Purpose: To study the efficacy and safety of Posterior Sub-Tenon Triamcinolone acetonide (PSTT) in the treatment of macular edema in retinal vein occlusions. The efficacy is studied by anatomical and visual improvements.
Background: Macular edema is the most common cause of visual loss in retinal vein occlusions. Many treatments have been advocated including laser, PSTT etc. The most recent trend is the usage of intravitreal Anti-VEGF (Vascular Endothelial Growth Factor) agents and steroids. Intravitreal injections have more complications.
Methods: This study was a prospective interventional case series. 24 eyes of 24 patients (13 male and 11 female) with recent onset non-ischemic RVO (Retinal Vein Occlusion) underwent Posterior Sub-Tenon Triamcinolone (PSTT). Of the 24 eyes treated, 18 eyes were of BRVO (Branch Retinal Vein Occlusion) and 6 were CRVO (Central Retinal Vein Occlusion). All the eyes received 40 mg of Triamcinolone Acetonide (TA) in 1ml through posterior sub-tenon route. All the eyes were examined at baseline and after four weeks of being injected with TA. Changes in the best corrected visual acuity {letters of ETDRS (Early Treatment Diabetic Retinopathy Study) chart} and Central Macular Thickness (CMT) were studied. A gain of more than 5 letters was considered as effective. The eyes were examined for raised IOP (Intra-Ocular Pressure) and other complications.
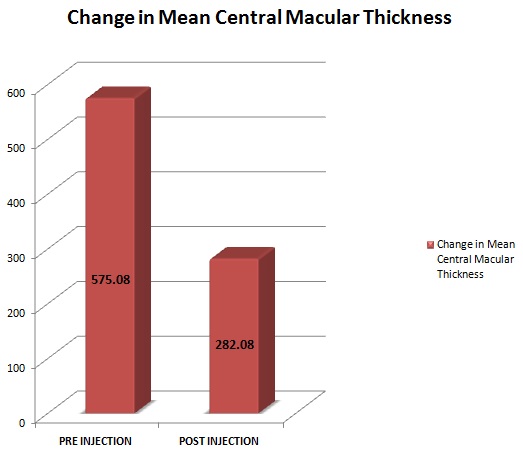
Results: Out of the 24 eyes 19 (79%) showed an improvement of more than 5 letters after a month of treatment. All the patients exhibited a certain degree of decrease in CMT. The mean BCVA increased from 30.08±10.16 to 40.21±8.93 (p<0.05). The mean CMT decreased from 575.08±131.55 to 282.08±163.99 (p<0.05).
Out of them 3 eyes developed raised IOP of more than >21mmHg, which was controlled with medication. There were no other complications observed in any of the patients.
Conclusion: PSTT is an effective modality of treatment with minimal complications for macular edema associated with Non-Ischemic RVO with minimal complications. In view of the more severe complications associated with intravitreal injections, PSTT can be used as the first line of treatment before contemplating intravitreal injections. Multicenter randomised trials with longer periods of follow–up are needed to evaluate the long term safety and efficacy of this treatment. Furthermore, comparative studies are required to compare it with intravitreal Anti–VEGF or TA.
Introduction
Retinal vein occlusion (RVO) is the second most common retinal vascular disease, next only to diabetic retinopathy [1]. In a study conducted in central India, RVOs were detected in 0.8% of the adults examined, with branch vein occlusions being approximately seven times more common than central vein occlusions [2].There are two variants: non-ischemic and ischemic [3]. The causes for visual loss are macular edema and ischemia. Macular edema (ME) is the most common cause for visual loss in both variants of RVO [4].
Vein occlusion results in poor venous drainage, leading to secondary inflammation which results ultimately in the breakdown of the blood-retinal barrier with exudation of blood, fluid, and lipid into the retina, leading to the development of macular edema[5].
The role of Vascular Endothelial Growth Factor (VEGF) in blood-retinal barrier breakdown has been established. The increased back-pressure leads to stagnation of blood flow, which leads to hypoxia of the retina causing the release of various chemical agents, of which VEGF is important [6]. VEGF disrupts the blood–retinal barrier by inducing fenestrations in capillaries and venules[7].
