Calcium Sulfate as Bone Graft Substitute in the Treatment of Osseous Bone Defects, A Prospective Study
Yashavantha Kumar C1, Nalini K B2, Jagdish Menon3, Dilip Kumar Patro4, Banerji B H5
1 Assistant Professor, Department of Orthopaedics, M S R Medical College, Bangalore, India.
2 Assistant Professor, Department of Anaesthesia, M S R Medical College, Bangalore, India.
3 Associate Professor, Department of Orthopaedics, JIPMER, Puducherry, India.
4 Professor and HOD, Department of Orthopaedics, JIPMER, Puducherry, India.
5 Associate Professor, Department of Orthopaedics, M S R Medical College, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Yashavantha Kumar C, No 20, Sri Tiru Nivas, Lotte Golla Halli, RMV II satge, Bngalore-94, India.
Phone: 9663581868, Email: kumyashwanth@gmail.com
Background: Calcium sulfate belongs to synthetic ceramic group of bone graft substitutes having an osteoconductive property. Calcium sulfate is an easily available, economic bone graft substitute. It is a bio-inert material which over a period of weeks get resorbed and fibrovascular tissue takes its place which eventually allows neovascularisation and bone formation within the area. Use of calcium sulfate as a bone graft substitutes avoids the complications and morbidity associated with autograft like infection, second surgery, and finite amount of graft.
Material and Methods: A total of 15 patients with benign bone lesions and chronic osteomyelitis were operated and the osseous defects were filled with calcium sulfate which was comprehensively sterilized. Patients were followed with serial radiographs at six week intervals. Calcium sulfate resorption and new bone formation was studied.
Results: Thirteen cases out of 15 showed calcium sulphate resorption and new bone incorporation. Calcaium sulphate resorption occurred at an average of 14.5 weeks (range,13-18weeks) whereas new bone incorporation occurred at an average of 6months ( range,5-7months). Thirteen patients out of these 15 cases returned to full activities of daily living. One patient had pathological fracture at the osseous defect postoperatively. One patient with GCT of distal end of tibia had recurrence of tumor and had to undergo second surgery.
Conclusion: Although autogenous bone graft is the gold standard for bone grafting, it has limitations like finite amount, additional surgery and donor site morbidity. Calcium sulphate is safe, efficient and easily available bone graft substitute in the treatment of osseous defects. Most common complication encountered was aseptic serous discharge. Functional results were favorable in most of the cases.
Calcium sulfate, Bone graft substitute, Osseous defects
Introduction
Treatment of large osseous bone defects is challenging. Autologous bone grafting is still the “biologic gold standard” against which all other forms are judged. Autograft enhances union by providing osteoconductive, osteoinductive and osteoprogenitor material to the fracture, nonunion and osseous defects. Unfortunately finite amount of graft available from each individual and additional surgery required for bone grafting with donor site morbidity approaching 30%. Non availability of autograft is a major concern in young children [1–4].
Allografts are alternatives to autografts and taken from donors or cadavers, circumventing some of the shortcomings of autografts by eliminating donor-site morbidity and issues of limited supply. However, with use of allografts, the risk of viral disease [HIV, hepatitis B and C] transmission from donor to recipient is not completely removed. Aseptic discharge locally is also a significant complication of allograft. Despite the benefits of autografts and allografts, the limitations of each have necessitated the pursuit of alternatives [5–9].
Using the two basic criteria of a successful graft namely osteoconduction and osteoinduction, investigators have developed several alternatives, some of which are available for clinical use and others of which are still in the developmental stage. Many of these alternatives use a variety of materials, including natural and synthetic polymers, ceramics, and composites, whereas others have incorporated factor- and cell-based strategies that are used either alone or in combination with other materials [5–9].
Calcium sulfate (CaSO4 • ½ H2O), also known as plaster of Paris, has been used for more than a century. Although its external use of calcium sulfates as plaster of Paris dates back to the seventeenth century, there have been few studies using calcium sulfate as a bone graft substitute. Key features of this alloplast material include its biocompatibility, rapid resorption rate, and unique ability to stimulate osteogenesis [10–16]. An additional use for calcium sulfate is its reported use as a binding and stabilizing agent. The matrix is osteoconductive, which leads to new osseous in growth [16,17].
