Aim: Investigate the efficiency of limbal conjunctival autograft in primary and recurrent pterygium. (2) To report the incidence of recurrence after primary and recurrent pterygium surgery using limbal conjunctival autograft.
Material and Methods: It is a prospective study conducted at Department of Ophthalmology, Basaveshwar Teaching and General Hospital, Gulbarga Karnataka, India for a period of 1 year (2007 to 2008) 100 patients were operated of which 6 were recurrent pterygium and the remaining were fleshy pterygium. All patients were in age group 20 to 60 and above.
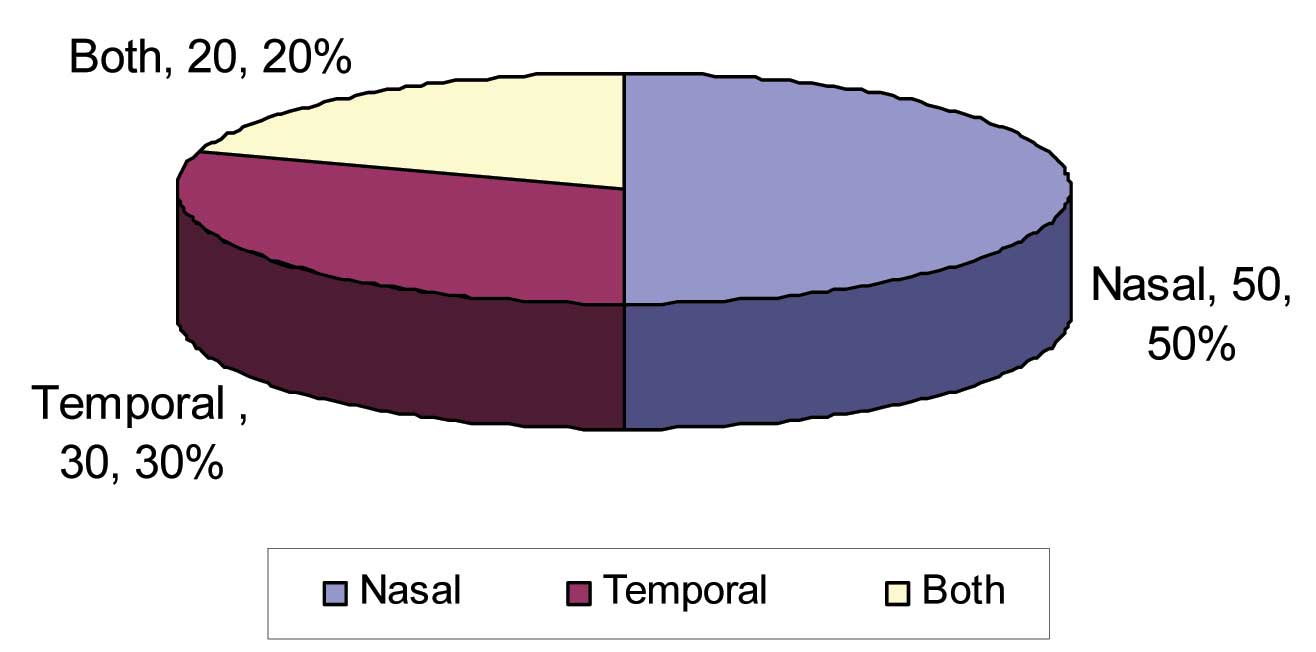
Results: In this study 7% cases were in age group 20 to 30 years, 22% 31 to 40 years, 30% 41 to 50 years, 24% 51 to 60 years and 17% 60 and above. (2) Depending on occupation high incidence is seen in outdoor patients i.e., 80%, indoor 20%. (3) Depending on location, 50% nasal, 30% temporal, bilateral 20%. (4) Laterality – Right eye 52%, left eye 38%, bilateral 10%. (5) Recurrence – More common in younger patients < 40 age 6 patients developed recurrence.
Conclusion: Autogenous conjunctival grafting is a safe, uncomplicated, quick procedure and does not involve loss of tissue and prevents recurrence of pterygium. It also reduces the risk of granuloma formation, scleral thinning and necrosis.
Conjunctival autograft, Primary pterygium, Recurrent pterygium
Introduction
Pterygium was recognised 3000 years ago, it was described by Susrutha way back in 1000 B.C. in India. It was also noted by great physicians of ancient times like Hippocrates, Galen, Celsius etc.
