Introduction: Ankylosing spondylitis (AS) is an inflammatory rheumatic disease characterized by spine and sacroiliac joint involvement that mainly affects young male subjects. Bone Mineral Density (BMD) loss occurs in AS disease course. Bone loss in AS appears to be multifactorial and perhaps involves different mechanisms at different stages of disease. The disease typically affects young males and is associated with progressive functional impairment, increased work disability and decreased quality of life. Osteoporosis is frequent in AS and there is a close association of bone mineral density, bone metabolism and inflammatory activity. Osteoporosis is frequently associated with AS and BMD decreased predominantly in patients with active disease.
Aims & Objectives: The aim of the present study was to study bone mineral density in cases of Ankylosing Spondylitis (AS) in comparison to age and sex matched controls.
Material and Methods: The present study was conducted on 100 established cases of AS based on modified New York criteria and 150 controls healthy, age, race, socio-economic matched controls patients. The results were statistically analyzed.
Results: Hundred cases of AS were subjected to undergo BMD by Dual Energy X-ray Absorption (DEXA) scan of different age groups in cases 35.19± 8.23(min age 23- max age 67years) and controls 33.27±5.22(min age 22years - max age 44years) with height observed in cases is 169.67±6-87 and controls 170.99±7.16 with weight varied in cases 65.63±10.27 and controls 70.14±10.67.
Conclusion: Osteoporosis is a significant complication in ankylosing spondylitis and needs to be monitored and managed at the earliest. Significant osteoporosis can occur even in early disease. Osteoporosis of spine is much more prevalent than femur.BMD spine is still the most important site to define osteoporosis in ankylosing spondylitis. Rise in BMD in LS spine with duration, is not exclusive for subjects with radiologically evident syndesmophytes. Statistically, presence of syndesmophytes did not affect estimation of osteoporosis of spine.
Introduction
Ankylosing spondylitis (AS) is an inflammatory rheumatic disease characterized by spine and sacroiliac joint involvement that mainly affects young male subjects. The name is derived from the Greek roots angkylos–meaning ‘bent’ (the word ankylosis means joint stiffening or fusion)–and spondylos–meaning spinal vertebra). Syndesmophytes, which are due to new bone formation, are considered to be a hallmark of the disease.
Physical examination of patients with ankylosing spondylitis may have one or more of the following abnormal findings on physical examination, reduced range of motion in the low back, changes in the spinal curvature. In a normal spine there are four areas of spinal curves: cervical, thoracic, lumbar, and sacral. Increased curvature in the thoracic area and decreased curvature in the cervical and lumbar areas are characteristic of ankylosing spondylitis, decreased ability to expand the chest during deep breathing, abnormal hip flexion (bending), pain and stiffness of joints other than the hips and low back.
Ankylosing spondylitis can affect daily life in various ways. Dressing, reaching, rising from a chair, getting up from the floor, standing, climbing steps, looking to the side or over the shoulder, exercising, and doing household or work related tasks can all be made more difficult by active arthritis or by the limited joint and spinal motion that can occur with ankylosing spondylitis. These limitations affect the family as well as the patient, and many patients with ankylosing spondylitis require support and assistance from family and friends. Osteoporosis is a common complication of ankylosing spondylitis with incidence between 18.7% and 62%. The prevalence of osteoporosis is greater in males, and increases with increasing patient age and disease duration [1].
Spinal osteoporosis is frequently observed, especially in patients with severe ankylosing spondylitis of long duration. Osteoporosis may contribute to spinal fractures and progressive spinal deformity. It increases the mortality and morbidity related to AS. Patients with AS develop characteristic changes in the sacroiliac joints that become visible on x-ray images. These changes take time to develop and in some patients may not be apparent until years after symptoms of ankylosing spondylitis begin. X-ray may be used to diagnose ankylosing spondylitis in someone whose symptoms, history, and physical exam suggest AS. CT & MRI are of not much value & not routinely used.
About 50% of spinal bone mass has to be lost before demineralization becomes apparent on standard radiographs. Therefore radiography is relatively insensitive in assessing skeletal changes. Dual Energy X-ray Absorption (DEXA) is the most reliable technique for measurement of bone mineral density (BMD) [2].
