Cryptococcososis of Bone Marrow: A Case Report with Review of Literature
Ashwini B.R1, AR Raghupathi2, Srinarthan A.3
1 Assistant Professor, Department of Pathology, Bangalore Medical College & RI, Bangalore, India.
2 Professor and Head, Department of Pathology, Bangalore Medical College & RI, Bangalore, India.
3 Post Graduate, Department of Pathology, Bangalore Medical college &RI, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ashwini B R., Assistant Professor, Department of Pathology, Bangalore Medical College & RI, Fort Bangalore-560002, India.
Phone: 9886362173,
E-mail: dr_ashwinibr@yahoo.co.in
Cryptococcus has been increasingly seen as a pathogen with the growing incidence of Acquired Immune Deficiency Syndrome (AIDS). Cryptococcosis commonly presents with pulmonary, CNS or skin involvement. Bone marrow involvement of Cryptococci has been rarely reported. We are reporting a case of bone marrow Cryptococcosis in a 50–year–old Human Immune Deficiency Virus (HIV) positive male, with review of literature.
Bone marrow examination, Trephine biopsy, Cryptococcosis
Case Report
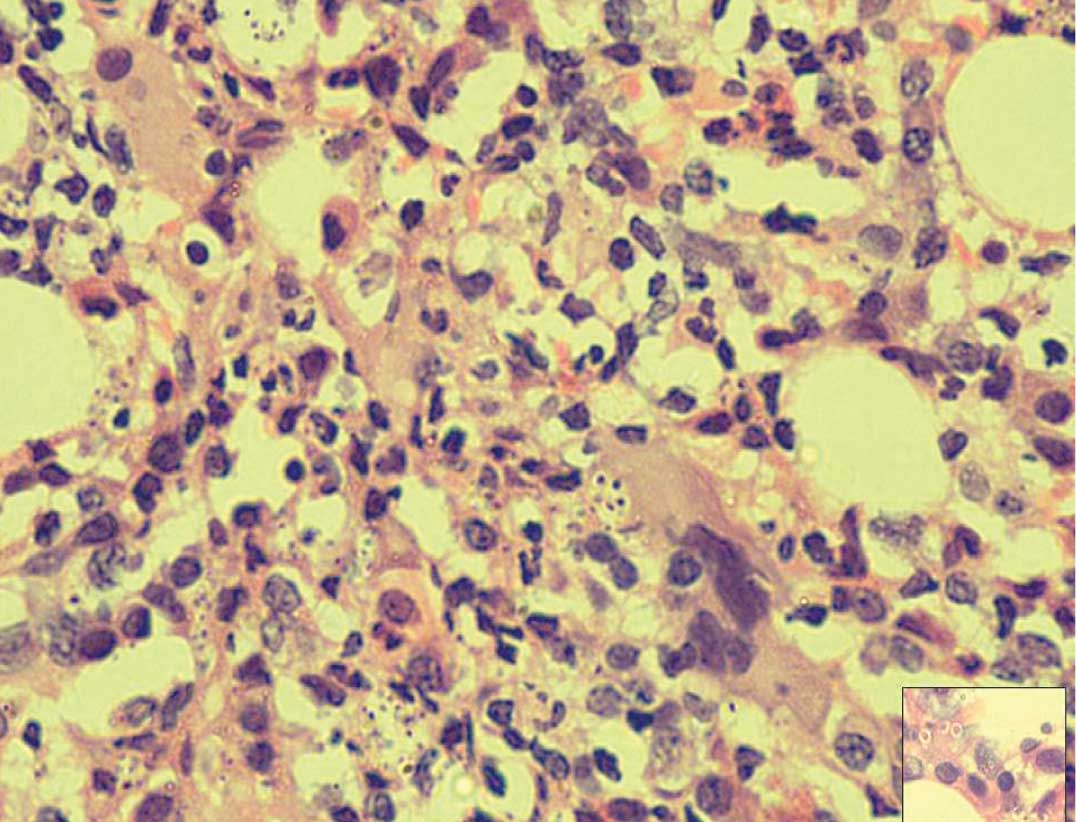
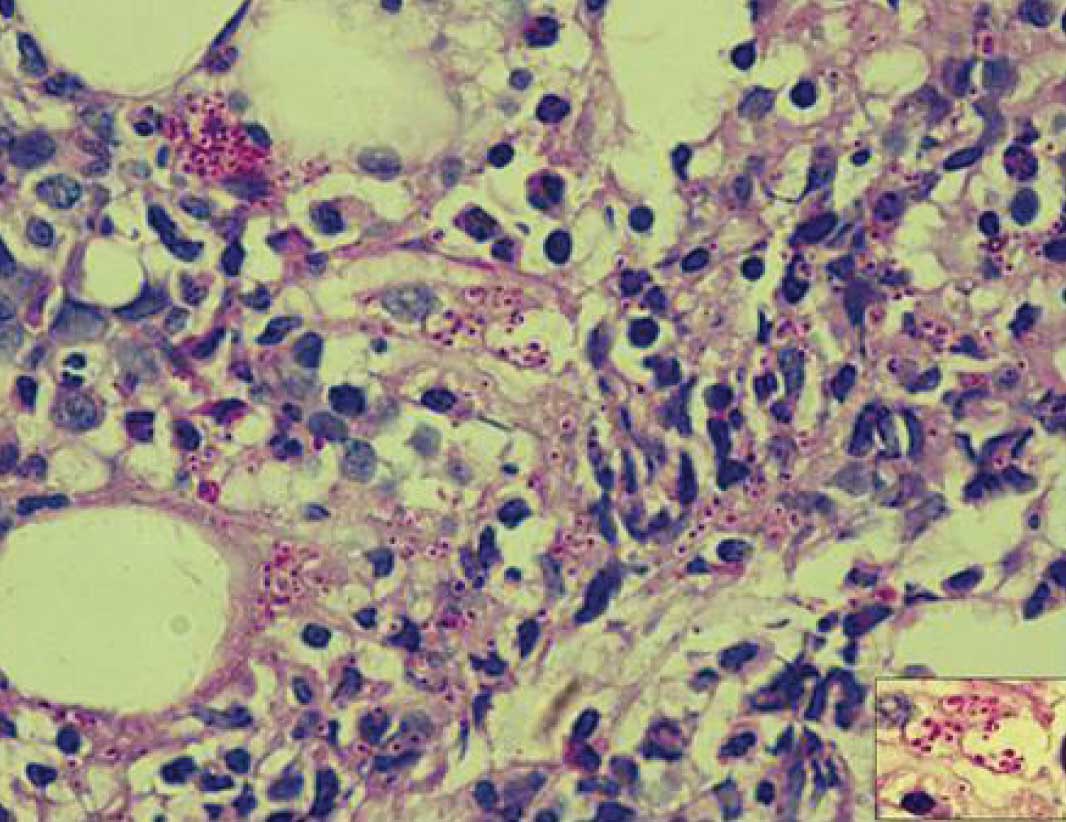
A 50-year-old male patient was referred to our hospital for evaluation of thrombocytopaenia. He had fever since one month, with chills and rigour. He had cough since one week and loose stools since three days. He was recently diagnosed to have an HIV positive status and his CD4 counts were 20 cells/cumm. He was not on anti-retroviral therapy. He did not have any history of headache or vomiting. On examination, patient was found to be conscious, oriented and he obeyed commands. Pallor, mild icterus and dependent oedema were present. Oral cavity showed candidiasis. His blood pressure was 70/50 mm of Hg and his pulse was 68/ min. Systemic examination showed no organomegaly, with normal vesicular