Myxoid Leiomyoma of Cervix
Hemlata T Kamra1, Sunita S Dantkale2, Khusboo Birla3, Pankaj W Sakinlawar4, Rahul R Narkhede5
1 Associate Professor, Department of Pathology, BPSGMC, Khanpur, India.
2 Associate Professor, Department of Pathology, GMC, Latur, India.
3 3rd Postgraduate, Department of Pathology, GMC, Latur, India.
4 3rd Postgraduate, Department of Pathology, GMC, Latur, India.
5 3rd Postgraduate, Department of Pathology, GMC, Latur, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hemlata T Kamra, Associate Professor, Department of Pathology, B-15,BPS GMC campus,Khanpur
Phone: 8221883255,
E-mail: hemlatamunde@rediffmail.com
Leiomyoma, a benign smooth muscle tumour of uterus, is the most common pelvic tumour which occurs in women of reproductive age group. Uterine leiomyomas are frequently seen in women who are older than 30 years of age and they are very rarely seen in women who are below the age of 18 years. They tend to regress after menopause. Incidence is 4% in women who are below 30 years of age. However , lifetime risk of fibroids in women who are over the age of 45 years is more than 60%, with an incidence which is higher in blacks than in whites Cervical leiomyomas constitute 1-2% of the total leiomyoma cases and they rarely occur. There are three types of cervical leiomyomas, namely; interstitial, supravaginal, and polypoidal. Supravaginal leiomyoma is the commonest type. Large cervical fibroids present with abdominal masses, incarcerated procidentia, uterine inversion, cervical malignancy, etc. The prevalence of fibroids during pregnancy, irrespective of site, has been reported to be 1-4%. Degeneration in leiomyomas have been described in 65% of the cases. Myxoid leiomyoma is characterized by absence of mito tic activity and the presence of myogenic phenotype. The higher end of prevalence for a myxoid degeneration has been reported in upto 50% of all degenerations in uterus, but myxoid leiomyoma has been rarely described in cervix. Cause of a myxoid change in pregnancy is unknown.
Myxoid, Leiomyoma, Cervix, Pregnancy
Case Report
A 28-year-old, 8 months primigravida, from a remote village presented to Gynaecology Out patients Department with on and off pinkish discharge which had been seen since 20 days . P/A examination and height of uterus corresponded to gestational age. P/S examination revealed a 5x4cm growth which was attached to cervix, which covered the cervical opening. P/V examination showed that fornices were clear. Sonography of the foetus corresponded with gestational age. The mass which was attached to cervix was hypoechoic with well circumscribed margins. An MRI was not advised because of the pregnancy. Routine investigations were normal. There was no history of any medication. Her previous sonography was done at 3 months of gestation by a private practitioner, but the mass was not identified at that time. We do not know exactly, as to whether there was a small leiomyoma before pregnancy or whether it had developed during the pregnancy. The patient underwent a myomectomy, to avoid any risk of complications.
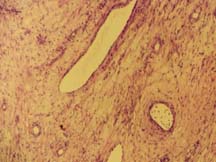
Gross specimen showed a sessile mass with a broad attachment which measured 5.5x4x3cm, which was attached to the anterior lip of cervix, which covered the entire cervical opening. Externally, the mass was grey white, nodular, firm in consistency [Table/Fig-1]. Cut-section was white with a gelatinous appearance and minute cystic areas [Table/Fig-2].
Shows nodular appearance of leiomyoma with part of cervix.(4320x2340 pixels)

Cut section shows white and gelatinous appearance (4320x2340 pixels)

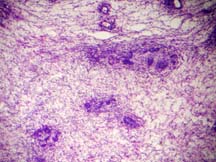
Microscopically, the tumour showed proliferation of smooth muscle cells without atypia or mitotic activity. Intervening stroma showed abundant myxoid change and oedema. Plenty of small and medium sized vessels were seen. Background showed plenty of mixed inflammatory cells [Table/Fig-3 and 4]. A differential diagnosis of an aggressive angiomyxoma was considered because of extensive myxoid change and presence of plenty of blood vessels. On extensive sectioning, only a rare section which was taken from periphery of tumour revealed features which resembled those of a leiomyoma.
shows spindle cells in a myxoid background(H & E,4000X3000 pixels)
Shows thin walled blood vessel, inflammatory cells, spindle cells in a myxoid background. (H &E,4000X3000 pixels
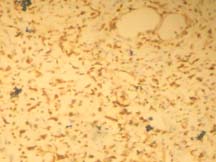
On immunohistochemistry, the tumour was found to be positive for vimentin and negative for CD34 [Table/Fig-5]. Both oestrogen and progesterone receptor studies showed negativity for the nuclei. Based on gross, microscopy and immunohistochemistry, a diagnosis of a myxoid leiomyoma was made.