A Pterygium is a wing shaped growth of fibro vascular conjunctiva on to the cornea; its incidence differs across geographical sites. A number of hypotheses have been approved to its aetiology [1]. Now, it is believed that Pterygium is a growth disorder characterised by conjunctivalisation of the cornea due to localized ultraviolet stimulated damage to the limbal stem cells [2]. Destructive Pterygial fibroblasts are also responsible for corneal invasion [3].
Several surgical techniques including bare sclera excision with or without the use of adjuncts like beta irradiation, thio tepa eye drops, intra-operative or post-operative mytomycin-C (MMC) or anti neoplastic agents, amniotic membrane transplantation, conjunctival autograft (CAG) with or without limbal stem cells have been illustrated [4].
Accounted rates of recurrence range from 2% for excision with CAG to 89% for bare sclera excision.
Pterygium surgery is quite common in India, which is situated within the tropics. Hence, our study aimed to determine the outcome of conjunctival autograft in primary and recurrent pterygium.
Gulbarga city has latitude of 17.21° and most of the pterygium cases occur, where the temperature is more than 30°C. People here work in agricultural fields, laborers etc., which are outdoor occupations. They work in dry and dusty places which is the cause of pterygium.
A true Pterygium is a condition found chiefly in the sunny, hot, dusty regions of the world, mostly between the Latitude of 37o North and South of the Equator.
Clinical Materials
This study is a prospective study conducted in the department of Ophthalmology, Basaveshwara Teaching and General Hospital attached to H. K. E. Society’s Mahadevappa Rampure Medical College, Gulbarga during a period of one year (2007-2008) conjunctival autografting was performed in 100 patients. Out of which, 6 were recurrent type and the remaining were fleshy pterygia. All the patients were in the age group of 20 – 60 years and above. Consent was obtained from all patients included and the ethical committee has approved this study.
Methods
Inclusion criteria-there are two pterygium i.e., primary and recurrent.
Exclusion Criteria
Patients with dry eye syndrome.
Patients with collagen vascular diseases.
Follow up less than 24 weeks.
Patients with pseudopterygium.
Patients with co-existent conjunctival diseases like previous alkali burns, moorens ulcer etc., which predispose to formation of pseudopterygium.
All the patients were examined under slit lamp and the type of Pterygium was noted.
Visual acuity, refraction, ocular motility intraocular pressure, potency of lacrimal passages and fundus examination findings were noted.
Routine investigations like blood pressure, syringing was done to all the patients. Patients were put on antibiotic drops before the day of surgery.
