An Interesting Case of Relapsing Polychondritis in A Young Girl
Shibani V Anchan1, Santosh S Garag2, Arunkumar J S3, K C Prasad4, Poorvi V Sharma5
1 Assistant Professor, Department of Ear, Nose and Throat, SDM College of Medical Sciences and Hospital, Dharwad, Karnataka, India.
2 Assistant Professor, Department of Ear, Nose and Throat, SDM College of Medical Sciences and Hospital, Dharwad, Karnataka, India.
3 Professor, Department of Ear, Nose and Throat, SDM College of Medical Sciences and Hospital, Dharwad, Karnataka, India.
4 Professor, Department of Ear, Nose and Throat, SDM College of Medical Sciences and Hospital, Dharwad, Karnataka, India.
5 Postgraduate, Department of Ear, Nose and Throat, SDM College of Medical Sciences and Hospital, Dharwad, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shibani V Anchan, Assistant Professor, Department of Ear, Nose and Throat, SDM College of Medical Sciences and Hospital, Manjushree Nagar, Sattur, Dharwad- 580009 Karnataka, India.
Phone: 9535010774, Email: shibanikotian@yahoo.com
Relapsing polychondritis is an acute, recurrent and progressive inflammation and degeneration of cartilage and connective tissue including that within the tracheobronchial tree affecting men and women equally and usually in the middle age. Serious airway manifestations occur in at least half of these patients. We present to you an interesting case report of a 20-year-old female who presented with exertional breathlessness. Imaging revealed diffuse calcification of pinna and tracheobronchial tree. Based on the characteristic clinical features and imaging studies a diagnosis of relapsing polychondritis was attained.
Auricular, Chondritis, Laryngotracheal, Polychondritis, Stenosis
Case Report
A 20-year-old female patient presented with exertional breathlessness, nasal obstruction and hardening of the auricles. She subsequently developed discomfort in both the auricles which was insidious in onset and gradually progressive. There was no similar history in the family.
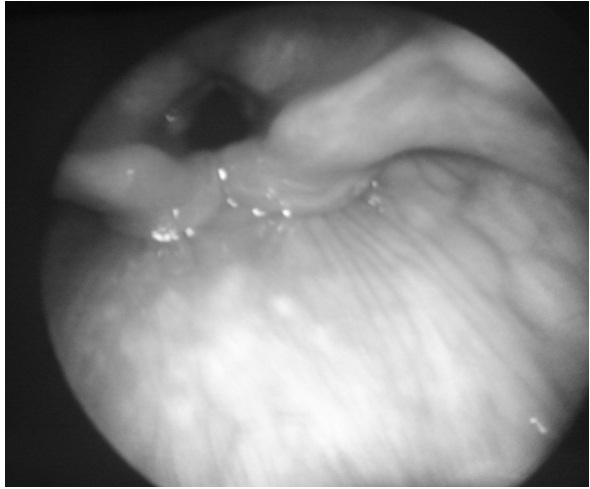
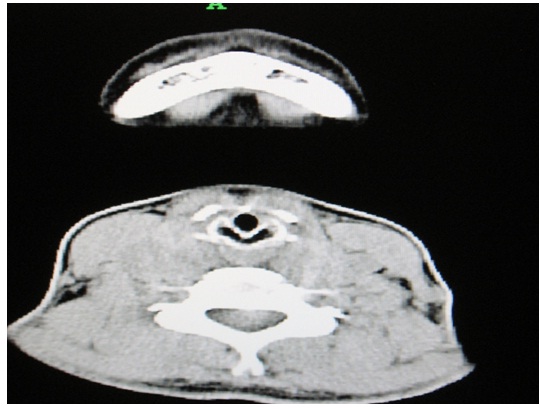
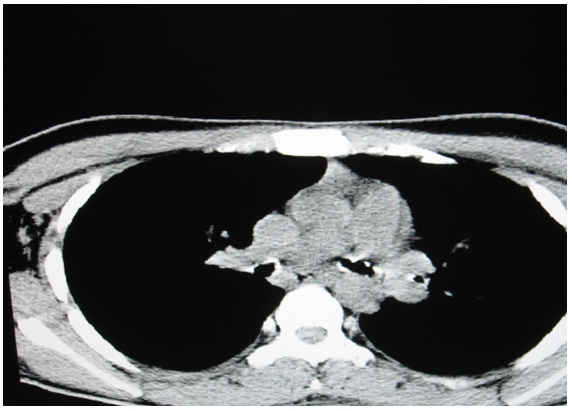
On examination she had a saddle nose deformity. The auricles had a normal appearance but were rigid and had a bony texture and moved as a single unit [Table/Fig-1]. Patient has given consent for publishing clinical photographs. On indirect laryngoscopy the laryngeal inlet appeared to have a shorter anteroposterior diameter with shortening of the vocal cords [Table/Fig-2]. The subglottis appeared stenosed. Diagnostic bronchoscopy was considered to rule out any intraluminal lesions in tracheobronchial tree. A 5mm outer diameter rigid bronchoscope was passed up to the upper trachea and could not be negotiated further. The patient was subjected to an array of radiological tests, blood investigations and histopathological studies. Computerized Tomography (CT) of the neck and chest showed diffuse calcification of elastic cartilages of pinna, nasal cartilage and laryngotracheobronchial tree [Table/Fig-3,4and5] up to the level of segmental bronchioles which accounted for exertional breathlessness in this patient. There was marked thickening of the cricoid cartilage with a symmetric “train-track” calcification pattern and severe subglottic narrowing. The transverse diameter of the larynx at the level of glottis was 6mm and at subglottis it was 5.6mm and at supraglottis it was 9mm. The anteroposterior diameter of trachea was 6mm.There was no significant lymphadenopathy. CT of the paranasal sinuses was done to exclude granulomatous diseases like Wegener’s granulomatosis. There was complete calcification of the cartilaginous portions of both external auditory canals and pinna (confirmed by biopsy from pinna) which resulted in meatal stenosis but pure tone audiometry showed no hearing loss.
