Late Postpartum HELLP Syndrome 60 Hours after Delivery Associated with Mild Pre-eclampsia
Bulent Cakmak1, Muhammet Toprak2, Mehmet Can Nacar3, Ahmet Karatas4
1 Department of Obstetrics and Gynecology, School of Medicine, Gaziosmanpasa University.
2 Department of Obstetrics and Gynecology, School of Medicine, Gaziosmanpasa University.
3 Department of Obstetrics and Gynecology, School of Medicine, Gaziosmanpasa University.
4 Department of Obstetrics and Gynecology, School of Medicine, Abant Izzet Baysal University.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bulent Cakmak, Department of Obstetrics and Gynecology, School of Medicine, Gaziosmanpasa University, Tokat, Turkey.
Phone: +905335726978,
E-mail: drbulentcakmak@hotmail.com
The purpose of this report is to present a case of mild Pre-eclampsia which was complicated with postpartum HELLP syndrome. A 25-years-old pregnant woman with mild Pre-eclampsia at 36 weeks of gestation was admitted to our clinic with uterine contractions. A caesarean section was performed, due to her previous caesarean section history. Postpartum period was uneventful until the 2nd day after the caesarean section. Epigastric pain, nausea and vomiting appeared two days after her delivery. In evaluation of the case, laboratory findings which were associated with HELLP syndrome were found to include haemolysis, elevated liver enzymes and low platelet counts. The general condition and laboratory findings of the case returned to normal with supportive and steroid treatment after 3 days. It should be noted that HELLP syndrome can develop in the postpartum period. Therefore, caution should be exercised in patients with pre-eclampsia, for the development of the postpartum HELLP syndrome.
HELLP syndrome, Postpartum period, Pre-eclampsia
Introduction
We are presenting a case of mild Pre-eclampsia which was complicated with postpartum HELLP syndrome after delivery, at the unusual time of postpartum period.
Case Report
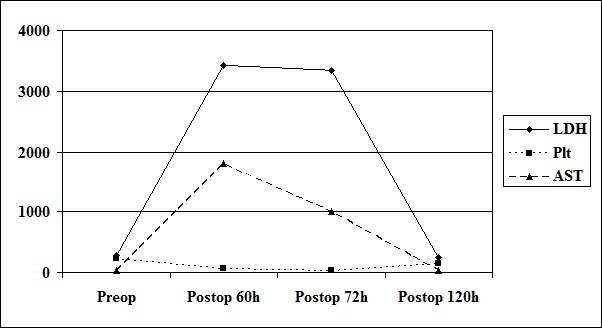
A 25-year-old pregnant woman, gravida 2, parity 1, was admitted to our clinic in the 36th week of gestation, with Pre-eclampsia. No problem was associated with her pregnancy until that time. Her blood pressure was 150/100 mmHg (after 6 hours; 150/90mmHg) and pretibial oedema (++) was detected during her physical examination. All laboratory findings including haematological, biochemical findings and coagulation profile, were within their respective reference intervals [Table/Fig-1]. Proteinuria was found to be 500 mg/dl during routine urine analysis (next day; calculated proteinuria was found 1250mg/24h). According to these findings, the case was considered to be that of mild Pre-eclampsia. Seven hours after her admission to the clinic, uterine contractions started, and cervical dilatation occurred, as 3cm and 90% effacement was examined. For this reason, a caesarean section was performed because of her previous caesarean history. After intravenous hydration with Ringer’s solution (1000 ml), spinal anaesthesia was induced with 10 mg of 0.5% hyperbaric bupivacaine via the L3—4 interspace. A liveborn, 3150 gram, female foetus with a 9 Apgar score in 5th min. was delivered without any complications. An estimated 500 ml of abdominal ascitic fluid was drained during the operation. Blood pressure remained around 150/100 mmHg during caesarean operation. After administration of a slow-release calcium channel blocker such as Nifedipine 30 mg for treatment of hypertension, the blood pressure was reduced to around 140/80 mmHg. Postoperative haematological parameters were unremarkable; haemoglobin -12.0 g/dl and platelet count- 234x103/mm3 after 8 hours of operation. Postpartum period was uneventful until the 2nd day of operation. The patient suddenly experienced epigastic pain, vomiting and nausea at the 52nd hour of postpartum period. Her blood pressure rose to 180/110 mmHg. Haematological parameters were found in normal limitations of references, but biochemical parameters, including ALT, AST and LDH, were detected to be higher than their respective reference intervals; 128 IU/L, 238 IU/L and 1380 IU/L, respectively. The patient was observed for possibility of developing postpartum HELLP syndrome, based on these findings. Intensity of the patient’s symptoms had decreased after 3 hours. The laboratory findings were consistent with those of HELLP syndrome, which included haemolysis (haemoglobin: 8.1g/dl, LDH: 3427IU/L), elevated liver enzymes (ALT: 583IU/L, AST: 1799IU/L), and low platelet counts (platelet: 67x103/mm3) at the 60th hour of postpartum period [Table/Fig-1]. Coagulation profile and other biochemical parameters such as electrolyte values were in normal limitation of references. An ultrasound examination disclosed a normal liver structure without any subcapsular haematoma, and an empty uterine cavity without any placental residue. Magnesium sulphate infusion (2g/hour; two days) and steroids were administered (dexamethasone; totally 30mg for two days), with supportive therapy such as; intravenous fluid, fresh frozen plasma and packed red blood cells. The laboratory findings improved dramatically after the treatment and at the 120th hour (5th day) of postpartum period, all of them completely regressed to normal values [Table/Fig-2]. She was discharged on the 6th day without any sequelae.
