Giant Subcutaneous Synovial Sarcoma: An Interesting Case
Pankaj Kumar Garg1, Debajyoti Mohnaty2, Bhupendra Kumar Jain3, Sunny Goel4, Bharat Singh5
1 Assistant Professor, Department of Surgery, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, Delhi, India.
2 Assistant Professor, Department of Surgery, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, Delhi, India.
3 Director Professor and Head, Department of Surgery, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, Delhi, India.
4 Post Graduate Resident, Department of Surgery, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, Delhi, India.
5 SAG Pathologist, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pankaj Kumar Garg, Assistant Professor, Department of Surgery, University College of Medical Sciences and Guru Teg Bahadur Hospital, Dilshad Garden, Delhi-110095, India.
Phone: +91 9999817562,
E-mail: dr.pankajgarg@gmail.com
A 45-year-old lady presented to us with a large subcutaneous swelling on her left side of back of 1 year duration. Local examination revealed a 13×12 cm spherical swelling on the left lower paraspinal region. Magnetic resonance imaging of lumbosacral spine revealed a 13×12 cm mass having solid and cystic components with internal septations in the subcutaneous tissue of left posterior paraspinal area. The mass was hetrogenously hyperintense on T 2 weighted images suggestive of synovial sarcoma. Wide local excision of the lump was carried out followed by closure of the defect with a lateral intercostal artery based rotational flap. The histopathology of the excised tumor revealed synovial sarcoma that stained positive for cytokeratin and epithelial membrane antigen. This case highlights an unusually large subcutaneous synovial sarcoma present in para-spinal area.
Synovial sarcoma, Soft tissue tumor, Cytokerati, Malignant neoplasm
Case Report
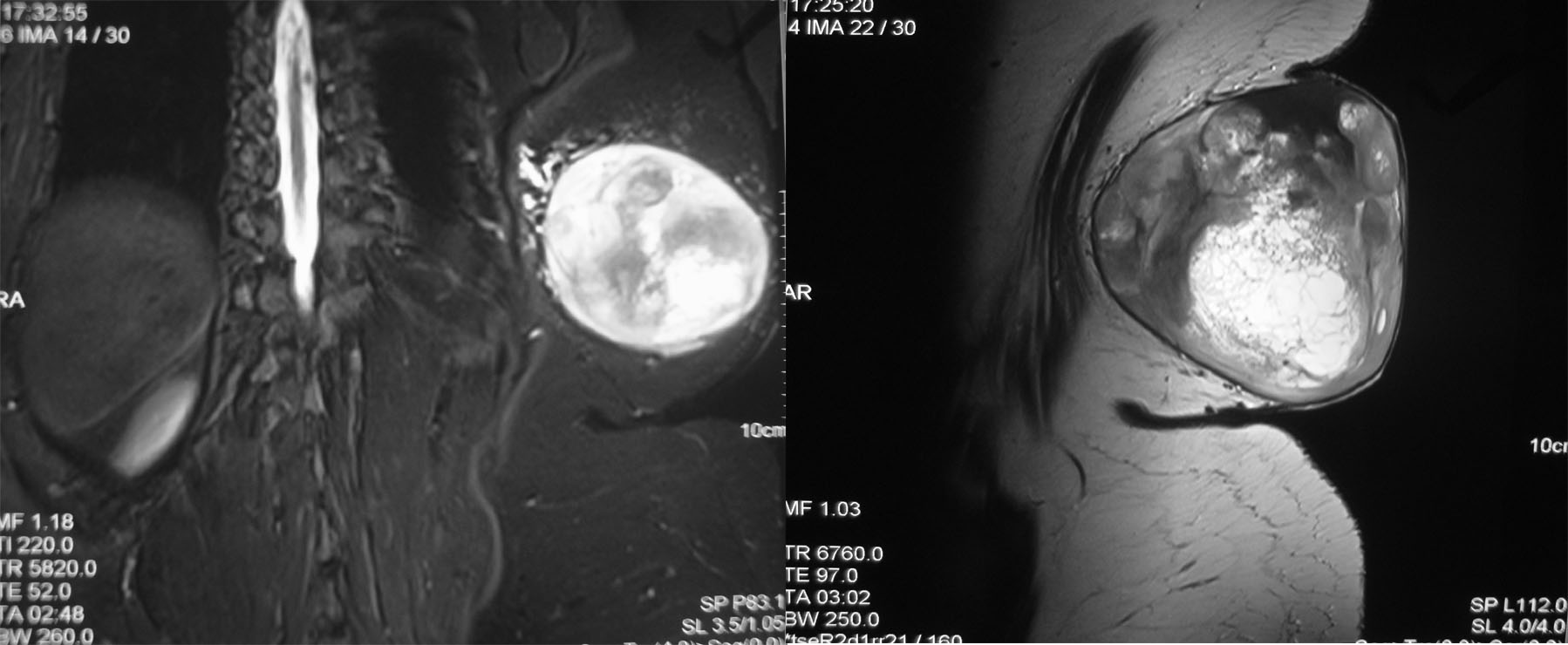
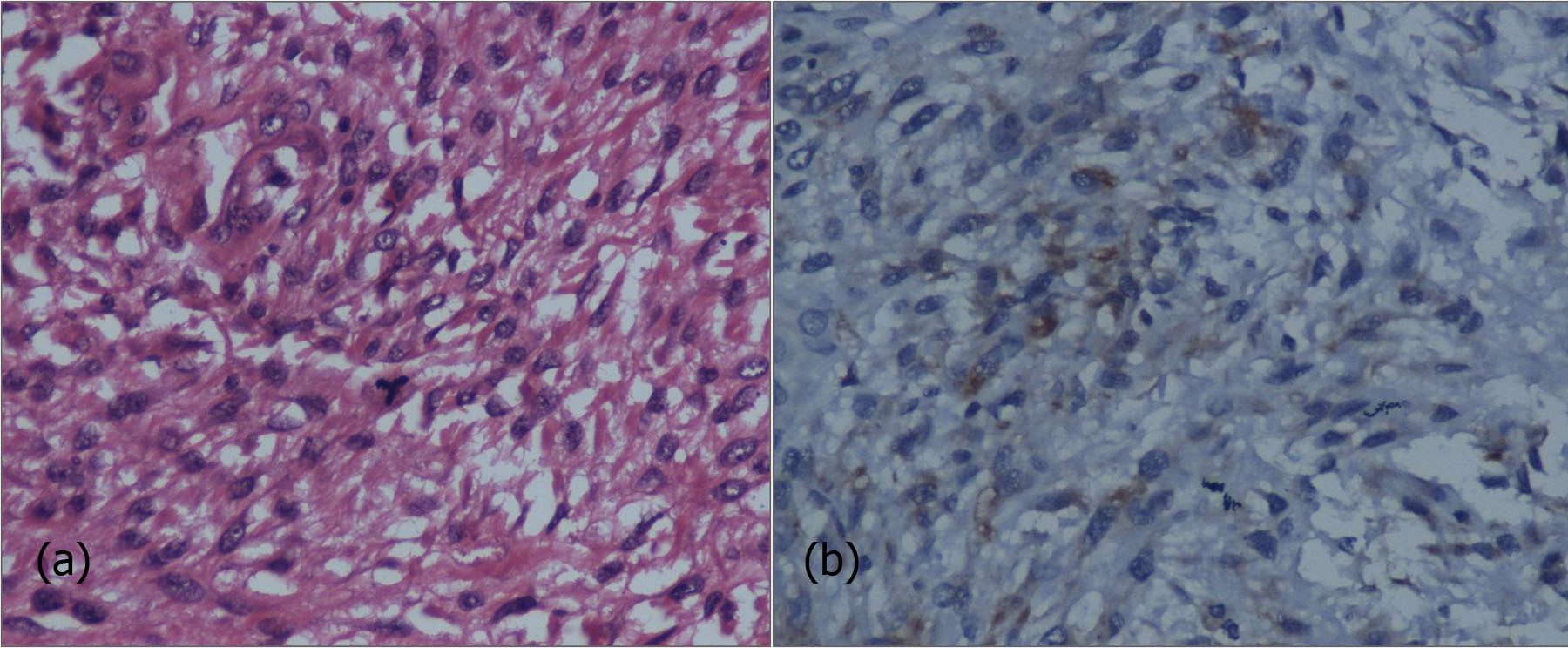
A 45-year-old lady presented with the complaints of a slow growing painless swelling on her left side of back of 1 year duration. The swelling started with an innocuous looking small subcutaneous nodule which was initially ignored by the patient as a harmless lump. The lump progressively enlarged in size to attain the present dimensions[Table/Fig-1]. The patient denied any history of