Induction of labour implies artificial initiation of regular uterine contractions after 28 weeks of gestation, before their spontaneous onset, resulting in progressive effacement and dilatation of cervix, with an aim to secure a vaginal delivery. Labour induction near term is required in 10-20% of women. Labour is induced when risk of continuing pregnancy outweighs the risk of delivery. The indication for induction has been steadily widened in recent years.
The aim of induction of labour is to achieve a vaginal delivery in advance of normal timing of parturition. The methods which are commonly available for the purpose of induction, are non pharmacological and pharmacological use of drugs like oxytocin, and prostaglandins.
Successful outcome of spontaneous or induced labour is the result of a well co-ordinated interplay between the dominant and contracting upper uterine segment, passive and dilating lower uterine segment and also, co-ordinated interplay between myometrial contractility and cervical effacement and dilatation.
Both oxytocin and prostaglandins are used for induction of labour. Induction of labour with oxytocin is unlikely to lead to a vaginal delivery in a reasonable period of time, especia+lly in an unripe cervix.
Induction of labour with prostaglandins offers the advantage of promoting cervical ripening with stimulation of myometrial contractility. Misoprostol (zytotec) a synthetic PGE1 analogue, has the advantage of being inexpensive, easy to store and stable at room temperature.
Material and Methods
Selection of cases: The methods were explained to the pregnant women who underwent medical and obstetric indication of labour and only those who volunteered were finally selected for the study. Prior to interview, informed consents were taken from every respondent. Patients who met the selection criteria were explained about the advantages and disadvantages of the procedures. Among them, those who provided their informed consents were interviewed and recruited in the study.
Selection Criteria: Singleton pregnancies with vertex presentation, gravida (1 to 4), clinically adequate pelvis, Bishop’s score of less than six, pregnancy induced hypertension, pre-eclampsia, antepartum, eclampsia, prolonged pregnancy, oligohydramnios, premature rupture of membranes.
Exclusion criteria: All patients with severe systemic illnesses like uncontrolled diabetes mellitus, pre-eclampsia, cardiac, renal or hepatic disease, intra-uterine deaths and hypersensitivity to misoprostol or prostaglandin analogue. Patients with any contraindication to induction and vaginal delivery, e.g. cephalopelvic disproportion, malpresentation, foetal compromise, no reassuring foetal heart rate pattern, previous scar and ante partum haemorrhage.
Methods of Administration
The patients were randomly assigned to one of the two groups of route of administration.
Group-I: (Vaginal misoprostol) 100 women.
Tablet Misoprostol available as 200 μg, 100μg and 25 μg. One tablet of 25 μg misoprostol was placed in vagina and dose was repeated every four hours for a maximum of four doses.
Group-II: (Oral misoprostol) 100 women.
Two tablets of 25μg misoprostol given orally. The dose was repeated every four hours for a maximum of four doses.
The doses were repeated till effective uterine contractions (more than 3 contractions in 10 minutes), cervical dilatations of 3 centimetres and Bishop’s score of 8 were achieved.
Patients were monitored for uterine contractions and foetal heart rate during this period.
Per vaginal examination was done at four hours and eight hours following drug administration or earlier, if the patient complained of draining per vagina or labour pains.
Membranes were ruptured when cervix was completely effaced with a cervical dilatation of >/= 3cms.
Oxytocin infusion was started in active phase of labour, in the absence of adequate uterine contractions, 6 hours after the last dose of drug was given.
Maternal pulse rate, blood pressure and foetal heart rate were monitored every 30 minutes from the time of induction.
Process of labour was assessed through partogram by noting the strength and duration of uterine contractions ,descent of presenting part, dilatation and effacement of cervix.
Complications with Induction
Hyperstimulation (more than five contractions in 10 minutes for 2 consecutive 10 minute periods, associated with abnormal foetal heart rate pattern) may occur with both oxytocin or prostaglandin administration. It can be reversed by stopping any infusion or subcutaneous administration of tocolyticsterbutaline 0.25mg or of that which was diluted in 5ml of normal saline intravenously over 5 minutes.
Tachysystole (defined as more than 5 uterine contractions per 10 minutes for two consecutive 10 minute periods, without foetal heart rate abnormalities)
Hypersystole (defined as one uterine contraction with a duration of >90 seconds.
Maternal Condition during Induction of Labour
The need for monitoring, largely, depends on the indication for induction.
Maternal pulse rate, blood pressure, the duration and frequency of uterine contractions are monitored.
Prostaglandins may cause a rise in temperature due to direct effect on thermo regulatory centres in the brain. Diarrohoea and nausea may occur, reassurance and support are required. Induction was considered as a failure if the Bishop’s score was < 8 after a maximum of 4 doses and after 12 hours of induction.
