Rare Retro-Orbital Intraconal Occurrence Of Benign Schwannoma – A Case Report
A.L. Hemalatha1, Vani D2, Giripunja M3, Bharathi M4, Geetanjali S5
1 Professor & Head, Department of Pathology - RGUHS, Mysore Medical College and Research Institute, Mysore, India.
2 Assistant Professor, Department of Pathology - RGUHS, Mysore Medical College and Research Institute, Mysore, India.
3 PG Student, Department of Pathology - RGUHS, Mysore Medical College and Research Institute, Mysore, India.
4 Professor, Department of Pathology - RGUHS, Mysore Medical College and Research Institute, Mysore, India.
5 PG Student, Department of Pathology – RGUHS, Mysore Medical College and Research Institute, Mysore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. A.L. Hemalatha, No.156, 12th Cross, 2nd main, jayanagar, Mysore- 570014, Karnataka, India.
Phone: 9964016014,
E-mail: halingappa@gmail.com
Schwannomas otherwise referred to as neurilemmomas are benign, slowly progressing, encapsulated tumors arising from Schwann cells in the peripheral nerve sheath. They may grow along any peripheral or cranial nerve. Amongst the cranial nerve schwannomas, the eigth cranial nerve is the commonest site. But orbit is a rare site for their occurrence. Solitary orbital schwannomas account for 1% of orbital neoplasms. Orbital schwannomas arise from 3th, 4th, 6th cranial nerves and ciliary ganglion. Since complications like optic nerve compression and atrophy are likely to occur, early diagnosis is imperative for appropriate management. The present case deals with the rare occurrence of a retro-orbital, intraconal schwannoma in a 23-year-old lady who was clinically and radiologically diagnosed to have a retro-orbital cavernous hemangioma. The variable presentation and location of this tumor can certainly make the diagnosis difficult which may be confirmed only by histopathological examination as in the present case. Our patient underwent a successful complete surgical excision before any complications could ensue.
Schwannoma, Intraconal, Retro-orbital
Case Report
A 23-year-old female patient presented to the ophthalmic department with painless, progressive forward protrusion of the right eye [Table/Fig-1] which developed progressively over a period of four years. There was no history of headache, diminution of vision or diplopia. There was no history of diurnal variation or change in proptosis either on coughing or straining. The past history and the family history were not contributory. Systemic evaluation was done to rule out the signs of neurofibromatosis.
Clinical picture of the 23-year-old female patient with proptosis of right eye

On ophthalmic examination, the eye movements were not restricted and no orbital mass could be palpated. Exophthalmometry revealed a forward proptosis of 2.5mm. The visual acuity was 6/6 in both the eyes. Fundoscopy of the right eye showed blurred disc margins and mildly engorged veins around the disc.
Ultrasound examination of the right eye revealed a retro-ocular hyperechoic mass with well- defined margins.
CT scan showed an intraconal, oval, slightly hyperintense lesion, medio-laterally measuring about 24x15mm in size with intra-lesional hyperintense foci in the right orbit. Margins of the lesion were well made out. The lesion was present postero- inferiorly to the globe as seen in axial and coronal sections [Table/Fig-2]. The clinico-radiological diagnosis was Retro-orbital Intraconal Cavernous hemangioma.
CT showing left eye with intraconal hyperintense lesion
Right lateral orbitotomy was performed and per-operatively, a well encapsulated, retro-ocular mass was found separate from the optic nerve which was easily dissected and excised. Post-operatively, visual acuity in the right eye remained at 6/6.
Gross examination of the excised mass showed a well– encapsulated, gray white tumor with smooth surface measuring 2.5 X 2cms [Table/Fig-3]. Cut surface was gray white, glistening with focal hemorrhagic areas [Table/Fig-4].
Well encapsulated tumor measuring 2.5 X 2 cms

Cut section- completely encapsulated, gray-white, glistening with focal hemorrhagic areas