anorexia, weight loss, weakness in the left upper limb or limited mobility of left shoulder joint. She reported inability to lie supine due to sheer size of the lump. Local examination revealed a 13×12 cm spherical swelling on the left lower para-spinal region. The overlying skin was reddened and stretched with coursing prominent superficial veins. The lump was non tender, of variegated consistency, having well defined margins, and freely mobile over the underlying Lattismus dorsi muscle. The chest X-ray of the patient was unremarkable. Magnetic resonance imaging (MRI) lumbosacral spine revealed a 13×12 cm mass having solid and cystic components with internal septations in the subcutaneous tissue of left posterior para-spinal area. The mass was hetrogenously hyperintense on T2 weighted images suggestive of synovial sarcoma [Table/Fig-2]. Core cut biopsy of the lump revealed mesenchymal tumor with spindle cell morphology. Wide local excision of the lump with lateral intercostal artery based rotational flap reconstruction was undertaken [Table/Fig-3]. The patient had an uneventful recovery, and was discharged on 7th post-operative day. The histopathological examination of the excised tumor revealed synovial sarcoma that stained positive for cytokeratin and epithelial membrane antigen [Table/Fig-4]. The patient was advised adjuvant chemo-radiotherapy in view of large size of the tumor; however she did not agree for adjuvant therapy.
Pre- operative photograph of the patient

(a) T2 weighted Magnetic Resonance Imaging (a) axial and (b) Sagittal section displays 13×12 cm hetrogenously hyperintense subcutaneous mass in the left posterior paraspinal area
Discussion
Soft tissue sarcomas (STS) are a heterogenous group of malignant neoplasms of mesodermal origin. They account for less than 1% of all adult malignant neoplasms [1]. Synovial sarcoma is an uncommon variant representing only 7-10% of all STS [2]. Synovial sarcoma does not mean synovial tissue origin of the tumor, rather the histological appearance of tumor cells closely resembles the cells lining the synovial membrane. As in most STS, synovial sarcomas usually present as painless, slow growing, deep seated tumors. The favored site for synovial sarcomas is lower extremity particularly the area around knee joint. The uncommon sites are head and neck, para-vertebral region, intra thoracic, intra abdominal and retroperitoneal location, and chest and abdominal wall [2].