Results
[Table/Fig-1] shows the gravida-wise distribution of pregnant women. The number of patients who were primigravida was 62 in vaginal group and it was 64 in oral group. The number of patients who were multipara was 38 in vaginal group and it was 36 in oral group. In the study group, gravida of patients ranged from 1 – 4. Prolonged pregnancies and pregnancy induced hypertension were the major indications for induction of labour [Table/Fig-2].
Gravida wise distribution of pregnant women
| Gravida | Group -1 (vaginal) | Group -2(oral) |
|---|
| Primi | 62 | 64 |
| G2 | 34 | 36 |
| G3 | 4 | 0 |
Indications for induction
| Indication | Group -1 (vaginal) | Group -2 (oral) |
|---|
| Prolonged pregnancy | 44 | 66 |
| Pregnancy Induced hypertension | 26 | 16 |
| Premature rupture of membranes | 11 | 14 |
| Oligohydramnios | 2 | 0 |
| Preeclampsia | 13 | 4 |
| Ante partumeclampsia | 4 | 0 |
[Table/Fig-3] shows the number of patients who delivered by vaginal and oral routes and the number of doses required for induction. As depicted in [Table/Fig-4], the p-value was 0.111 and there was no significant difference between number of patients who delivered vaginally and number of doses required.
Comparison of number of patients delivered vaginally and number of doses required
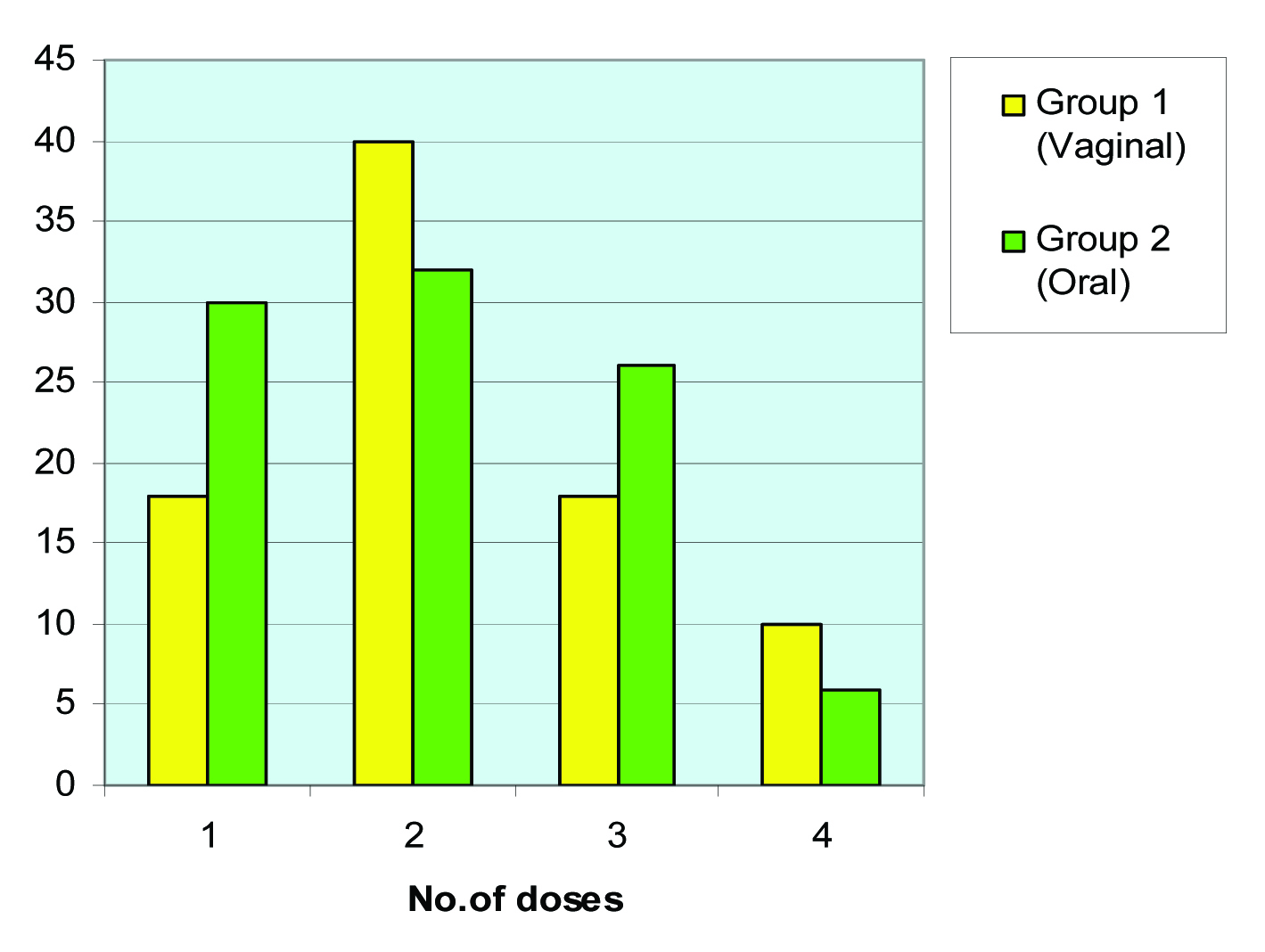
Comparison of number of patients delivered vaginally & number of doses required
| Number of doses | Group 1 (Vaginal) | Group 2 (Oral) |
|---|
| 1 | 18 | 30 |
| 2 | 40 | 32 |
| 3 | 18 | 26 |
| 4 | 10 | 6 |
| Chi-square | 5.999730107 | |
| p-value | 0.1116233567 N.S. | |
Major indication for both the groups was foetal distress, as shown in [Table/Fig-5].