Recently calcium sulfate has been shown to be osteoinductive. This osteoinductive property was related to local bone mineralization which occurs as a result of a reduction of the local pH. This demineralization leads to the release of osteoinductive molecules in the bone matrix stimulating healing process [16,17]. Most of the synthetic bone graft substitutes are not available in India and if available are very costly. We conducted this study in an attempt to prove that calcium sulfate in the form of plaster of Paris was a economical, easily available bone graft substitute with no biological adverse reactions.
Material and Methods
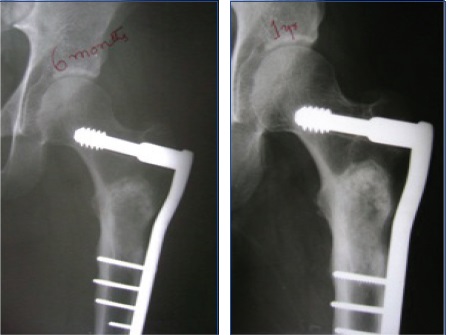
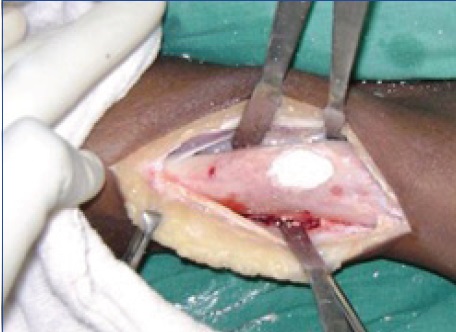
The current study was a prospective study conducted in department of orthopaedics from December 2006 to July 2008. Ethical clearance obtained from institute ethical committee. Fifteen patients with bone defects secondary to benign bone lesions and chronic osteomyelitis were included in the study. The efficacy of healing of bone defects using calcium sulphate was studied. Thorough history and comprehensive clinical examination of the all patients was carried out. All the routine and special investigations were done before biopsy or definitive procedure. Preoperative planning of the approach, type of internal fixation and the amount of graft required was done. Dynamic condylar screw (DCS) was used in three cases of proximal femur fibrous dysplasia after curettage of the lesion. In three cases of chronic osteomyelitis with a defect external fixator was used. All the surgeries were performed by the same surgeon under general /regional anaesthesia. All the lesions were curetted extensively, if required internal fixation was done. Complete haemostasis was achieved and the prepared calcium sulphate graft was applied. Wound was closed in layers meticulously without drain. On first postoperative day the radiographs were taken for assessing curettage and calcium sulphate grafting. Follow up radiographs were taken on sixth week, three months, six months and one year. All the fifteen patients were followed for minimum of one year.
Preparation of Calcium Sulphate Graft.
About 250gm of calcium sulphate powder was collected in a steel container and sterilised by dry heat in a hot air oven. The temperature used was 1210C for fifteen minutes. The calcium sulphate containers stored in a sterile package after the procedure. Half an hour before surgery calcium sulphate was mixed with absolute alcohol so that mixture becomes paste like material. This procedure ensured additional sterilization of the powder. Gradually alcohol evaporates and the calcium sulphate becomes a dry powder over 30-45 minutes. When the calcium sulphate becomes dry one gram ceftriaxone powder was added and mixed thoroughly. Finally distilled water was added to make powder into thick paste which was incorporated into the osseous defects.
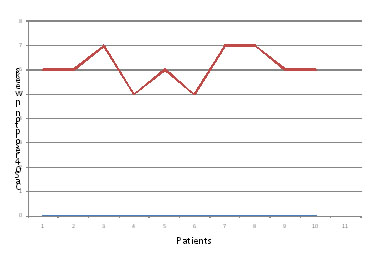
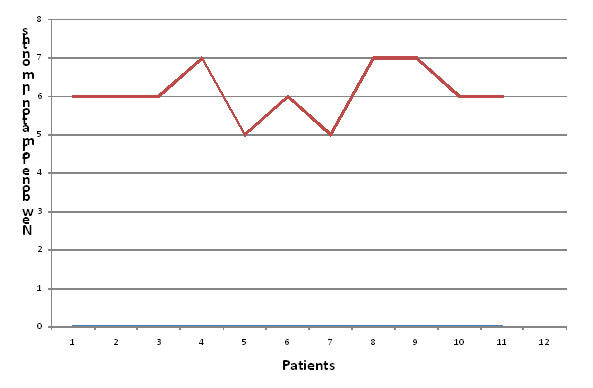
Post-operatively injection of ceftriaxone was given for three days in clean cases. Patients with chronic osteomyelitis were given antibiotics according to culture and sensitivity report. Patients were followed at six weeks, 3 months, 6 months and at one year. During follow up radiological assessment of calcium sulfate resorption and new bone formation was done by Irwin’ criteria, [18]. Using Irwin’s criteria as shown below [Table/Fig-1,2,3,4,5,6,7,8,9,10and11].