It is two to three times more common in men than women. Ankylosing spondylitis usually begins with back pain and stiffness in adolescence and early presentations may antedate back symptoms in some patients [3–7]. It is very rare for ankylosing spondylitis to first begin after 45 years of age, but disease is diagnosed at an older age in many patients, in part because symptoms over the years have been minimal [8–11].
Symptoms commonly begin in late adolescence and early adulthood [12–13]. With an estimated prevalence of 0.9% in northern European white populations [14]. AS is a significant health burden to the community.
The diagnosis of ankylosing spondylitis is clinical, but the classic features suggestive of chronic inflammatory back pain—insidious onset before 45 years of age, worsening with inactivity, and improvement with physical exercise are on their own not very specific [15]. It has been established for several years that Bone Mineral Density (BMD) loss occurs early in the ankylosing spondylitis disease course. However, the pathogenesis of osteoporosis remains controversial. Bone loss in Ankylosing spondylitis appears to be multifactorial and perhaps involves different mechanisms at different stages of disease. In the current literature there are several studies that examined bone mass in ankylosing spondylitis.
Bone is a target in many inflammatory rheumatoid diseases, such as ankylosing spondylitis and Rheumatoid Arthritis (RA). The generalized effect of inflammation on bone may result in a decreased quality of bone and is associated with an increased risk of fractures and deformities, in ankylosing spondylitis while rheumatoid arthritis is characterized by periarticular osteopenia, systemic osteoporosis and bone erosions.
Material and Methods
Hundred cases of AS and 150 controls healthy, age, race, socio-economic matched controls patients were taken from a tertiary care hospital. In this established cases of AS based on modified New York criteria were taken (proven cases). Patients with seronegative spondyloarthropathies other than AS, secondary cases of osteoporosis, on medication known to affect calcium metabolism especially steroids and disease modifying agents were excluded from our study. All the patients and the control groups were soldiers with relatively active life style.BMD was measured from hip and spine by DXA (Hologic QDR 4500W, Hologic, Bedford, MA), which has a mean precision error of 1% for spine and hip The results were recorded as g/cm2, Z score and T score. T scores>-1 were classified as normal. <-1 and >-2.5 were classified as ON and < -2.5 were classified as OP according to WHO classification. The ethical committee clearance and an informed consent of the subjects were taken.
Statistical Analysis
Data was analysed by using EPi info software. Standard error of difference between means, linear regression, stratified Odd’s ratio and Chi-square for linear trend were used to study mean BMD and study factors influencing osteoporosis.
Results
Hundred cases of AS were subjected to undergo BMD by DEXA scan of different age groups in cases 35.19± 8.23 (min age 23- max age 67 years) and controls 33.27±5.22 (minimum age 22 years - maximum age 44 years) with height observed in cases is 169.67±6-87 and controls 170.99±7.16 with weight varied in cases 65.63±10.27 and controls 70.14±10.67.
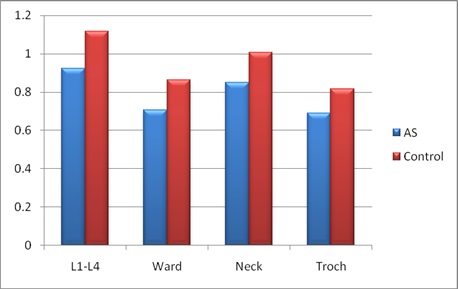
It was observed that there was significant reduction of bone mineral density at all sites with maximum affected site L1-L4 in both cases and control groups as depicted in graph [Table/Fig-1,2].