Treatment of ME is imperative to improve the vision. A study revealed that not a single case of macular edema with central retinal vein occlusion resolved spontaneously within a year.However, approximately 30% of the cases resolved spontaneously over a long interval, often with neuroretinal or pigment epithelial scarring and atrophy [8]. Resolution of ME can be long delayed. In one study, the time taken for resolution of ME in untreated Non-ischemic CRVO with ME averaged 23 months compared to 29 months for Ischemic CRVO [9].Spontaneous resolution of BRVO associated ME is better, but it can still lead to macular damage without intervention [10].
Macular grid laser was considered the gold standard treatment [11]. But the Central Vein Occlusion Study (CVOS) proved that macular grid laser doesnot improve vision. There was no statistically significant difference in visual acuity between treatment and control groups at any stage of the follow-up [12].The Branch Vein Occlusion Study (BVOS) has advised grid laser for macular edema of more than three months duration [1]. But postponing treatment for more than three months would adversely affect the collaterals, and cause more damage to the macula. Therefore, early treatment with intravitreal or periocular injections was advised [13,14].
Triamcinolone-acetonide is a corticosteroid that, in addition to its anti-inflammatory effects, cause down-regulation of vascular endothelial growth factor (VEGF) [15]. Triamcinolone intravitreally was largely used with good results in ME of RVO [16,17]. Intravitreal Triamcinolone may be associated with various complications like glaucoma, cataract, endophthalmitis, retinal detachment, scleritis, etc [18,19].
Since the first report of the efficacy of Intravitreal Bevacizumab (IVB) in a patient with ME secondary to CRVO in 2005 [20], several case series have shown the benefit of this treatment, with improvement in visual acuity in patients with ME with RVO [21].
The need for an operation theatre setup and the cost of the Anti-VEGF drug may be limiting factors for many patients. As it is an intraocular procedure, it may be associated with severe complications including endophthalmitis, retinal detachment etc.[22]. Intra-ocular Anti-VEGF can be associated even with systemic complications [22].
Taking the above factors into consideration, the technique of Posterior sub-tenon Triamcinolone (PSTT) which has already been used for many indications like Diabetic Macular Edema, Uveitis etc [23,24] may be analysed for its effectiveness in the treatment of ME associated with RVO. As the posterior sub-tenon space is adjacent to the macular area,the steroid deposited in that area would transfuse through the sclera and act on the macular edema.
This study is aimed to study the efficacy and safety of PSTT in macular edema associated with retinal vein occlusions.
Material and Methods
This study is a prospective interventional case series done during March 2011 and March 2012 in ophthalmology department of a tertiary health care center in Hyderabad, south India.
Inclusion criteria
Macular edema with Non-Ischemic Retinal Vein Occlusion as evidenced by clinical and angiographic evaluation.
Decreased vision with vision better than PLand less than 70 letters on ETDRS chart, of duration less than one month.
CMT ≥ 250 μ.
Exclusion criteria
Ischemic RVO
Prior laser treatment
Glaucoma/Ocular Hypertension
Cataract which precludes the evaluation of macula
Vitreous hemorrhage
Macular ischemia
Iris neovascularisation
Prior intravitreal injections
With power of 80%, significance level of 0.05 and 6 letters of minimum significance, a sample size of 22 were calculated.Approval was obtained from the Head of the Institute.Total number of 24 eyes of 24 patients were included after taking written informed consent. All these patients underwent basic eye examination including Best Corrected Visual Acuity (BCVA) with 4 meter ETDRS chart (4m ETDRS chart model no. 2121, Akriti Logistics) with 70 letters in 14 lines, thorough slit lamp examination, Goldman Applanation Tonometry (GAT), Contact lens biomicroscopy (CLB), Indirect ophthalmoscopy (IO), Fundus Fluorescein Angiography (FFA), and Optical Coherence Tomography (Time domain OCT, Zeiss Stratus OCT). Demographics of the patients are given in [Table/Fig-1].