Fibrous dysplasia Proximal Femur

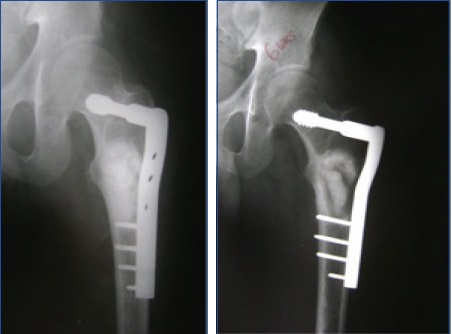
Radiograph at six weeks showing calcium sulphate resorption
Radiograph at three month showing new bone formation

At 6 months new bone consolidating
Radiograph at 18 months of follow up.


After Calcium sulfate grafting
| Stage | Graft margin |
|---|
| I | Obvious |
| II | Hazy |
| III | Obvious incorporation |
| Stage | Graft margin |
|---|
| Fibrous dysplasia | 7 |
| Subacute osteomyelitis | 2 |
| Chronic Osteomyelitis | 2 |
| Aneurismal bone cyst | 1 |
| Giant cell tumor | 1 |
| Intraosseous cyst | 1 |
| Nonossifying fibroma | 1 |
Results
Fifteen cases involved in the study had osseous defects ranging from 13cm3 to as large as 138cm3 fifteen patients among the fifteen cases were of benign bone lesions. Thirteen cases out of these thirteen showed calcium sulphate resorption and new bone incorporation. Calcium sulphate resorption occurred at an average of 14.5 weeks (range,13-18weeks) whereas new bone incorporation occurred at an average of 6 months (range, 5-7 months). Thirteen patients out of these 15 cases returned to full activities of daily living.
One patient had pathological fracture at the osseous defect Post-operatively. One patient with GCT of distal end of tibia had recurrence of tumor and had to undergo second surgery.
Aseptic discharge was a common complication seen in 8 cases, but it was self limiting and responded to simple saline dressing. There was no incidence of hypercalcemia, soft tissue calcification or persistence of infection.
Discussion
It is well recognised that use of synthetic bone graft substitutes overcome many limitations of more commonly used autogenous bone graft [1–4]. There has been a explosion of commercial products for the orthopaedic surgeon to choose from. Calcium sulphate, calcium phosphate, bioactive glass, biodegradable polymers and recombinant human BMPs are all offered as solutions to the problem of bone healing. Calcium sulphate was used alone without bone graft or other additives [10–17]. Currently calcium sulphate is available as medical grade calcium sulphate. We use calcium sulfate powder for casting without crystallization.
Our study involved 15 patients out of which four were females and 11 were males with mean age of 23.61 years. Bone lesions involved in study were both structural and non-structural (cavitory) osseous defects. Twelve cases out of 15 were in lower limbs where as other three were in humerus and clavicle. Calcium sulphate does not provide structural support and hence some type of fixation required along with calcium sulphate. For proximal femoral lesions dynamic condylar screw and proximal femoral nailing was used. External fixator was used in three other cases whereas other cases were managed with external splint.