breath sounds. Central Nervous System (CNS) examination was within normal limits. His liver function test showed aspartate aminotransferase 121 IU/L, alanine transaminase: 66 IU/L, alkaline phosphatase: 79 IU/L, total bilirubin: 0.9 mg/dl, direct bilirubin: 0.3 mg/dl, total proteins: 5.1gms/dl, albumin: 2.0gms/dl, globulin: 3.1gms/dl. His electrolytes showed Na: 126mEq/L, K: 2.7mEq/L, Cl: 104mEq/L. Complete haemogram of the patient showed Haemoglobin: 8.4gm% (13-17%), haematocrit: 25.5%, total leucocyte count: 1,800/cumm (4000-11,000/cumm), platelet count: 19,000/cumm (1.5-4.5 lakhs/cumm). Bone marrow aspiration and biopsy were done to evaluate pancytopaenia using 18 gauge needle. The bone marrow aspiration and biopsy showed a hyper cellular marrow with an M:E ratio of 1.2:1. Bone marrow aspirate showed erythropoiesis with a normoblastic pattern of maturation and megaloblastic changes. Myelopoeisis showed an increase in intermediate precursor form, with myelocytes and metamyelocytes. Megakaryocytes were increased in number and they had normal morphologies. Lymphopoiesis and plasma cells were mildly increased in number and they had normal morphologies. Occasional macrophages with intra-cellular and few extra-cellular clusters of capsulated yeast forms were seen. No granulomas were seen on aspirate [Table/Fig-1]. Bone marrow biopsy showed a hypercellular marrow, with increase in all three cell lineages, with numerous clusters of capsulated yeast forms [Table/Fig-2]. A majority of the yeast forms were extracellular. No granulomatous response was seen on bone marrow biopsy. The capsulated yeast forms were Periodic Acid Shiff (PAS) positive [Table/Fig-3]. Gomori’s Methenamine Silver (GMS) positivity was also seen. A diagnosis of cryptococcosis of bone marrow was made. The patient was discharged against medical advice and no further follow up was available.