| n=24* | Mean±SD† |
|---|
| Age | 43-78 | 62.13±10.39 |
| Sex | M‡: 13 (54.2%) F§,: 11 (45.8%) | |
| Type of vein occlusion | CRVO||: 6 (25%) BRVOζ: 18 (75%) | |
| Eye | RE**: 13 (54.2%) LE††: 11 (45.8%) | |
| Pre-PSTT BCVA‡‡ (No. Of letters on ETDRS§§ chart) | 14-46 | 30.08±10.16 |
| Pre-PSTT||||CMTζζ | 334-789 | 575±131.54 |
*n=Number of eyes, †SD=Standard Deviation, ‡M=Male, §F=Female,
||CRVO=Central Retinal Vein Occlusion, ζBRVO=Branch Retinal Vein Occlusion,
**RE=Right Eye, ††LE=Left Eye, ‡‡BCVA=Best Corrected Visual Acuity,
§§ETDRS=Early Treatment Diabetic Retinopathy Study, ||||PSTT=Posterior Sub–
Tenon Triamcinolone, ζζCMT=Central Macular Thickness
The technique of injection was as described by Nozik [25]. All injections were given as out-patient procedures. The patient was made to lie down comfortably on the treatment couch. Topical anesthesia drops (Proparacaine 0.5%) were instilled twice with an interval of five minutes.The first drop was placed in the inferior cul-de-sac and the second drop was placed over the super otemporal quadrant, after asking the patient to look inferonasally. A 2 ml syringe was loaded with 1ml (40 mg) of preservative free Triamcinolone Acetonide (Aurocort, Aurolabs, India). The needle was replaced with a 26G half–inch needle. The surgeon positioned himself on the opposite side of the patient. The patient was asked to stare at his/her opposite shoulder (Inferonasal gaze). With the left hand, the surgeon retracted the upperlid upwards, thus exposing the superotemporal quadrant. The needle was passed through the bulbar conjunctiva and tenon’s capsule at the posterior most visible area, with the bevel facing towards the globe. Maintaining the needle as close as possible to the globe,the needle was advanced. Side to side movement of the needle was made and the limbus was looked for any movement. Any movement of the limbus indicates the presence of needle in the sclera. The needle was advanced till the hub was reached over the injection site. Aspiration was done to rule out any blood vessel entry, and then the drug was injected with moderate force.
Post–procedure instructions for all patients were the same with oral Acetazolamide and Non-steroidal Anti-Inflammatory Drugs (NSAID). Topical medications include Steroid-Antibiotic combination for five days and anti–glaucoma medication, usually Timolol 0.5% for a month. Acetazolamide 250 mg was given thrice daily for a day. NSAID was given for two days.
Patients were seen after a month, unless any patient noticed complications. They were examined with the same parameters like VA, GAT, IO,FFA,OCT etc.
The effectiveness of the treatment was judged by visual improvement of more than 5 letters.
Statistical Analysis was made with SPSS software (SPSS for Windows, version 13.0, SPSS Inc., Chicago, Illinois, USA). Student’s t-test was used. For the effect on BCVA and CMT, paired sample statistics was done with 95% confidence interval. To know the difference between CRVO and BRVO, effect in both groups on BCVA and CMT was compared with independent samples T test.
Results
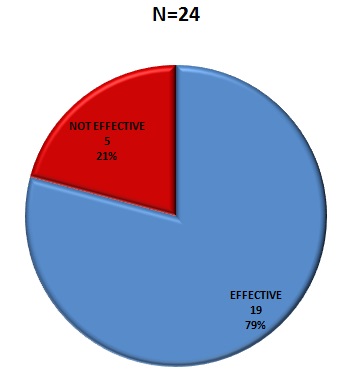
All the patients turned up for the follow-up after four weeks. 19 eyes showed an improvement of more than 5 letters, which is 79%. Of the remaining 5 eyes, 2 eyes showed a loss of one number and the other 3 showed an improvement of less than 5 letters. All 24 eyes showed atleast some reduction in CMT. The treatment was 79% effective [Table/Fig-2].
