Anaesthetic Management of a Child with Neurofibromatosis Type 2 for Multiple Tumour Decompressions
Geetha Lakshiminarasimhaiah1, Aniruddha Thekkatte Jagannatha2, Kulyadi Raghavendra Pai3, Ravi Gopal Varma4, Alangar Satyaranjandas Hegde5
1 Assistant Professor, Department of Neuroanaesthesia, Ramaiah Medical CollegeBangalore-560054, Karnataka, India.
2 Assistant Professor, Department of Neuro Surgery, Ramaiah Medical CollegeBangalore-560054, Karnataka, India.
3 Professor and Head, Department of Neuroanaesthesia, Ramaiah Medical CollegeBangalore-560054, Karnataka, India.
4 Professor and Head, Department of Neurosurgery, Ramaiah Medical CollegeBangalore-560054, Karnataka, India.
5 Senior Professor, Department of Neuro Surgery & Director, MS Ramaiah Institute of Neurosciences. Bangalore-560054, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Geetha Lakshiminarasimhaiah, # 281/E, II ‘A’ main, I Phase Girinagar, Bangalore – 560085, Karnataka, India.
Phone: 9611897899,
E-mail: geetha4kiran@yahoo.in
Neurofibromatosis type 2 is a genetic disorder with autosomal dominant pattern. It can manifest as intracranial, spinal, ocular and cutaneous lesions. The lesions can extend to all the systems. We present an anaesthetic management of a paediatric patient with neurofibromatosis 2 for multiple spinal and thoracic tumour decompression.
Neurocutaneous syndrome, Cervical myelopathy, Intrathoracictumour, Videolaryngoscopy, Massive blood transfusion
Case Report
A 9-year-old girl presented with a history of weakness in the right upper and lower limb of 3 months duration. She was born out of non-consanguinous marriage and full term normal delivery. Her developmental milestones were normal. She was 132.5 cms tall and weighed 25 kgs. Physical examination revealed ptosis and miosis in the left eye suggesting horner’s syndrome. She had decreased power, 3/5 in right upper limb and 4/5 in right lower limb. Her reflexes were brisk in bilateral upper and lower limbs. She had horizontal nystagmus in both eyes and mild sensorineural deafness. Airway examination revealed prominent teeth, neck tilt to right side and congestion of posterior pharyngeal wall.
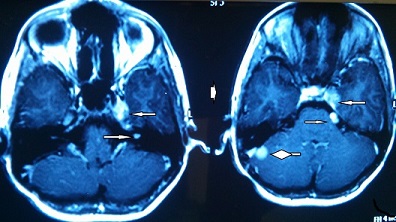
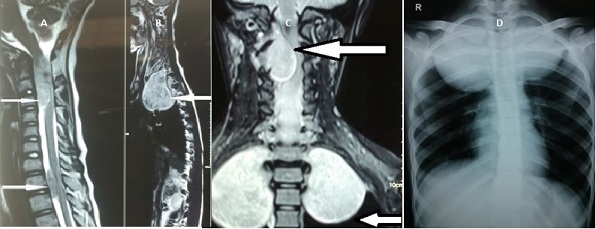
The MRI brain study revealed left vestibular and trigeminal nerve schwannomas and a posterior petrous meningioma on the right side [Table/Fig-1]. The spine MRI study showed intradural extramedullary lesions at C1-C2, C7, D1-D3 levels and multiple tiny lesions in the region of filum terminale [Table/Fig-2]. The dorsal lesions were seen extending to posterior mediastinum. The chest radiograph showed tumours occupying both the apices of the lungs, and on right side the lesion had extended to midzone as well [Table/Fig-2]. These findings lead to the diagnosis of NF2 [1].
MRI brain showing left vestibular and trigeminal nerve schwannomas adjacent to cavernous sinus (small arrows) and a small posterior petrous meningioma on the right side (Rhomboid arrow)
MRI spine (A, B and C) showing intradural extramedullary lesions at C1-C3 and at D1-D3 levels and Posteroanterior Chest radiograph (D) showing tumours occupying both the apices of the lungs.