Saddle nose deformity and rigid pinna,

Endoscopic view of larynx,
CT scan showing calcified pinna,

CT scan showing calcified laryngeal cartilages,
CT scan showing calcified and stenosed lower airway,
Calcification of the cartilages of the laryngeal framework is known in aged patient, but to present in such a young age was truly intriguing. We were forced to think in terms of rare metabolic, endocrine disorders and hereditary diseases. Systemic conditions like diabetes, hypertension, Addison’s disease, Acromegaly, hypopituitarism, alkaptonuric oochronosis are associated with dystrophic calcification. Diffuse calcification is also seen in sarcoidosis, vitamin D intoxication, hyperparathyroidism, tumoral calcinosis in the presence of hyperphosphatemia. Nasal mucosa was sent for biopsy to rule out scleroma. Split skin smear was done to rule out leprosy. Venereal disease research laboratory test was negative. Routine blood investigation showed a normochromic normocytic type of blood picture. Erythrocyte sedimentation rate was elevated and rheumatoid factor was within normal limits. Blood urea and serum creatinine, serum calcium and phosphate, serum electrolytes, alkaline phosphatase, uric acid, free thyroxine and triiodothyronine were within normal limits. This ruled out a host of metabolic disorders.
RP can be diagnosed based on common clinical features like auricular chondritis, nonerosive sero-negative inflammatory polyarthritis, nasal chondritis, ocular inflammation, respiratory tract chondritis and audiovestibular damage. McAdam proposed that the diagnosis is certain if three or more of the above mentioned features are present together with histologic confirmation [1]. Damiani and Levine later suggested that the diagnosis could be made when one or more of the above features and a positive biopsy was present, when two or more separate sites of cartilage inflammation were present that responded to steroids or Dapsone, or when three or more of the above features were present [2]. Auricular chondritis and arthropathy are the most common presentations of RP. Almost 50% of the patients present with either arthropathy or auricular chondritis but with prolonged follow-up, a majority of patients develop ocular, respiratory and audiovestibular symptoms [1]. Laboratory and radiographic investigations usually show no characteristic abnormalities.
Patient was put on a course of intravenous Prednisolone 40mg/day for 1 week and given tapering dose of prednisolone for 1 week on discharge. Patient was on follow up for one year with no remission during this period. Corticosteroids have decreased the frequency, duration, and severity of breathlessness in this patient.
Discussion
Systemic diseases like Addison’s disease, hypopituitarism, thyroid or parathyroid disorders can present with ectopic calcification of cartilage following local trauma. Diffuse tracheobronchial narrowing may result from RP, ulcerative colitis, amyloidosis, sarcoidosis, Wegener’s granulomatosis (WG). Fifty nine percent of WG patients with airway abnormality with subglottis are most frequently involved [3]. CT scan usually shows focal or diffuse wall thickening and airway narrowing.