Significant reduction of BMD at all sites in AS subjects
| Average BMD (g/sq cm) | AS (n=100) | Control (n=150) | p-value |
|---|
| L1- L4 | 0.9241 ± 0.1665 | 1.1172 ± 0.1415 | 0.00001 |
| Femur neck | 0.8491 ± 0.1185 | 1.0064 ± 0.1138 | 0.00001 |
| Femur trochanter | 0.6910 ± 0.1109 | 0.8154 ± 0.1085 | 0.00001 |
| Ward’s triangle | 0.7065 ± 0.1782 | 0.8640 ± 0.1389 | 0.00001 |
| E (20%) | 10.7 | 3.68 | 3.68 |
Significant reduction of BMD at all sites in AS subjects
This table shows that the prevalence of osteoporosis in patients with AS is seen more in cases with maximum affected site is spine L1-L4 in 22% of cases & 2.66% in controls with least affected site being Femur trochanter in 4% cases & 0.66% in controls as shown in [Table/Fig-3].
Prevalence of Osteoporosis
| Site | Cases (n= 100) T score <-2.5 | Controls (n=150) T score<-2.5 | OR | Chi-square | p-value |
|---|
| L1- L4 | 22 (22%) | 4 (2.66%) | | 40.67 | 0.00001 |
| Femur neck | 9 (9%) | 0 | Undefined | 19.54 | Fisher exact 0.00001 |
| Femur trochanter | 4 (4%) | 1(0.66%) | | 5.38 | Fisher exact 0.00001 |
| Ward’s triangle | 13 (13%) | 3 (2%) | | 21.11 | 0.00001 |
| Osteoporosis (anysite) | 31(31%) | 4 (2.66%) | | | |
It was observed that there was no significant alteration in BMD with duration of the disease. Low BMD was observed in the initial stage of the disease as depicted in [Table/Fig-4].
Factors affecting osteoporosis in cases of ankylosing Spondylitis
| Duration | Osteoporosis | Osteopenia | Total with Low BMD |
|---|
| < 2 yrs | 1 (14.3%) | 6 (85.7%) | 7 |
| 2-5 yrs | 9 (42.8%) | 12 (57.2%) | 21 |
| 5-10 yrs | 14 (42.4%) | 19 (57.6%) | 33 |
| >10 yrs | 2 (15.4%) | 11 (84.6%) | 13 |
| Total | 74 | 26 | 74 |
Discussion
A comparative study on 100 cases of ankylosing spondylitis and 150 healthy, age, race, socio-economic matched controls was carried out.
Low bone mass at spine and femur has been well documented in AS. However, there has been wide variation in reported prevalence of OP ranging from 18.7% and 62% [1]. We recorded significant reduction in BMD of AS subjects at lumbar spine, neck femur, greater trochanter and ward’s triangle as compared to controls.
In AS patients the mean BMD and the corresponding T scores were significantly reduced in both lumbar spine as well as femoral neck as compared with controls (all p < 0.05; [Table/Fig-2]. Vertebral fractures were observed in only 1 out of 100 patients (1%).
In our study it was observed that 27% of patients with ankylosing spondylitis had osteoporosis, 47% had osteopenia, normal values were seen in 26% of the cases, where as in control group 2.66% had osteoporosis, 29.33% had osteopenia and normal values in 68% of patients.
22% of cases had osteoporosis at lumbar spine while in the control group it was observed that 2.66% controls had osteoporosis and (normal values were observed in 68%; p=0.03). At the femoral neck we found 9% of the patients had osteoporosis & 50% had osteopenia, while 41% had normal value.
This study showed a reduction of BMD in the lumbar spine as well as the femoral neck in patients with ankylosing spondylitis. In the current literature there are several studies that examined bone mass in ankylosing spondylitis. Taken together, the results were similar, showing that BMD is reduced in ankylosing spondylitis patients in comparison with controls, with some differences according to the stage of the disease.
While in a study by Mulaji et al., found that patients with advanced ankylosing spondylitis had a significantly increased BMD of the lumbar spine both in comparison with the control group and with patients suffering mild disease [16].
In another study, by Donelly et al., found that patients with ankylosing spondylitis had significantly lower femoral neck BMD in proportion to disease severity and duration. They also found that lumbar spine BMD was reduced in early disease, but in patients with advanced ankylosing spondylitis it was increased considerably [17].
