, between the OBM and BS (lingual sites). IOPA also showed correlation with OBM and BS for buccal measurements. Dentascan measures correlated with OBM and BS for lingual sites. Overall, correlation between various diagnostic techniques for distal sites was greater than that for the mesial sites.
Conclusion
Thus, within the limitations of this study, it can be concluded that though Dentascan is a novel technique in field of Periodontics, which has successfully been proven time and again by various in-vitro studies, still, further, clinical studies are required to prove its reliability and accuracy, before it can be used rationally & routinely in periodontal practice.
n = sample size, OBM = Open bone measurement, BS = Transgingival probing, IOPA = intra-oral periapical radiographs, OPG = orthopantogram, p = p-value
* indicates significance at the 0.05 level
** indicates significance at the 0.01 level
** indicates significance at the 0.01 level
* indicates significance at the 0.05 level