The patient was scheduled for decompression of the cervicodorsal lesions and excision of the right intrathoracic lesion. ECG, NIBP, ETCO2, nasopharyngeal temperature, Entropy, urine output were monitored. The girl was induced with propofol followed by videolaryngoscopy to see if any lesions were present in the larynx complicating intubation. As no abnormalities were detected, the child was intubated with 6.0 mm size cuffed oral endotracheal tube which was facilitated with vecuronium. Invasive monitors used were right radial artery and left jugular venous pressures. Anaesthesia was maintained with O2, N2O and isoflurane. Analgesia was achieved with intermittent doses of Morphine. Due to massive blood loss estimating to about 2000ml, only cervical tumour was excised and further tumour excision was scheduled later. Intra-operative blood loss was replaced with packed red blood cells and fresh frozen plasma. The vitals were maintained within 20% of the base line values. Post-operatively, the child was extubated and monitored in PICU for two days. A month later, this girl was scheduled for excision of dorsal tumor and its right throracic extension. As proper size double lumen tube was not available for single lung ventilation for thoracic tumour exision, the child was intubated with single lumen 6.0 mm cuffed endotracheal tube. Intraoperatively invasive monitors were initiated and dorsal tumor exision was performed uneventfully. She was positioned in left lateral decubitus position with proper padding to avoid injury to axillary neurovascular bundle. The child was ventilated using air-oxygen mixture and isoflurane with small tidal volumes of 100 -125 ml and respiratory rate of 30-35 min with a PEEP of 4 mm Hg. The EtCO2 and oxygen saturations were maintained between 35-40 mmHg and above 97% respectively. The arterial blood gas analysis showed pH 7.388, pO2 145 mmHg, pCO2 32.6, HCO3 of 21.6. Child was ventilated in PICU for 24 hours and extubated later. Her further hospital stay was uneventful. The histopathology of all the spinal tumors were reported as schwannomas.
Discussion
Neurofibromatosis is an autosomal dominant disorder characterized by congenital malformation of ectodermal tissue and their extensions. It involves abnormal deposition of neural tissue within the nervous system, viscera, endocrine system and skin. It is classified as Neurofibromatosis Type 1 (NF1) and Neurofibromatosis Type 2 (NF2). NF1 affects 1 in 3000 live births whereas NF2 occurs less frequently with the incidence of 1 in 33000 – 40000. NF2 gene is mapped to chromosome 22 where it encodes a cytoskeletal protein dubbed merlin or schwannomin [1]. The type of mutation in the NF2 gene dictates the severity of disease. Because NF2 is of relative rarity and recently recognized as a distinct entity, not many cases concerning the anaesthetic management in pediatric patients are reported.
The majority of patients with NF2 present with hearing loss. However, the first sign of more severe multi-tumour disease in early childhood is often a non-8th nerve tumour. In children, Vestibular Schwannoma accounts for as little as 15-30% of initial symptoms. Some children present with a polio-like illness with wasting of muscle groups in lower limbs. In about 3-5% of patients a more generalized polyneuropathy occurs . Skin features are much more subtle in NF2 than NF1 [2]. In our patient, the main complaints were weakness in right upper and lower limbs. The gold standard for diagnosis is MRI scan of cranial and entire spinal canal. MRI screening of the chest and abdomen to look for extensions of the tumour to thorax or abdomen and compression of adjacent structures is vital.
The anesthetic management of parturients with NF2 presenting for caesarean section with general anaesthesia has been reported [3]. JE Spiegel et al., have described Lumbar epidural anesthesia for caesarean delivery in a NF2 patient [4]. Anaesthetic management of patients with NF2 has not been specifically addressed in paediatric patients.