Indications for caesarean section in both groups
| Indication | Group 1 (Vaginal) | Group 2 (Oral) |
|---|
| Fetaldistress | 8 | 3 |
| Failedinduction | 6 | 2 |
| Failed Progress | 0 | 1 |
[Table/Fig-6] shows that in group 1, 24 out of 74 had low Apgar scores (6-8) and that 20 out of 78 had meconium stained liquor . In group-2, 14 out of 86 had low Apgar scores (6-8) and 14 out of 86 had meconium stained liquor. Hyperstimulation was seen in one case in group 1; none was seen in group 2. Incidence of nausea and hyperpyrexia were more in group 2. Neonatal mortality was nil in both the groups.
Complications in both the groups
| Complications | Group -1 | Group-2 |
|---|
| FETAL | 0 | 0 |
| Low APGAR scores | 24 | 14 |
| Meconium aspiration | 20 | 14 |
| N eonatal mortality | 0 | 0 |
| MATERNAL | 0 | 0 |
| Hyperstimulation | 1 | 0 |
| Hyperpyrexia | 0 | 3 |
| NAUSEA | 0 | 3 |
| DIARRHOEA | 0 | 0 |
Discussion
Misoprostol has been approved for the treatment of peptic ulcers. Initial studies confirmed that misoprostol’s utero tonic abilities and intra vaginal application were successful and that it was used to terminate first and second pregnancies. The first investigations using mispprostol in cervical ripening and cervical induction were done in South America. Subsequent studies showed favourable comparison of intravaginal misoprostol with other commonly used induction agents, including prostaglandins and oxytocin [3].
In the literature, the interval of administration of misoprostol has been reported to range from every 3 to 6 hours. However, due to the possible risk of tachysystole, many studies had centred use of 4-6 hours interval in their protocols. This study followed the same protocol. Ngai et al., [4] investigated the effectiveness of oral misoprostol
as a cervical priming agent for patients presenting with pre-labour rupture of membranes at term and suggested that oral misoprostol was an effective agent for this group of patients. Similar results were reported by Sanchez-Ramos et al., [3] and Shetty et al., [5].
Induction to Delivery Interval
Oral group had a shorter induction to delivery interval of 12.92 hours as compared to 14.04 hours in vaginal group. But, there was no significant difference between the two. The results of the present study done on oral misprostol were comparable with those of the following studies.
Induction delivery interval
Ratna Khatri et al., [6] (2007) 15.5 hrs
Khadija et al., [7] (2004) 09.81hrs
N Sultan et al., [8] (2003) 08.3 hrs
Rozinarasheed et al., [9] (2002) 20.64hrs
Chandersheikher et al., [10] (2009) 15.05hrs
Present study 12.92 hrs
In the present study, induction delivery interval was 12.92 hrs, which almost consistent with the findings of Khadija et al., [7], Ratnakhatri et al.,[6], Chandersheikher et al., [10]. The results of the present study done on vaginal misprostal were comparable to those of the following studies. In the present study, the induction delivery interval in vaginal group was 14.042 hours, which was almost consistent with the findings of Rozina Rasheed et al., [9] and Ratnakhatri et al., [6]. In the present study, oxytocin augmentation required in group-I was 10% and that which was required in group-II was 12%. These results were consistent with those of Shetty et al., [5], Chandersheikher et al., [10] where 56% patients required oxytocin augmentation in oral group.