Operative Tech (For Conjunctival Flap)
All patients were operated under local anaesthesia, instillation of 4% xylocaine and subjconjunctival injection of 2% xylocaine beneath the pterygium.
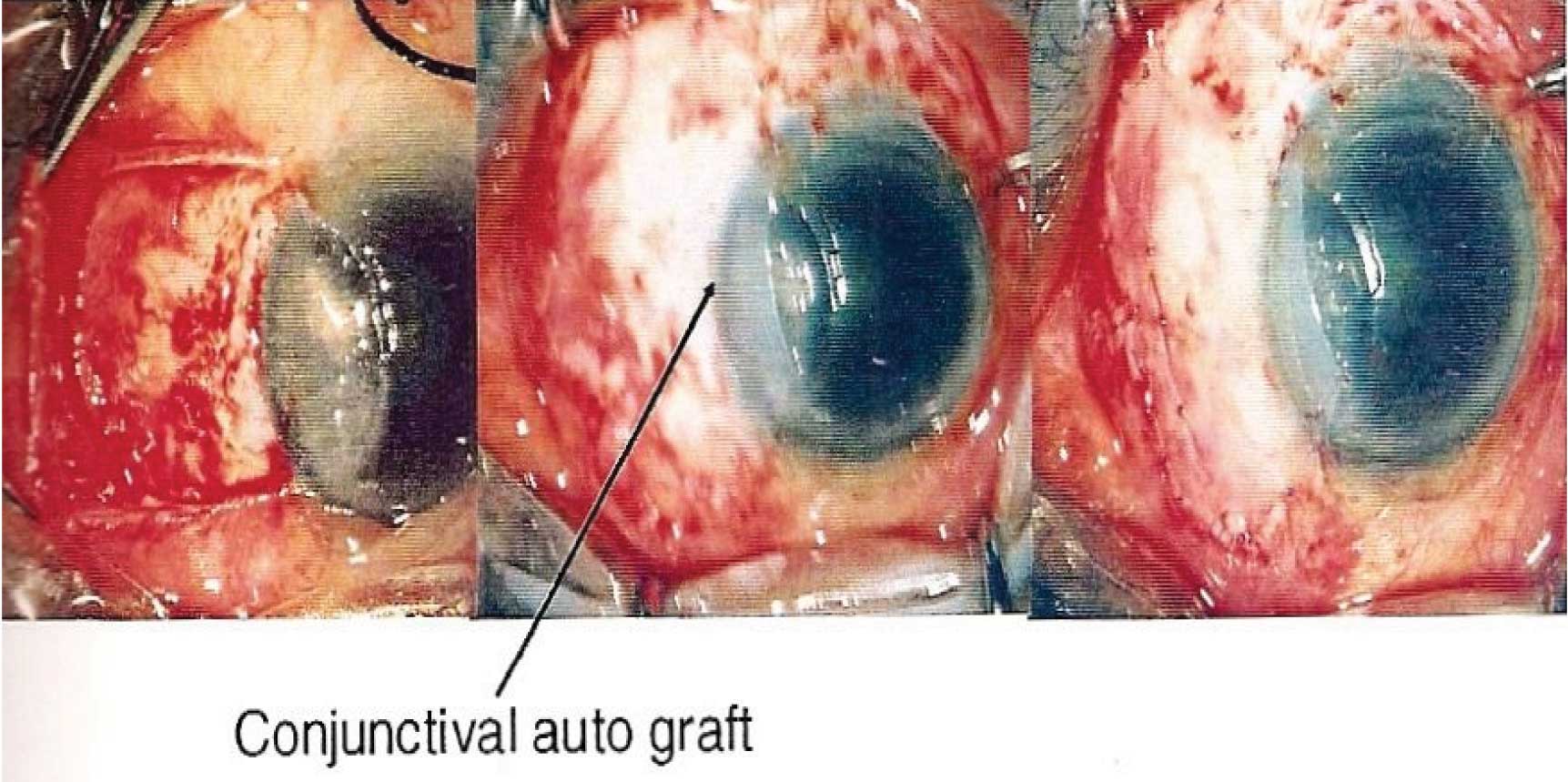
The pterygium head was recessed from the cornea. The size of the graft was determined by measuring the area of exposed sclera with caliper. The autograft was taken from the bulbar conjunctiva and it was sutured to the recessed ends of the pterygium with 8-0 silk [Table/Fig-1].
Operative Technique For Conjunctival Flap
Post-operative Regime
Post-operatively topical beta methasone eye drops were used every 2 hours for the first operative week and then tapered over the subsequent 5-6 weeks. Antibiotic ointment was used 3 times daily for 2 weeks.
Follow up visits were scheduled for post-operative days 1st, 7th, 30th, then every 2 months till six months of operation. Additional visits were mode as and when required.
Recurrence of any fibrovascular tissue past the limbus onto the clear cornea in the area of previous Pterygium constituted treatment failure.
Results
In this study 7% of cases were found in the age group of 20 – 30, about 22% belongs to the age group of 31 – 40, 30% belongs to the age group 41 – 50, and 24% in the age group of 51 – 60 and 17% were in the age group of 60 and above [Table/Fig-2].
Age and sex wise distribution of study population
| Age | Sex | Total |
|---|
| Male | Female |
|---|
| no. | % | no. | % | no | % |
|---|
| 20 – 30 | 02 | 2% | 05 | 5% | 07 | 7% |
| 31 – 40 | 13 | 13% | 09 | 9% | 22 | 22% |
| 41 – 50 | 20 | 20% | 10 | 10% | 30 | 30% |
| 51 – 60 | 13 | 13% | 11 | 11% | 24 | 24% |
| 60 and above | 12 | 12% | 05 | 5% | 17 | 17% |
| Total | 60 | 60% | 40 | 40% | 100 | 100% |
Pterygium is more often seen in men than in women. This is attributed to the fact that males are exposed to dust and environmental irritants more than women.In this study 60 patients were male and 40 patients were female. These results correlate with observations previously mentioned in the literature.
[Table/Fig-3] showed the observations of higher incidence of Pterygium in outdoor workers as compared to the indoor workers is in conformity with similar observations of other workers like McRenodl, Hilger, Kamal and Duke-Elder.
| Occupation | No. of patients | Percentage |
|---|
| Outdoor | 80 | 80% |
| Indoor | 20 | 20% |
| Total | 100 | 100% |
In this study 50 cases had Pterygium nasally. The nasal affinity of the Pterygium was attributed to the following factors.
Sparseness of the subconjunctival tissue in the temporal region and the temporal region is exposed to a lesser extent to UV radiation due to greater amount of bowing of outer 2/3 of the upper lids.