As NF2 affects both ectodermal and mesodermal tissues, all the systems of the body may be involved. Neurofibromas of the tongue, pharynx or larynx may interfere with tracheal intubation. History of dysphagia, dysarthria, stridor or change of voice may raise the suspicion of possible difficult airway situation in these patients. Laryngeal neurofibromas are extremely rare in NF2, but few such cases have been reported in NF1 [5]. The presence of multiple cervical neurofibromas may itself lead to difficult airway and painless dislocation of cervical vertebra [6]. In our patient, videolaryngoscopy was performed to visualize laryngeal involvement with neurofibromatous lesions and to avoid injury to cervical spine. No mass or deviation of the airway was found and guiding the ET tube was possible without causing much movement of the neck.
The schwannomas are generally vascular tumours which necessitate invasive monitoring of blood pressures in the peri-operative period and good IV access for blood transfusion. This patient required replacement of her entire blood volume and replacement was done with FFPs and PRBCs. Early transfusion of FFPs in patient requiring massive blood transfusion avoids acidosis, hypothermia and coagulopathy [7].
The older children behave like adults in terms of changes in ventilation and perfusion in lateral decubitus position. The dependent lung receives more ventilation and relatively more perfusion and hence the V/Q changes are matched [8]. This patient had both the lungs normal and her pulmonary function tests were normal. We used single lumen 6.0 mm ID, cuffed ETT and ventilated with small tidal volumes. We did not face any issues regarding ventilation during thoracic tumour excision. Arterial blood gas samplings were done which showed normal partial pressures of O2 and CO2.
Conclusion
In summary, we present a case of Neurofibromatosis 2 which is a rare entity who presented with multiple cervicodorsal tumours with intrathoracic extensions managed successfully for tumour excision. A pre-operative discussion involving anaesthesiologist, neurosurgeons, neuroradiologist , ENT and thoracic surgeon helped in better peri-operative management of this case. To our knowledge, there is no case reports of anaesthetic management of multiple tumour excisions in pediatric age group with NF2.
[1]. Ian G, Dorward and Jeffrey R; Youman’s Neurological Surgery 2011 6th editionPhiladelphiaElsevier Saunders [Google Scholar]
[2]. Gareth D, Evans R, Sainio M, Baser Michael E, Neurofibromatosis Type 2J Med Genet 2000 37:897-904. [Google Scholar]
[3]. Sakai T, Vallejo M. C, Shannon K. T, A parturient with neurofibromatosis Type 2: anesthetic and obstetric considerations for deliveryInternational Journal of Obstetric Anesthesia 2005 14:332-35. [Google Scholar]
[4]. Spiegel J. E, Hapgood A, Hess P. E, Epidural anesthesia in a parturient with neurofibromatosis type 2 undergoing cesarean sectionInternational Journal of Obstetric Anesthesia 2005 14:336-39. [Google Scholar]
[5]. Rahbar Reza, Litrovnik Biana G, Vargas Sara O, Robson Caroline D, Nuss Roger C, Irons Mira B, McGill Trevor J, Healy Gerald B, The Biology and Management of Laryngeal Neurofibroma Arch Otolaryngol Head Neck Surg 2004 130:1400-06. [Google Scholar]
[6]. Lovell A.T., Alexander R., Grundy E.M., Silent unstable cervical spine injury in multiple neurofibromatosisAnaesthesia 1994 49:453-54. [Google Scholar]
[7]. Gonzalez Ernest A, Moore Frederick A, Holcomb John B, Miller Charles C, Kozar Rosemary A, Todd S Rob, Cocanour Christine S, Balldin Bjorn C, McKinley Bruce A, Fresh Frozen Plasma Should be Given Earlier to Patients Requiring Massive Transfusion J Trauma 2007 62:112-19. [Google Scholar]
[8]. Hammer Gregory B, New concepts and techniques in pediatric anesthesiaAnesthesiology Clinics of North America March; 2002 20(1):164 [Google Scholar]