Synovial sarcoma is a rare form of extremity sarcoma characterized by slow growth and high malignant potential. As the name suggests, this tumor is located in the vicinity of the articular surfaces, in close association with the tendon sheath, bursae and joint capsules; however, the articular surface proper is never involved. The tumor is also notorious for arising in aberrant locations away from the joint cavities. This slow growing tumor does not restrict the joint movements and as a consequence diagnosis is often delayed till it attains a significant size or becomes painful. The occurrence of pain is due to the pressure effect of the enlarging mass on the adjacent neurovascular bundle and erosion of bone periosteum. Lungs are the principal site for distant metastasis and in rare instances metastasis to the lymph nodes and skeletal system may be observed [2].
The diagnosis of STS rests on both radiological and histopathological findings. Radiological imaging plays a key role for preoperative diagnosis of synovial sarcoma. Presence of a soft tissue mass laced with peripheral punctuate calcification on plain X-ray is highly suspicious for synovial sarcoma [3]. CECT scan shows a heterogenous septate soft tissue mass with cystic areas and small soft tissue calcific deposits. It also provides useful information about the adjacent bones and draining lymph nodes. MRI is the imaging modality of choice for diagnosis and staging of synovial sarcoma. The advantage of MRI includes full delineation of the tumor mass with accurate information regarding involvement of adjacent muscle compartments, tendons, fascial planes, neurovascular bundles and the skeletal system. Most patients have multilocular lesions with internal septations and tumor calcifications. The demonstration of triple signal density i.e. areas of hyperintensity, isointensity and hypointensity in relation to fatty tissue is unique of synovial sarcoma. This appearance is due to the presence of cystic, solid areas with intra tumoral hemorrhage and fibrosis [3]. Presence of calcifications in the tumor mass is associated with a better prognosis while hemorrhage and triple signal pattern indicate a poor prognosis [4].