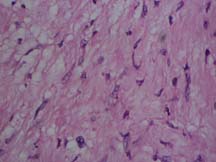
Histopathological examination of the excised mass showed a large, encapsulated, spindle cell tumor with admixed hypocellular ( Antony B ), myxoid, and hypercellular ( Antony A ) areas [Table/Fig-5]. The tumor cells showed bland, oval to spindly, wavy and buckling nuclei [Table/Fig-6] forming palisades at places. Also seen admixed were dilated and congested blood vessels. Immunohistochemistry showed positivity for S-100 protein.
Hypercellular (Antoni-A) areas and Hypocellular (Antoni-B) areas

H&E, 40X : Spindled tumor cells with bland oval to wavy nuclei with buckling
With these features, the final diagnosis of Benign Orbital Schwannoma was arrived at.
During a follow up six months after tumor excision, the patient was asymptomatic and healthy.
Discussion
Orbital tumors have always remained an enigma posing diagnostic challenges to the ophthalmologists as in the present case. Tumors of neurogenic origin are rare in the orbit and account for about 1% of all orbital tumors [1,2]. To quote Duke Elder, “Orbital neurilemmoma is so rare as to be a curiosity” [3,4]. Orbital shwannomas are associated with neurofibromatosis type I in about 1.5% of the patients. Extensive literature search also revealed that, only a few case reports of orbital schwannomas are intraconal. Orbital schwannomas are tumors of adulthood with the mean age of presentation at 40 years [5]. They are localized, usually unilateral and rarely malignant.
Orbital schwannomas may present with varied combinations of signs and symptoms due to the variability in origin and location of the tumor. Orbital schwannomas are usually asymptomatic when small and may produce progressive, painless proptosis on enlargement as in the present case. Their most common presenting features include exophthalmos, restriction of ocular mobility and diplopia [5,6]. Clinical presentation of the lesions near the orbital apex may simulate retro-orbital neuritis. Besides these, pressure effects such as papilledema and optic nerve atrophy may also be found [7]. Therefore, early diagnosis and treatment are indicated to avoid the complications related to progressive growth of the tumor. The present case did not manifest with any such complications.
The chances of recurrence, intracranial extension and malignant transformation are higher if the tumor is highly cellular on histology or, whenever the tumor is removed piecemeal [8]. However, the tumor in the present case was not completely hypercellular and was excised in totality. Hence ,the chances of these complications seem remote.
Conclusion
Orbital Schwannoma, despite being a rare entity has to be considered under the differential diagnosis of all orbital tumors, because of the dismal complications which may follow suit.
[1]. Khetan VD, Giant subperiosteal orbital Schwannoma with luxated globeJ Clin Ophthalmol Res [serial online] 2013 [cited 2013 Sep 17] 1:159-62. [Google Scholar]
[2]. Kinger Arvind, Kawatra Mallika, Chaudhary TS, Chaudry Anitha, Plexiform schwannoma of infraorbital nerve – A rare case reportIJB 2013 Vol 2(No 3) [Google Scholar]
[3]. Spencer W.H., Ophthalmic Pathology: An Atlas and Textbook 1996 4th editionPhiladelphia, Pa, USAWB Saunders [Google Scholar]
[4]. Asrani S G, Jehangir R P, Adrianwala S D, Sane S Y, Benign orbital neurilemmoma, (a case report)J Postgrad Med 1991 37:121 [Google Scholar]
[5]. Grover A K, Rastogi A, Chaturvedi K U, Gupta A K, Schwannoma of the orbitIndian J Ophthalmol 1993 41:128-9. [Google Scholar]
[6]. Dulani Somya, Diagavane Sachin, Lele Seema, Gaurkhede Harshal, “A Bilobed Schwannoma in Roof of Orbit: A Rare Case Report,” Case Reports inOphthalmological Medicinevol. 2012Article ID 139241, 4 pages, 2012. doi:10.1155/2012/139241 [Google Scholar]
[7]. Brucoli M, Giarda M, Arcuri F, Benech A, A benign isolated schwannoma of the orbitJ Craniofac Surg 2011 Nov 22(6):2372-4. [Google Scholar]
[8]. Garg R, Dhawan A, Guptha N, D’souza P, A rare case of benign isolated schwannoma in the inferior orbitIndian J Ophthalmol 2008 Nov-Dec 56(6):514-15. [Google Scholar]