In Tracheopathia osteochondroplastica, multiple osteocartilaginous masses are seen adjacent to the inner anterolateral wall of the trachea. It does not involve the posterior membranous portion of the trachea as opposed to RP or amyloidosis. CT may show focal tracheal thickening, calcification of the tracheal rings, calcified tracheal nodules, and tracheal stenosis [3]. Five percent of Tracheobronchial papillomatosis present with laryngeal and upper airway lesions. CT may reveal intraluminal masses, parenchymal nodules or thick-walled cavities [3,4]. Other infections such as tuberculosis, coccidioidomycosis, histoplasmosis, mucormycosis, and rhinoscleroma can also present with focal airway narrowing.
RP is an uncommon disorder of unknown origin usually seen in the fourth and fifth decade of life with no sex predilection. The predominant clinical features include recurrent painful swelling of the external ear and nose, uveitis and peripheral arthropathy. It can also present with glomerulonephritis, sensorineural hearing loss, cardiac abnormalities and skin lesions. Involvement of the nose results in a classic “saddle nose” deformity of the nasal bridge. Morbidity and mortality is usually due to recurrent pulmonary infections in these patients [3]. The respiratory tract is involved in approximately half of the patients with clinical symptoms of dyspnea, cough, wheezing, stridor, and dysphonia [5,6]. A prospective case series of 23 patients by McAdam et al.,has shown that 14% of patients have respiratory symptoms at initial presentation. Patients with respiratory involvement have a more fulminant course of disease that is less responsive to steroid treatment [1]. Respiratory distress may occur due to collapse of the airway from destruction and fibrosis of the laryngeal and tracheal cartilages. Kent et al., has reported that 43% of patients present initially with auricular chondritis, 32% with arthritis, 21% with nasal chondritis, 18% with ocular inflammation, 23% with Laryngotracheal symptoms, 7% with reduced hearing, 11% with saddle nose, and 15% with larygotracheal strictures [7].
CT is the most useful imaging technique for identifying cartilaginous and soft-tissue structures pathology and evaluation of both upper and lower airways [6, 8]. Typical CT findings of RP include subglottic stenosis, tracheal stenosis due to densely calcified and thickened tracheal cartilage, peripheral bronchial narrowing and bronchiectasis, calcifications of the pinnae, and nasal cartilage collapse. The most frequent CT manifestations are increased attenuation and smooth thickening of the airway walls [6].
Some patients with chondritis and arthritis get relief with Dapsone 50–100 mg/d. Role of immunosuppressive agent in RP is limited. Rapid dissolution of cartilage can be prevented by early use these agents. It should be reserved for patients with severe organ-threatening disease or patients with poor response to prednisone. The 5- and 10-year probabilities of survival after diagnosis are 74% and 55%, respectively [9].
Conclusion
A rare disease relapsing polychondritis presenting even rarer in a young girl was diagnosed based on McAdam`s criteria. Treatment with prednisolone has led to symptom free interval in this patient which has further supported the diagnosis.
[1]. McAdam LP, O’Hanlan MA, Bluestone R, Pearson CM, Relapsing polychondritis: prospective study of 23 patients and a review of the literatureMedicine 1976 55:193-215. [Google Scholar]
[2]. Langford Carol, Harrison’s principles of internal medicine Relapsing polychondritis Chapter 18th edition vol 2 328 2802-05 [Google Scholar]
[3]. Edith M Marom, Philip C. Goodman, McAdams H. Page, Diffuse abnormalities of trachea and main bronchiAJR March 2001 176:713-17. [Google Scholar]
[4]. Gruden JF, Webb R, Sides DM, Adult-onset disseminated tracheobronchial papillomatosis: CT featuresJ Comput Assist Tomogr 1994 18:640-42. [Google Scholar]
[5]. Ernst A, Rafeq S, Boiselle P, Sung A, Reddy C, Michaud G, Relapsing polychondritis and airway involvementChest 2009 Apr 135(4):1024-30. [Google Scholar]
[6]. Laura E Faix, Barton F Branstetter, Uncommon CT Findings in Relapsing PolychondritisAJNR 2005 26:2134-36. [Google Scholar]
[7]. Kent Peter D, Clement J. Michet Jr, Luthra Harvinder S, Relapsing PolychondritisCurr Opin Rheumatol 2004 16:56 [Google Scholar]
[8]. Tillie-Leblond I, Wallaert B, Leblond D, Respiratory involvement in relapsing polychondritis: clinical, functional, endoscopic, and radiographic evaluationsMedicine 1998 77:168-76. [Google Scholar]
[9]. Michet CJ Jr, McKenna CH, Luthra HS, O’Fallon W M, Relapsing polychondritis. Survival and predictive role of early disease manifestationsAnn Intern Med 1986 Jan 104(1):74-78. [Google Scholar]