In yet another study done by Devogelaer et al., reported a significant decrease in the lumbar spine BMD in mild ankylosing spondylitis, but in advanced ankylosing spondylitis the spine BMD values were similar to the normal controls [18]. Although mild and advanced disease were defined according to various criteria, it seems likely that in advanced ankylosing spondylitis exists a false increase of BMD values, due to syndesmophyte formation and/ or facet joint ankylosis [18,17,19,16,20]. That’s why, the anteroposterior lumbar DEXA (dual energy X-ray absorptiometry) results can be misleading when evaluating the extent of osteoporosis in late stage ankylosing spondylitis [20].
Where as in our study it was observed that there is no significant change in BMD with appearance of syndesmophytes, with insignificant p-value and the syndesmophytes did not alter prevalence of bone mineral density.
In a study contrast to our study by Laura Muntean et al., lumbar spine BMD values of the advanced cases were increased compared with the mild cases, but without statistical significance. Considering the low sensibility of anteroposterior DEXA (dual energy X-ray absorptiometry) in late stage cases, it’s likely for these patients to have lower BMD values and more severe osteoporosis than actually measured.
In a recent study, on a cohort of 103 patients with ankylosing spondylitis, Karberg et al., reported that bone loss is more frequently detected in ankylosing spondylitis patients with syndesmophytes. They concluded that the method of bone density measurement is critical and should be different depending on disease duration. It was found that DEXA (Dual Energy X-ray Absorptiometry) at the femoral neck is the most sensitive method for evaluating osteoporosis in ankylosing spondylitis, even in patients without syndesmophytes [21].
This study also confirmed that the majority of ankylosing spondylitis patients has decreased BMD values at both the lumbar spine and femoral neck. Osteoporosis can be observed in early stages of the disease. The similar frequency of osteoporosis in mild and advanced ankylosing spondylitis suggests that immobility does not have an important role in pathogenesis. Patients with active disease are especially at risk for developing osteoporosis.
The presence of syndesmophytes had no distorting effect on BMD measured by lateral DEXA (Dual Energy X-ray Absorptiometry) or on quantitative computerized tomography (QCT), these methods being more useful than anteroposterior lumbar DEXA (Dual Energy X-ray Absorptiometry ) in late stage ankylosing spondylitis patients [22,23,21].
In another study, in contrast to our study by L Muntean and et al., it was suggested that in late ankylosing spondylitis, the presence of syndesmophytes could falsely elevate the spine BMD values [24,16].
In a latest study, done by Mermerci Baskan B et al., it showed that lumbar spine BMD was significantly lower in AS patients compared with healthy controls when measured by lateral projection DXA but not when measured with AP DXA scan, this study significantly correlates with my study but in this study additional lateral projection DXA scan was also measured [25].
In contrast to the aforementioned studies, we did not find a significant increase in bone mass at the lumbar spine. This might be explained by the heterogeneity of the studied population, since we have included ankylosing spondylitis patients in all stages of the disease, and more than half of the patients did not have syndesmophytes.
[1]. Bessant R, Keat A, How should clinicians manage osteoporosis in ankylosing spondylitis?J Rheumatol 2002 Jul 29(7):1511-9. [Google Scholar]
[2]. Mazess RB, Bone densitometry of the axial skeletonOrthop Clin North Am 1990 21:51-63. [Google Scholar]
[3]. Walsh NC, Crotti TN, Goldring SR, Gravallese EM, Rheumatic diseases: the effects of inflammation on boneImmunol Rev 2005 208:228-51. [Google Scholar]