Pterygium Location
Nasal : 50%
Temporal : 30%
Both : 20%
Pterygium Laterality [Table/Fig-4]
RE : 52
LE : 38
Bilateral : 10
Total : 100
χ2 = 7.7 p < 0.001 highly significant as compared to complication of indoor and outdoor, outdoor complications are more. This is statistically highly significant [Table/Fig-5].
Occupational Incidence and Complications
| Occupation | Cases | Total |
|---|
| Normal | Complications |
|---|
| Indoor | 20 | 01 | 20 |
| Outdoor | 80 | 20 | 60 |
| Total | 100 | 21 | 100 |
Recurrence Rate in Pterygium
Recurrence of Pterygium was more frequent in patients younger than 40 age. In this study 27 patients were younger than 40 years, of these 6 developed recurrences (6.00%) [Table/Fig-6].
Recurrence Rate of Pterygium in Study
| No. of cases | Recurrent |
|---|
| Progressive primary Pterygium | 94 | 06 |
| Recurrent Pterygium | 06 | 00 |
| Total | 100 | 06 |
Discussion
There have been various efforts to optimize Pterygium surgery. These days a wide range of techniques are in use. The plan is to excise the Pterygium and prevent its recurrence. Autologous conjunctival transplant evades the risk of scleral necrosis associated with alternative adjunctive therapies.
The comparatively lower recurrences with this technique could be due to the transplantation of normal conjunctiva that forms a barrier to the proliferation and progression of residual abnormal tissue towards the limbus. It was moreover higher in patients below 40 years of age as has been described previously [5–7]. The lipoid degeneration in peripheral cornea in elderly individuals may be an inhibiting factor for Pterygium progression.
Age Incidence
According to Cameron, Young Son, Pterygium affects people living in peri equatorial regions. The highest incidence is in fourth decade. In a study conducted by Dr. Meenakshi et al., showed that 87.5% were above the age of 40 years. Another study conducted by Dr. Rao, SK et al., [8] showed that 56.98% were above the age of 40 years.
Present study showed that 73% were above the age of 40.
2) Sex Incidence
Pterygium is more often seen in men than in women. This is attributed to the fact that males are exposed to dust and environmental initiates more the than women. In the present study 60 patients were male and 40 patients were female. These results correlate with observations of JH Hillger’s [9], Rao Srinivas, Dr. Jaspreet Sukhija and many others.
Occupational Incidence
Occupation is supposed to play a major role in causing the Pterygium. In the present study majority of the patients were working out doors (80%). This fact is well supported by several authors, like MacRenolds, [10] Hillgers [9] and Kerknezov [11].
Pterygium Laterality
In the present study 50 patients had Pterygium nasally. The nasal affinity of the Pterygium was attributed to the following factors. Sparseness of the subconjutival tissue in the temporal region. The temporal region is exposed to lesser extent to UV radiation due to greater amount of bowing of outer 2/3 of the upper lid.
In a study by Fernandes, M, Sangwan, VS, Bansal, AK, et al., [12], 7.5% had bilateral Pterygium compared to 20% found in present study [Table/Fig-7].
Comparison of Recurrence Rates of Pterygium in Various Studies with Present Study
| Author | Place of study | Number of patients studied | Recurrence rate of Pterygium |
|---|
| Dowlut [13] | Canada | 15 | 8%(1) |
| Kenyon [14] | Boston | 57 | 5% (3) |
| Singh [15] | Los angeles | 13 | 8% (1) |
| Simona [16] | Geneva | 14 | 35% (5) |
| Lewallen [5] | St. Kitts | 19 | 16% (3) |
| Koch [17] | Essen | 13 | 8% (1) |
| Mizyglod [18] | Poland | 41 | 3%(1) |
| Farid [19] | California | 42 | 20% (8) |
| Bora Yuksel [20] | Turkey | 29 | 13% (4) |
| P S Mahar [21] | Pakistan | 120 | 6.7% (8) |
| KM Salagar (Present Study) | India | 100 | 6% (6) |
Complications
No major intra operative complications were encountered in this series, except 5 button holes which were repaired during the procedure Graft edema was noted in 4 cases and it responded well to short course of systemic steroids. Graft haemorrhage occurred in 3 cases and it resolved spontaneously without compromising the results.
Giant papillary conjunctivitis occurred in 3 cases and subsided after stitch removal.
Recurrence occurred in 6 (6.38%) eyes after 3-4 months post-operatively. Recurrence of Pterygium was more frequent in patients younger than 40 years age. In this study 27 patients were younger than 40 years, of these, 6 developed recurrence.