Bone marrow aspirate showing both intra-cellular and extra-cellular capsulated yeast forms. (Leishmann stain, 100x)

Bone marrow biopsy showing numerous large clusters of capsulated Cryptococci amidst the marrow cells. (H&E, 40X). Inset showing extra-cellular Cryptococci with thick capsule. (H&E, 100X)
[A] Large aggregates of Cryptococci showing Periodic acid shiff positivity. (PAS stain 40x). Inset showing magenta coloured aggregates of cryptococci (PAS, 40X).
Discussion
Cryptococcosis is an important cause of morbidity and mortality in immun-ocompromised hosts and it is the second most common fungal infection which complicates acquired immunodeficiency syndrome (AIDS). Cryptococcosis commonly presents with pulmonary, central nervous system or skin involvements. Hepatic, prostatic and bone marrow involvements are rarely reported [1,2]. The annual incidence of cryptococcosis ranges from 1.7- 6.6% in AIDS patients, with fungal meningitis as the commonest presentation. Only few cases of bone marrow cryptococcosis have been reported and its exact incidence is not known. The diagnosis can be established by isolation of the organism in culture, by studying specific biochemical reactions or by a histopathological examination of the tissue with PAS and GMS or mucicaramine positivity or by detection of the polysaccharide capsular antigen [3].
Bone marrow examination plays a critical role in diagnosing opportunistic fungal infection like cryptococcosis as a cause of pancytopenia in immunosuppressed individuals. Cryptococcus acts synergistically with HIV to cause cytopaenias [4]. The polysaccharide capsule of Cryptococcus is immunosuppressive, which results in low CD4 counts [5]. Cases of disseminated cryptococcosis with both good granulomatous response and no granulomatous response in bone marrow, have been reported [4]. Our patient did not show any granulomatous response. The number of Cryptococcus is inversely proportional to the granulomatous response [4]. The presence of the granulomatous response, in turn, is dependent on the CD4 levels in the patients. The decrease in the CD4 cell counts to below 100/cumm in AIDS patients makes them vulnerable to infections caused by cryptococcus [6]. Due to the granulomatous response and fibrosis, bone marrow aspirate alone is less useful in cryptococcosis. When a bone marrow examination is indicated, both an aspiration and a trephine biopsy must be done in the same setting. The trephine biopsy may show granulomas or fibrosis, which are not seen in aspirate. Thus, the detection rate of Cryptococcus is much higher in trephine biopsies [7]. Although our case showed no granulomatous response, very occasional Cryptococci were seen on aspirate, but numerous clusters of Cryptococci were seen on bone marrow trephine biopsy, which stressed the importance of trephine biopsies. The occurrence of fewer Cryptococci in the aspirate in the absence of granulomas was a very unusual finding and it could not be explained easily in our case. Cryptococcus has a gelatinous polysaccharide capsule. The polysaccharide capsule can result in a gelatinous mass or a pseudocyst formation, with numerous Cryptococci within the pool of mucin [8]. Our hypothesis was a probable resistance to aspirate by the mucinous material to a narrow gauge needle and a more wide bore needle may be required in suspected cases of Cryptococci. However, a more detailed study is essential in this regards, to make a definitive conclusion.
[1]. Taneja Juhi, Bhargava Aradhna, Loomba Poonam, Dogra Vinita, Thakur Arhana, Mishra Bibhabati, Cryptococcal granulomas in an immunocompromised HIV- negative patientIJPM 2008 51(4):553-55. [Google Scholar]
[2]. Agarwal V, Atul S, Gautam A, Harsh M, Anjali Disseminated cryptococcosis mimicking lymphoreticular malignancy in a HIV negative patientJK Science 2004 6:93-5. [Google Scholar]
[3]. Srinivas Upendra, Kar Rakhee, Saxena Renu, Prasad Pati Hara, Cryptococcal neoformans profiles in peripheral blood neutrophils: An unusual presentationIJPM 2008 51(2):296-97. [Google Scholar]
[4]. Pantanowitz L, Omar T, Sonnendecker H, Karstaedt AS, Bone marrow cryptococcal infection in the acquired immunodeficiency syndromeJ Infect 2000 Jul 41(1):92-4. [Google Scholar]
[5]. Muller J, Immunological aspects of cryptococcosis in AIDS patients. In: Vanden Bossche H et al, edsMycoses in AIDS patients 1990 New YorkPlenum Press:123-32. [Google Scholar]
[6]. Jung Alan C, Paauw Douglas S, Diagnosing HIV-Related Disease Using the CD4 Count as a GuideJ Gen Intern Med 1998 February 13(2):131-36. [Google Scholar]
[7]. Bain B.J, Bone marrow trephine biopsyJ Clin Pathol 2001 54:737-42. [Google Scholar]
[8]. Kovoor Jerry M.E., Mahadevan Anita, Narayan Jayakumar P, Govindappa Srikanth S., Satishchandra P., Cryptococcal Choroid Plexitis as a Mass Lesion: MR Imaging and Histopathologic CorrelationAJNR 2002 23:273-76. [Google Scholar]