All the cases were followed regularly with serial radiographs, calcium sulphate resorption and bone incorporation was assessed using Irwin’s criteria. Out of fifteen patients 13 patients with showed calcium sulphate resorption and new bone incorporation. Calcium sulphate resorption occurred at an average of 14.5 weeks and bone incorporation occurred at an average of six months. There is a significant delay between calcium sulfate resorption and bone consolidation because after calcium sulphate is resorbed it is replaced by fibrous tissue over which bone consolidation occurs. Fibrous tissue unlike calcium sulphate and new bone is radiolucent. Two patients with nonunion calcium sulphate extruded because of inadequate soft tissue cover. These patients underwent second surgery in the form of Ilizarov fixation. There were no significant complications like hypercalcemia and persistence of infection. However aseptic serous discharge was seen in 8 patients which was self-limiting. Aseptic discharge lasted for 3-4 weeks.
We recommend use of sterilised calcium sulphate in the treatment of osseous defects following curettage of benign lesions , osteomyelitis and trauma. It can be used to fill large osseous defects and also can be used as graft expander with autograft. It is also recommended in the treatment of nonunions where adequate soft tissue coverage is possible. Use of calcium sulphate is not associated with major complications but overcomes limitations of an autograft.
Limitation of our study was a small sample size.
Conclusion
Although autogenous bone graft is the biological gold standard for bone grafting, it has limitations like finite amount, additional surgery and donor site morbidity. Calcium sulphate is safe, efficient and easily available bone graft substitute in the treatment of osseous defects. Complication encountered was aseptic serous discharge which was self-limiting in most of the cases.
[1]. Banwart JC, Iliac crest bone graft harvest donor site morbidityA statistical evaluation:1055-60.spine 20 [Google Scholar]
[2]. Hill N.M, Donor site morbidity in the iliac crest graftAust N Z J Surg69:726-28. [Google Scholar]
[3]. Fowler BL, Dall BE, Rowe DE, Complications associated with harvesting autogenous iliac boneAm J Orthop 1995 24:895-903. [Google Scholar]
[4]. Younger EM, Chapman MW, Morbidity at bone graft donor siteJ O trhop Trauma 1989 3:192-5. [Google Scholar]
[5]. Jaffery Yao MD, bone grafts and bone graft substitutes, clinics volumeSeptember, pages243-50 [Google Scholar]
[6]. Finkemier CG, bone grafting and bone grafting substitutesJ bone Joint surg Am 2002 84:454-64. [Google Scholar]
[7]. Gazdag A R, Lane J, Mang Glaser D, alternative to autogenous bone graft : efficacy and indicationsJ Am Acad Orthop Surg 1995 3:1-8. [Google Scholar]
[8]. Habal MB: bone graft and bone graft substitutes, philedelphia, pp.6-8 [Google Scholar]
[9]. Grrenwald AS, bone graft substitutes : facts, fictions and applicationsJ Bone Joint Surg (Am)83-A:98-103. [Google Scholar]
[10]. Thomas radiographic and histologic assessment of calcium sulphate in experimental animal models and clinical use as a resorbable bone graft substitute, a bone graft expander and amethod for local antibiotic deliveryJ Bone Joint Surg Am83:8-18. [Google Scholar]
[11]. Kelly C M, The use of surgical grade calcium sulphate as a bone graft substituteClinical Ortho Related Research Jan (382):42-50. [Google Scholar]
[12]. Gitelis , use of calcium sulphate based bone graft substitute for benign bone lesionsOrthopaedics 2001 4:162-66. [Google Scholar]
[13]. Mirzayan R, The use of calcium sulphate in the treatment of benign bone lesions: a preliminary reportJ bone joint surg83A:355-58. [Google Scholar]
[14]. Peltier L, the use of plaster of paris to fill large defects in boneAm J Surg97:311-15. [Google Scholar]
[15]. Dreesman H, Uber knochenplombierrung, beitr klin chir9:804-10. [Google Scholar]
[16]. Borreli J, treatment of nonunions and osseous defects with bone graft and calcium sulphateClin Ortho Rel Res411:245-54. [Google Scholar]
[17]. Evaniew N, Tan V, Parasu N, Jurriaans E, Finlay K, Deheshi B, Ghert M, Use of a calcium sulfate-calcium phosphate synthetic bone graft composite in the surgical management of primary bone tumoursOrthopedics 2013 Feb 36(2):e216-22.doi: 10.3928/01477447-20130122-25 [Google Scholar]
[18]. Irwin coralline hydroxyl appetite as the bone graft substitute in orthopaedic oncologyAm J orthop30:544-50. [Google Scholar]