Ovarian Hyperstimulation Syndrome (OHSS) Presented as Massive Hydrothorax
Pradip Kumar Saha1, Poonam Goel2, Rimpy Tandon3
1 Assistant Professor, Department of Obstetrics & Gynaecology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh, India.
2 Professor, Department of Obstetrics & Gynaecology, Government Medical College & Hospital, Sector-32, Chandigarh, India.
3 Assistant Professor, Department of Obstetrics & Gynaecology, Government Medical College & Hospital, Sector-32, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pradip Kumar Saha, Assistant Professor, Department of Obstetrics & Gynaecology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh, India.
Phone: 91-9914209341,
E-mail: pradiplekha@yahoo.co.in
Ovarian hyperstimulation syndrome (OHSS) is an iatrogenic complication of controlled ovarian stimulation. Although considered uncommon, the severe form is potentially fatal. Patient can present with varied clinical presentation like pain abdomen, abdominal distension or tachypnea. Diagnosis is made by careful history, examination and investigation. Treatment is conservative and supportive care. Here, we have presented a case of severe OHSS which was missed initially, as the doctor who had first seen probably was not aware of this disease.
Ovarian hyperstimulation syndrome, Hydrothorax
Case Report
A 28–year–old nulliparous woman with history of primary infertility for 8 years. On investigation for infertility she was diagnosed to be a case of unexplained infertility. Few occasions she took treatment for ovulation induction drugs but she did not conceive. So she underwent in vitro fertilization (IVF) protocol from a private clinic. Ovulation was induced with gonadotrophin drugs and for final maturation of follicle injection HCG was given. Oocyte retrieval was done 24 hours after HCG injection. Embryo transfer done 48 hours after oocyte retrieval. However, patient was not counseled about the complication of ovulation induction and in vitro fertilization. Four days after embryo transfer she started having abdominal distension and respiratory