(a) Large number of spindle cells with nuclear pleomorphism (b) Epithelial membrane antigen positivity on immunohistochemistry
Post-operative photograph at 4 months of follow up

On histopathological examination three different subtypes of synovial sarcoma are identified. The monophasic type comprises of only spindle cells while the biphasic type is a mixture of spindle cells with epithelioid cells. The third type is the poorly differentiated type which consists of mainly primitive round cells with areas of high cellularity, pleomprphism, increased mitosis, and necrosis [2]. Immunohistochemical staining is routinely done for diagnosis of synovial sarcomas. The spindle cells shows a positive immunoreactivity to epithelial membrane antigen, vimentin, calretinin, cytokeratin, and proliferating cell nuclear antigen; they are negative to smooth muscle actin, CD117 and S 100 [5]. The gold standard for diagnosis is molecular analysis method that identifies the characteristic t(X;18)(p11,2;q11,2) translocation [6]. This is particularly useful for differentiation of sarcomatoid mesothelioma that shares the same immunoreactivity pattern as synovial sarcoma.
Wide local excision with negative resection margins is the desirable treatment for synovial sarcomas. The role of radiotherapy is limited to local disease control. In many patients adjuvant radiotherapy is beneficial in that it allows a conservative limb sparing resection to be carried out. Chemotherapeutic regimens containing ifosfamide and doxorubicin have a beneficial role in controlling the metastatic deposits [7]. Adjuvant radiotherapy and chemotherapy is indicated in high risk individuals having a tumor size > 5 cm, positive resection margins, high histological grade and presence of metastasis.
Early diagnosis and prompt treatment is the key for successful outcome in any malignant process and STS are no exception. Factors that compel the patient to seek early medical attention are presence of pain, visible lump with associated rapid growth, and cosmetic and functional deficits [1]. STS are notorious for delayed diagnosis as they are painless, slow growing, and remain unnoticed for prolonged periods if situated at an unexposed and inaccessible part of the body. More over patients with superficial STS present late in comparison to patients with deep seated STS. Probably the ease of palpation of the superficial lump gives a false sense of assurance to the patient that lump is not harmful. The inability to feel a deep seated lump in its whole extent makes the patient apprehensive about the nature of the lump and to seek early medical opinion. Absence of tell tale signs of malignancy can deceive the unsuspecting physician as in they tend to settle for diagnosis of a more common benign soft tissue swelling. These results in adopting a wait and watch policy, delay in ordering the requisite radiological investigations and not going for wide excision even if resection is planned thus adversely affecting the prognosis.
We would like to conclude that even if we are in the 21st century with all the modern diagnostic armamentarium at our disposal, diagnosis of STS is often delayed due to lack of awareness on the part of the patients and overconfidence on the part of the treating physicians. Adhering to the principles of meticulous history and physical examination and ordering necessary investigations at the slightest possible suspicion will go a long way in achieving a better prognosis for these patients.
[1]. Brouns F, Stas M, Wever ID, Delay in diagnosis of soft tissue sarcomasEur J Surg Oncol 2003 29:440-45. [Google Scholar]
[2]. Weiss SW, Goldblum JR, Synovial sarcoma. In Enzinger and Weiss’s soft tissue tumours 2001 MosbyLondon:309-46.Edited by: Weiss SW, Goldblum JR. [Google Scholar]
[3]. Sheldon PJ, Forrester DM, Learch TJ, Imaging of intraarticular massesRadiographics 2005 25:105-19. [Google Scholar]
[4]. Tateishi U, Hasegawa T, Beppu Y, Satake M, Moriyama N, Synovial sarcoma of the soft tissues: prognostic significance of imaging featuresJ Comput Assist Tomogr 2004 28:140-48. [Google Scholar]
[5]. Nakano J, Yokomise H, Huang CL, Misaki N, Chang SS, Okuda M, Kushida Y, Progressive growth of primary synovial sarcoma of the lungAnn Thorac Cardiovasc Surg 2010 16:194-97. [Google Scholar]
[6]. Clark J, Rocques PJ, Crew AJ, Gill S, Shipley J, Chan AM, Identification of novel genes, SYT and SSX, involved in the t (X;18)(p11.2;q11.2) translocation found in human synovial sarcomaNat Genet 1994 7:502-08. [Google Scholar]
[7]. Randall RL, Schabel KL, Hitchcock Y, Joyner DE, Albritton KH, Diagnosis and management of synovial sarcomaCurr Treat Options Oncol 2005 6:449-59. [Google Scholar]