Conclusion
Autogenous conjunctival grafting is a safe, uncomplicated and quick procedure and does not involve loss of tissue and prevents recurrence of pterygium. It also reduces the risk of granuloma formation, scleral thinning and necrosis.
[1]. Hiwt L, Distribution, risk factors and epidemiology. In Taylor HR (ed) Pterygium 2000 Vol 2The Hague, NetherlandsKugler Publications:15-28. [Google Scholar]
[2]. Dushku N, Reid TW, Immunohistochemical evidence that human pterygia originate from an invasion of vimentin expressing altered limbal epithelial basal cellsCurr. Eye Res 1994 13:473-81. [Google Scholar]
[3]. Li DQ, Lee SB, Gurja–Smith Z, Liu Y, Solomon A, Meller D, over expression of collagenase (mm P-1) and stromelysin (mm P-3) by Pterygium head fibroblastsArch. Ophthalmol 2001 119:71-80. [Google Scholar]
[4]. Hirst LW, The treatment of PterygiumSurv. Ophthalmology 2003 45:145-80. [Google Scholar]
[5]. Lewallen SA, Randomized trial of conjunctival autografting for pteryigum in the tropicsOphthalmology 1989 96:1612-14. [Google Scholar]
[6]. Chen PP, Ariyasu RG, Kaza V, LaBree LD, McConnell PJA, randomized trail comparing mitomcyin C and conjunctival autograft after excision of primary PterygiumAm. J. Opthalmol 1995 120:151-60. [Google Scholar]
[7]. Mannis CA, Koless PM, Diaz D, Yee RW, Intra-operative mitocyin in primary Pterygium excisionOphthalmology 1997 104:844-48. [Google Scholar]
[8]. Rao SK, Lekha T, Mukesh BN, Sitalakshmi G, Padmanabhan P, Conjunctival limbal autografts for primary and recurrent pterygia: technique and resultsIndian J. Opthalmology 1998 46:203-09. [Google Scholar]
[9]. Hilgers JH, Pterygium on the island of ArubaAmsterdam Klein Offset Drukkerjj Poortpers NV 1959 [Google Scholar]
[10]. McReynolds JO, The nature and treatment of pterygiaJAMA 1902 39:296 [Google Scholar]
[11]. Kerkenezov N, TransOphthalmic society Aust. 16 1956 110 [Google Scholar]
[12]. Fernandes M, Sangevan VS, Bansal AK, Gangopadhyay N, Sridhar MS, Garg P, India; Outcome of Pterygium surgery bt. 1988-2001Eye 2005 19(11):1182-90. [Google Scholar]
[13]. Dowlut M S, Laflamme M Y, Les pterygions recidivants: frequence et correction par autogreffe conjonctivaleCan J Ophthalmol 1981 :16119-120.120.[PubMed] [Google Scholar]
[14]. Kenyon KR, Wagoner MD, Hettinger ME, Conjunctival autograft transplantation for advanced and recurrent pterygiumOphthalmology 1985 92:1461-70. [Google Scholar]
[15]. Singh G, Wilson MR, Foster CS, Long-term following up to do study of mytomicin drops as adjunctive treatment of pterigia and its comparison with conjunctival autograft transplantationCornea 1990 9:331-34. [Google Scholar]
[16]. Simona F, Tabatabay CA, Leunberger PM, Preliminary results of ptery-gium excision with conjunctival autograftingKlink Monatsbl Augenheilkd 1990 196:295-7. [Google Scholar]
[17]. Koch M, Mellin JB, Waubke TN, Initial experience with autologous con-junctival transplantation in pterygiumKlin Monatsbl Augenheilkd 1990 197:106-9. [Google Scholar]
[18]. Mrzygiot S, Scubit Zewsca T, Surgery for pterygium with transplantation of an epithelial conjunctival flapKlin Ozna 1990 92:99-100. [Google Scholar]
[19]. Farid M, Pirnazar JR, Pterygium recurrence after excision with conjunctivalautograft: a comparison of fibrin tissue adhesive to absorbable suturesCornea 2009 8(1):43-45. [Google Scholar]
[20]. Yuksel B, Unsal SK, Onat S, Comparison of fibrin glue and suture technique in pterygium surgery performed with limbal autograftInt J Ophthalmol 2010 3(4):316-320. [Google Scholar]
[21]. Mahar PS, Pterygium recurrence related to its size and corneal involvementJournal of the College of Physicians and Surgeons 2013 Vol. 23(2):120-23. [Google Scholar]