distress. She went to a chest physician who was unaware about this syndrome and investigated for a possible case of pulmonary tuberculosis. Sputum as well as plural fluid for AFB found to be negative. Mycobacterium serology was negative. She had huge right sided hydrothorax. Empirically she was put on Anti tubercular therapy (ATT). As there was no improvement she was referred to Emergency medical department of our medical college.
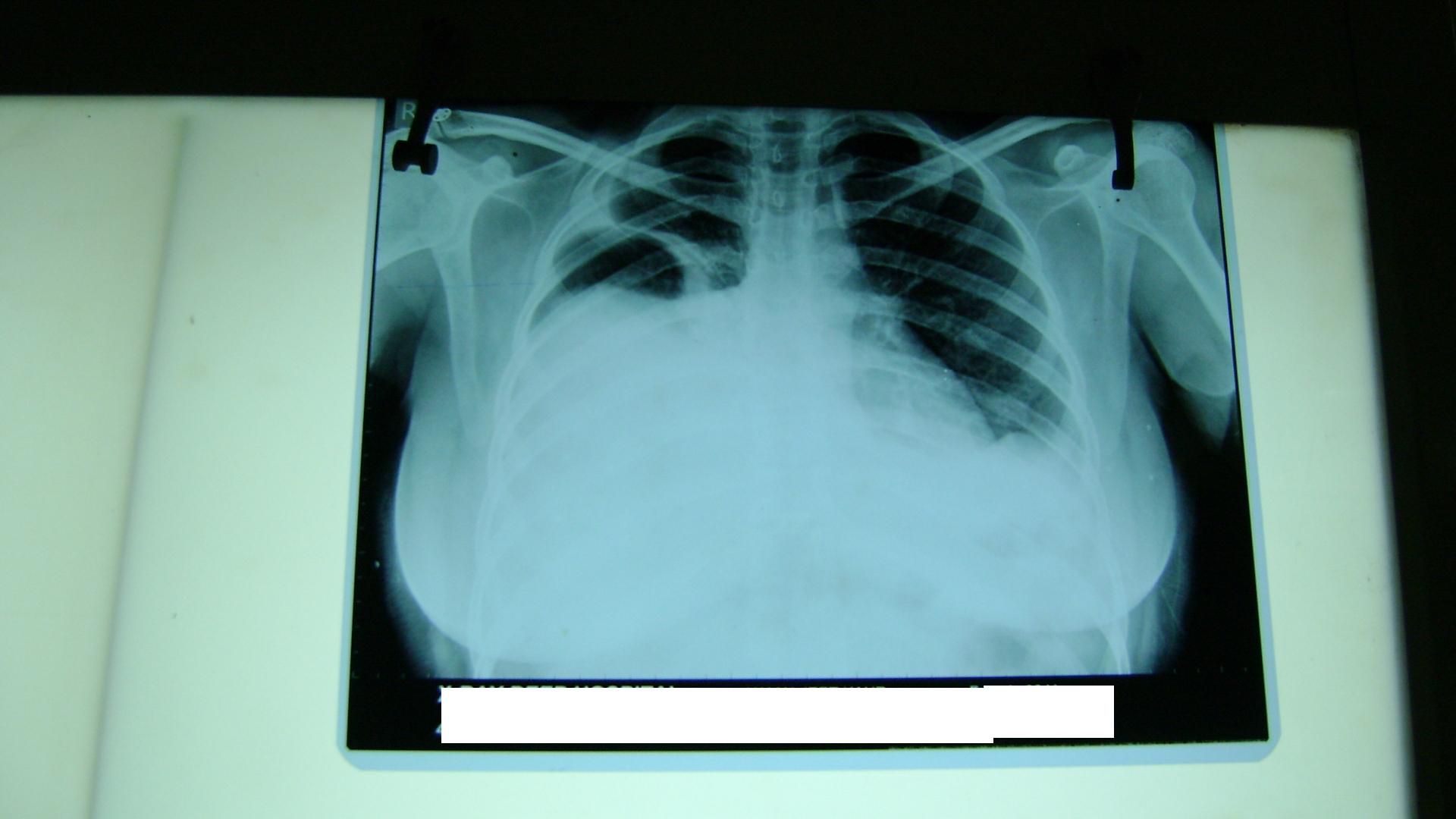
As she is overdue of her period, a Gynaecology consultation was taken and finally diagnosed to be a case of Ovarian hyperstimulation syndrome based on typical history and examination. Her urine pregnancy test was positive and her period of gestation was 6 weeks. On examination there was marked tachycardia (P/R-124/mt) however her BP records were normal. There were marked tachypnea (Respiratory rate 34/mt) and marked distension of abdomen. On investigation her haemoglobin was 14gm% and PCV 40%. She had leukocytosis (Total leukocyte count 16800/cc.), hyponatremia, deranged coagulation profile and mildly elevated Serum bilirubin (sr bilirubin 2.1mg %). On ultrasound ovaries were enlarged with multiple cyst in it [Table/Fig-1] and huge ascites [Table/Fig-2]. On chest X-ray there was huge hydrothorax on right side of the chest [Table/Fig-3]. Ultrasound also showed twin intrauterine gestation[Table/Fig-4].
USG showing multicystic ovary


Chest X-ray showing huge hydrothorax on right side of the chest
Ultrasound showing twin intrauterine gestational sac

Patient was put on conservative management. Intravenous fluid with cristaloid was given. Strict input and output record and her abdominal girth record also maintained. Hydrothorax and ascites was drained and her coagulation profile and hyponatremia was corrected. She was given thromboprophylaxis. Gradually patient became comfortable. Her ascites and hydrothorax as well as her hematological and biochemical parameter improved. However, she aborted 16 days after admission and was discharged 18 days after admission with satisfactory condition.