Vaginal Deliveries
Induction delivery interval
Ratna Khatri et al., [6] (2007) 15.03 hrs
Khadija et al., [7] (2004) 09.09 hrs
N Sultan et al., [8] (2003) 06.61 hrs
Rozinarasheed et al., [9] (2002) 13.56hrs
Chandersheikher et al., [10] (2009) 10.35hrs
Present study 14.042hrs
The success of vaginal deliveries in oral group was 94% as compared to 86% in vaginal group. Failure rate in oral group was 6% as compared to 14% in vaginal group. The above results were consistent with those of Ratna Katri et al., [6], who reported success rate of 86% in oral group and that of 70% in vaginal group. Failure rate was 14% in oral group and it was 30% in vaginal group.
The above results were also consistent with those of N Sultana et al., [8], where success rate in oral group was 70% and that in vaginal group was 66%. Failure rate was 30% in oral group and it was 34% in vaginal group. The above results were also consistent with findings of Wing et al., [11], where success of vaginal deliveries was more in oral group.
A study was conducted by Chander Sheiker, Natasha Suri, Uma Kohli [10] of SMGS Hospital, Jammu, India, where success rate in oral group was 56.6% and in vaginal group it was 86.6%, where failure rate in oral group was 26.6% and in vaginal group, it was 13.3%. Even the study of Chandrasheikher et al., [10] and many other studies showed that success of vaginal deliveries was more in oral group than in vaginal group. The present study showed that success of vaginal deliveries was more in oral group (94%).
Operative Delivery Rate
In this study, caesarean rate in oral group was 6% and in vaginal group, it was 14%. These results were consistent with those of Ratnakhatri et al., [6], where operative delivery rate was 14% and it was 30% in vaginal group.
Major indication for operative delivery rates in both the groups was foetal distress. In the present study, in 57% cases in vaginal group and in 50% cases in oral group, the indication for operative delivery rates was foetal distress. The major causes of foetal distress in both the groups were preeclampsia and prolonged pregnancy, probably caused by placental insufficiency and umblical cord compression, caused by oligohydramnios.
These results were also consistent with those of N Sultana et al., [8], where operative delivery rate was 30% in oral group and it was 34% in vaginal group.
The incidence of instrumental delivery was same in both the groups in this study.
Failed Induction
In this study, failed induction rate was more in vaginal group, which had a 6% rate as compared to oral group, which had a rate of 2%. These results were consistent with those of N Sultana et al., [8], where failed Induction rate was 8% in vaginal group and it was 6% in oral group.
Maternal Complications
The rate of hyperstimulation in vaginal group was only 1%, where caesarean section was done immediately and it was nil in oral group. Hyperstimulation in vaginal group was caused by greater bioavailability.
These results were consistent with those of N. Sultana et al., [8], where they reported a 4% rate of hyperstimulation in vaginal group. These results were also consistent with those of Khadija et al., [7], where they reported a 1% rate of hyperstimulation in vaginal group.
Gastrointestinal side-effects were reported more in oral group
and incidence of hyperpyrexia was also more in oral group.
Neonatal Outcome
24 cases out of 74 in vaginal group and 14 cases out of 86 in oral group had low 5 minutes Apgar scores of 6-8. None reported neonatal mortality in both the groups.
The major cause of low Apgar scores at 5 minutes was prolonged pregnancies (39%) in both the groups. This was caused by umbilical cord compression secondary to oligohydramnios (Leveno et al., 1984) [12] and placental insufficency caused by placental senescence (Silver et al., 1988) [13].
There were two admissions to NICU, where they were discharged after two days after observation.
Overall, neonatal outcomes in both the groups were good.
Ratnakhatri et al., [6] reported 100% in oral group and 96% in vaginal group, where 5 minutes Apgar scores were greater than 6.
In this study, incidence of meconium stained liquor was more in vaginal group (20 out of 78) as compared to that in oral group (14 out of 86) but there was no significant difference. The major cause in both the groups was a prolonged pregnancy.
Regarding the type of liquor, orally induced misoprostol group had more patients with clear liquor (44/50 i.e. 88%) as compared to the vaginally induced group, which had only 20/50 i.e. 40% women with clear liquor, which was statistically significant [6]. In all the studies, vaginal misoprostol had more number of MSL. According to Uludag [14] this was 16.7%: 5.9% [15]. Increased meconium stained liquor in the vaginally induced group could be explained by the fact that vaginally absorbed misoprostol bypasses the hepatic and gastrointestinal metabolism and so, it achieves a higher concentration in plasma, increased by the cumulative effect, following repeated administration of the drug.
Conclusion
The acceptability of the different routes of administration of misoprostol by women was evaluated. Patients preferred the oral route of administration for induction of labour. Further research with regards to labour induction should include the balance between effectiveness and safety. Moreover, there is a need to follow-up mothers and neonates over a long term, to detect rare but serious side-effects of misoprostol. However, based on this study, it does appear that oral misoprostol may be an effective induction agent that is well tolerated orally, because of its ease of usage.