sshows cells positive for vimentin.(4000x3000 pixels)
Discussion
Myxoid leiomyoma was first described in 1979, by Tavassoli and Norris, who reported 10 cases of leiomyoma with myxoid changes, seven of whom were pregnant [1]. Fibroids prevalence during pregnancy, irrespective of site, has been reported to be 1-4% [2]. Incidence of myxoid leiomyoma in cervix is unknown. Rarely, has a case been reported. A clinical diagnosis is not possible. Cervical fibroids are similar to those fibroids which are found in other parts of the body of the uterus. Like uterine myomas, cervical leiomyomas can undergo various types of degenerations like hyaline, myxoid and cystic degenerations. Cervical fibroids can lead to urinary retention, urinary frequency, constipation, menstrual abnormalities, dyspareunia and sometimes, postcoital bleeding. Cervical fibroids generally don’t affect a womans’ abilty in becoming pregnant, though cervical fibroids are rarely seen in pregnancy [3]. During pregnancies, they may cause miscarriages. Cases have been reported, where cervical fibroids mimicked ovarian tumours [4]. Cytogenetically, they are monoclonal tumours and 40-50% of them show karyotypically detectable chromosomal abnormalities. Specific mutations of the MED12 protein have been noted in 70% of fibroids [5]. Fibroid growth is strongly dependent on oestrogen and progesterone. It has been believed that oestrogen and progesterone produce mitogenic effects on leiomyoma cells and that they also act by influencing large number of growth factors, cytokines and apoptotic factors, as well as, other hormones [6]. Growth hormone and prolactin are thought to promote growth of uterine leiomyomas, but they require further investigations [7]. Diagnosis can be established in most of the cases with the use of imaging modalities. On ultrasound, leiomyomas are hypoechoic. On MRI images, myxoid component shows high signal intensity on the T2 weighted images,low signal intensity on the T1 weighted images and no enhancement on the gadolium enhanced images [8]. But, imaging modalities cannot distinguish between myxoid leiomyomas and myxoid leiomyosarcomas. Myxoid leiomyosarcomas show nuclear enlargement and pleomorphism, along with infiltrative growth. In myxoid leiomyomas, there is a myxoid degeneration of collagen, which tends to leave large thick-walled vessels in the stroma, a feature which is not found in myxoid leiomyosarcomas.
It is unclear as to whether any specific hormone change which occurred in pregnancy led to a myxoid change in leiomyomas, but it has been emphasized that a myxoid change is closely associated with the age of occurrence.
Leiomyomas whichare considered to occur infrequently in pregnancy, should now be considered as one of the common differential diagnosis of any mass which presents in a pregnant female. Secondly , the closest differential diagnosis of an aggressive angiomyxoma, angiomyofibroblastoma, myxoid leiomyosarcoma should always be ruled out. A diagnosis can be made only by doing histopathological studies.
[1]. Tavassoli FA, Norris HJ, Smooth muscle tumors of the vulvaObstet Gynecol 79 53:213-17. [Google Scholar]
[2]. Bromberg JV, Goldberg J, Rychlak K, Weinstein L. The effects of uterine fibroid on pregnancy outcomes. Available at http://orwh.od.nih.gov/health/39-Brombergpdf [Google Scholar]
[3]. Garg R, Two uncommon presentation of cervical fibroidsPeople Journal of Scientific Research 2012 5(2):36-39. [Google Scholar]
[4]. Sharma S, Pathak N, Goraya SPS, Singh A, Mohan P, Large cervical fibroid mimicking an ovarian tumorSri Lanka Journal of Obstretics and Gynaecology 2011 33:26-27. [Google Scholar]
[5]. Makinen N, Mehine M, Tolvanen J, Kaasinen E, Li Y, Lehtonen HJ, Gentile M, Yan J, Med 12, the mediator complex, subunit 12 gene is mutated at high frequency in uterine leiomyomasScience 2011 334:252-5. [Google Scholar]
[6]. 0Yen-Ping HO J, Man WC, Wen Y, Polan ML, Shih-Chu Ho E, Chen B, Transforming growth interacting factor expression in leiomyoma compared with myometriumFertil. Steril 2009 94(3):1078-83. [Google Scholar]
[7]. Vanni R. Uterus: Leiomyoma. Atlas Genet Cytogenet Oncol Haematol. February 2002URL:http://AtlasGeneticsOncology.org/Tumors/leiomyomID5031.html Lynch AM, Morton CC. Uterus: Leiomyoma. Atlas Genet Cytogenet Oncol Haematol. May 2007. URL: http://AtlasGeneticsOncology.org/Tumors/leiomyomID5031.html [Google Scholar]
[8]. Ueda H, Togashi K, Konishi I, Kataoka ML, Koyama T, Fujiwara T, Unusual appearances of uterine leiomyomasMR Imaging findings and their histopathologic findings [Google Scholar]