Discussion
OHSS is a systemic disease resulting from vasoactive products released by hyper stimulated ovaries. Pathophysiology of OHSS is characterized by increased capillary permeability, leading to leakage of fluid from the vascular compartment, with third space fluid accumulation and intravascular dehydration. The incidence of OHSS varies between treatments and patient groups and accurate estimates from the literature are difficult owing to the variety of classification schemes used. The majority of cases of severe OHSS are seen following IVF treatment but the syndrome can occur after any form of supraphysiological ovarian stimulation, including clomiphene and gonadotropins ovulation induction. As many as 33% of IVF cycles have been reported to be associated with mild forms of OHSS [1].
History is very important for diagnosis in such cases. Classic symptoms of moderate to severe OHSS include a sensation of bloating, abdominal pain, rapid weight gain, and decreased urine output. Increasing abdominal pain, oliguria, weight gain, increased girth measurement and breathlessness point to worsening OHSS. Physical examination should include observing signs, body weight, abdominal girth at the umbilicus, and assessment for the presence of pleural effusion, and signs of venous thromboembolic disease, such as unilateral increase in calf diameter. Caution should be taken with pelvic examinations to minimize the risk of trauma to enlarged ovaries. Haemoconcentration is a measure of the severity of OHSS and may be measured by raised haemoglobin and haematocrit [2,3].
In most of the condition Mild forms of ovarian hyperstimulation syndrome (OHSS) do not require treatment and Moderate OHSS should be followed up on an outpatient basis with no specific treatment. However, severe OHSS requires proper evaluation. Investigations are done to evaluate hematocrit, electrolytes, and kidney and liver function. Conservative treatment with intravenous (IV) fluids and close monitoring is usually done. Intensive care admission is indicated in cases with severe respiratory distress or major electrolyte imbalance with elevated serum creatinine. Crystalloids in the form of IV saline and colloids as albumin or hydroxyethyl starch are commonly used to expand intravascular volume. Dopamine can be used to improve diuresis, and prophylactic heparin is administered to prevent venous thrombosis. Diuretics are generally contraindicated because they may further contract intravascular volume. Abdominal or vaginal aspiration of ascitic fluid results in marked improvement of symptoms, improved diuresis, and shortened hospital stay. The current trend to treat patients with IV fluids, albumin, and to perform aspiration of ascitic fluid on an outpatient basis has been found to be a more cost-effective protocol of treatment. Renal failure, thromboembolism, pericardial effusion, and adult respiratory distress syndrome are potential life-threatening complications of OHSS. These conditions should be diagnosed early and managed by a multidisciplinary team possibly in an ICU setting [3–5].
There are some loopholes in this case. Patient was not made aware about symptoms of OHSS, so when the problem occurred she went to physician rather than going to Gynaecologist. Physician who attended first was not familiar about this syndrome leading to delayed diagnosis.
Conclusion
Severe form of OHSS is potentially life threatening. Detail history and clinical examination will diagnose this condition. Proper understanding of the pathology of the disease is imperative. Early diagnosis and prompt treatment will reduce most of the complications. Medical specialist must be aware of this disease as this kind of patient may present to them with ascites or hydrothorax.
[1]. Delvigne A, Rozenberg S, Epidemiology and prevention of ovarian hyperstimulation syndrome (OHSS): a reviewHum Reprod Update 2002 8:559-77. [Google Scholar]
[2]. RCOG Green-top Guideline No. 5 ,September 2006 [Google Scholar]
[3]. Shmorgun D, Claman P, The Diagnosis and Management of Ovarian Hyper stimulation SyndromeJ Obstet Gynaecol Can 2011 33(11):1156-62. [Google Scholar]
[4]. Aboulghar M, Treatment of Ovarian Hyperstimulation SyndromeSeminars in reproductive medicine 2010 28(6):532-39. [Google Scholar]
[5]. Zivi E, Simon A, Laufer N, Ovarian Hyperstimulation Syndrome: Definition, Incidence, and Classification Seminars in reproductive medicine 2010 volume 28(number 6) [Google Scholar]