Laboratory findings of the case
| Laboratory findings | Preoperative Period | Postoperative Period |
|---|
| 8 h | 52 h | 60 h | 72 h | 84 h | 96 h | 120 h |
|---|
| Hb (gr/dl) | 12.0 | 10.6 | 11.0 | 8.1 | 9.2 | 9.0 | 9.1 | 9.0 |
| Plt (x103/mm3) | 234 | 203 | 151 | 67 | 33 | 54 | 110 | 142 |
| ALT (IU/L) | 17 | -- | 128 | 583 | 394 | 114 | 34 | 24 |
| AST (IU/L) | 27 | -- | 238 | 1799 | 1005 | 518 | 83 | 32 |
| LDH (IU/L) | 283 | -- | 1380 | 3427 | 3347 | 999 | 699 | 252 |
| INR | 0.75 | -- | 0.76 | 1.09 | -- | 0.81 | -- | 0.82 |
Hb: Haemoglobin; Plt: Platelet count; ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; LDH: Lactate dehydrogenase; INR: International normalized ratio of prothrombin time
Change of the laboratory findings over time Plt: Platelet count (x103/mm3); AST: Aspartate aminotransferase (IU/L); LDH: Lactate dehydrogenase (IU/L)
Discussion
The rate of pregnancy-related hypertensive disorders constitute 12-22% of all pregnancies and approximately 17.6% maternal deaths occur for this entity [1]. HELLP syndrome, generally occurs in the presence of Pre-eclampsia. However, approximately 20% of HELLP syndrome cases can occur without Pre-eclampsia. Presence of severe epigastric pain, low platelet counts with high ALT and AST levels arouse suspicion for HELLP syndrome [2]. In our case, because of existence of Pre-eclampsia before the above mentioned symptoms were seen, suspicion of HELLP syndrome was strong in our minds. However, all the signs of HELLP syndrome occurred 12 hours after the occurrence of severe epigastric pain. Epigastric pain, the most important symptom of this syndrome, is the result of stretching of Glisson capsule and the reason of this stretching is obstruction in the sinusoidal blood flow in the liver [3].
There are two conditions, eclampsia and HELLP syndrome, which occur in the postpartum period, which are related to Pre-eclampsia and have been labeled as unwanted by obstetricians and gynaecologists. Eclampsia usually occurs within the first 48 hours after birth. However, in the literature, eclampsia has been reported on the 16th day of the postpartum period [3]. Similarly, approximately 30% of HELLP syndrome occurs in postpartum period and it typically occurs within 48 hours. In this case, the first symptom of postpartum HELLP syndrome emerged at 52nd hours and all symptoms appeared at the 60th hour of postpartum period.
Corticosteroid therapy such as high dose dexamethasone is often used in HELLP syndrome, but there are still controversial reports on it in the literature [4–6]. According to a Cochrane analysis which was done in 2009, there were no significant differences in the primary outcomes of maternal mortality and morbidity caused by placental abruption, pulmonary oedema and liver haematoma or rupture. There was a tendency of platelet count to greatly increase over 48 hours, and of less mean number of hospital stay days with corticosteroid treatment [5]. In addition, there was no clear evidence of any effect of corticosteroids on substantive clinical outcomes [6]. In our clinic, according to our experience, dexamethasone treatment should be considered as a routine in patients with HELLP syndrome. In this case, when we diagnosed HELLP syndrome, immediately, after dexamethasone treatment was started, a dramatic rise in the number of platelets was seen and decline in ALT and AST levels was observed.
In conclusion, when patients present with epigastric pain in postpartum period, it must be kept in mind that it is one of the first signs of HELLP syndrome and if we are aware of this, we can significantly prevent the development of maternal mortality and permanent sequelae.
[1]. Walker JJ, Pre-eclampsiaLancet 2000 356:1260-5. [Google Scholar]
[2]. Sibai BM, Diagnosis, controversies, and management of the syndrome of hemolysis, elevated liver enzymes, and low platelet countObstet Gynecol 2004 103(5Pt1):981-9. [Google Scholar]
[3]. Felz MW, Barnes DB, Figueroa RE, Late postpartum eclampsia 16 days after delivery: case report with clinical, radiologic, and pathophysiologic correlationsJ Am Board Fam Pract 2000 13:39-46. [Google Scholar]
[4]. Haram K, Svendsen E, Abildgaard U, The HELLP syndrome: clinical issues and management. A ReviewBMC Pregnancy Childbirth 2009 9:1-15. [Google Scholar]
[5]. Matchaba PT, Moodley J, WITHDRAWN: Corticosteroids for HELLP syndrome in pregnancyCochrane Database Syst Rev 2009 8(3):CD002076 [Google Scholar]
[6]. Woudstra DM, Chandra S, Hofmeyr GJ, Dowswell T, Corticosteroids for HELLP (hemolysis, elevated liver enzymes, low platelets) syndrome in pregnancyCochrane Database Syst Rev 2010 8(9):CD008148 [Google Scholar]