[4]. Wendling D, Bone loss in ankylosing spondylitis: Can we put the puzzle together?J Rheumatol 2005 32:1184-86. [Google Scholar]
[5]. Sieper J, Braun J, Rudwaleit M, Boonen A, Zink A, Ankylosing spondylitis: an overviewAnn Rheum Dis 2002 61(Suppl 3):iii8-iii18. [Google Scholar]
[6]. Bessant R, Keat A, How should clinicians manage osteoporosis in ankylosing spondylitis?J Rheumatol 2002 29:1511-19. [Google Scholar]
[7]. Toussirot E, Wendling D, Bone mass in ankylosing spondylitisClin Exp Rheumatol 2000 18(Suppl 21):S16-S20. [Google Scholar]
[8]. Khan MA, van der Linden SM, A wider spectrum of spondyloarthropathiesSemin Arthritis Rheum 1990 20:107-13.[PMID: 2251505] [Google Scholar]
[9]. Zeidler H, Mau W, Khan MA, Undifferentiated spondyloarthropathiesRheum Dis Clin North Am 1992 18:187-202.[PMID: 1561402] [Google Scholar]
[10]. Olivieri I, Salvarani C, Cantini F, Ciancio G, Padula A, Ankylosing spondylitis and undifferentiated spondyloarthropathies: a clinical review and description of a disease subset with older age at onsetCurr Opin Rheumatol 2001 13:280-4.[PMID: 11555728] [Google Scholar]
[11]. Mader R, Atypical clinical presentation of ankylosing spondylitisSemin Arthritis Rheum 1999 29:191-6.[PMID: 10622683] [Google Scholar]
[12]. Khan MA, Update on spondyloarthropathiesAnn Intern Med 2002 135:896-907. [Google Scholar]
[13]. Sieper J, Braun J, Rudwaleit M, Boonen A, Zink A, Ankylosing spondylitis: an overviewAnn Rheum Dis 2002 61(suppl 3):iii8-18. [Google Scholar]
[14]. Braun J, Bollow M, Remlinger G, Eggens U, Rudwaleit M, Distler A, Prevalence of spondylarthropathies in HLA-B27 positive and negative blood donorsArthritis Rheum 1998 41:58-67. [Google Scholar]
[15]. Blackburn WD Jr, Alarcon GS, Ball GV, Evaluation of patients with back pain of suspected inflammatory natureAm J Med 1988 85:766-70.[PMID:2973749] [Google Scholar]
[16]. Mulaji AB, Upadhyay SS, Ho EK, Bone mineral density in ankylosing spondylitis. DEXA comparison of control subjects with mild and advanced casesJ Bone Joint Surg Br 1994 76:660-65. [Google Scholar]
[17]. Donnelly S, Doyle DV, Denton A, Rolfe I, Mccloskey EV, Spector TD, Bone mineral density and vertebral compression fracture rates in ankylosing spondylitisAnn Rheum Dis 1994 53:117-21. [Google Scholar]
[18]. Devogelaer JP, Maldague B, Malghemj Nagant De Euxchaisnes C, Appendicular and vertebral bone mass in ankylosing spondylitis. A comparison of plain radiographs with single- and dual-photon absorptiometry and with quantitative computed tomographyArthritis Rheum 1992 35:1062-67. [Google Scholar]
[19]. Bronson WD, Walker SE, Hillman LS, Keisler D, Hoyt T, Allen SH, Bone mineral density and biochemical markers of bone metabolism in ankylosing spondylitisJ Rheumatol 1998 25:929-35. [Google Scholar]
[20]. Capaci K, Hepguler S, Argin M, Bone mineral density in mild and advanced Ankylosing spondylitisYonsei Med J 2003 44:379-84. [Google Scholar]
[21]. Karberg K, Zochling J, Sieper J, Bone loss is detected more frequently in patients with ankylosing spondylitis with syndesmophytesJ Rheumatol 2005 32:1290-98. [Google Scholar]
[22]. Lee YS, Schlotzhauer T, Ott SM, Skeletal status of men with early and late ankylosing spondylitisAm J Med 1997 103:233-41. [Google Scholar]
[23]. Gilgil E, Kaçar C, Tuncer T, Bütün B, The association of syndesmophytes with vertebral bone mineral density in patients with ankylosing spondylitisJ Rheumatol 2005 32:292-94. [Google Scholar]
[24]. Gran JT, Husby G, Clinical, epidemiological, and therapeutic aspects of ankylosing spondylitisCurr Opin Rheumatol 1998 10:292-8. [Google Scholar]
[25]. Mermerci Baskan B, Pekin Dogan Y, Sivas F, Bodur H, Ozoran K, The relation between Osteoporosis and Vitamin D level and disease activity in ankylosing spondylosisRheumatol Int 2010 30:375-81. [Google Scholar]