Effectiveness of the treatment (improvement of more than 5 letters) No. of Eyes=24, Effective in 19 eyes and Not effective in 5 eyes
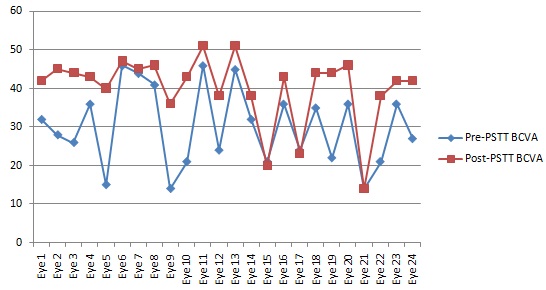
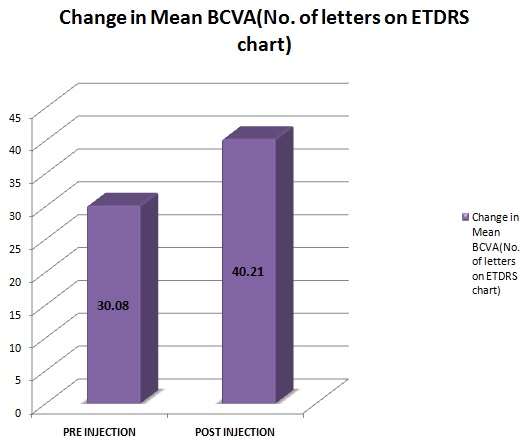
The Pre-operative and Post-operative BCVA of individual eyes are depicted in [Table/Fig-3]. The mean Pre-operative visual acuity in terms of numbers was 30.08. The standard deviation was 10.16 with standard error of mean 2.08. The mean Post-operative BCVA was 40.21 with standard deviation 8.93 and standard error mean 1.82. The Pre and Post–operative values were analysed with paired samples test. The mean change in VA was 10.13 with standard deviation 8.20 and standard error mean 1.67. The 2 tailed p value was < 0.005, suggesting that the treatment improved the visual acuity which is statistically significant [Table/Fig-4].
BCVA (No. of ETDRS Letters) in individual eyes, Pre and Post PSTT
Change in Mean Visual Acuity
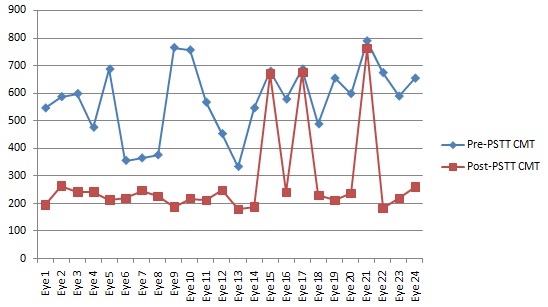
The Pre-operative and Post-operative CMT of individual eyes are depicted in [Table/Fig-5]. The mean Pre-operative central macular thickness (CMT) was 575.08 microns with standard deviation 131.55 and standard error mean 26.85. The mean Post-operative CMT was 282.08 microns with standard deviation 163.99 with standard error mean 33.48. The change in central macular thickness was 293 microns with standard deviation of 162.67 and standard error mean 33.21. The 2 tailed p value was < 0.005 which suggests that PSTT reduced the central macular thickness to a statistically significant level [Table/Fig-6].
CMT in individual eyes, Pre and Post PSTT
Intergroup analysis
Mean increase in BCVA in CRVO group was 9.17±9.02 (n=6) and in BRVO 10.56±7.85 (n=18) with p-value of 0.72, suggesting no statistically significant difference. Mean decrease in CMT in CRVO and BRVO were 277±214.67 and 298.33±148.75 with p-value of 0.79 which again is not significant statistically.
Complication
No serious complication was noted at any point of time. Raised IOP was noted in 3 eyes (8%), one week after the injection,which was controlled by the addition of Brimonidine,to Timolol, which was already being used. None developed complications such as Glaucoma, perforation, infection etc.
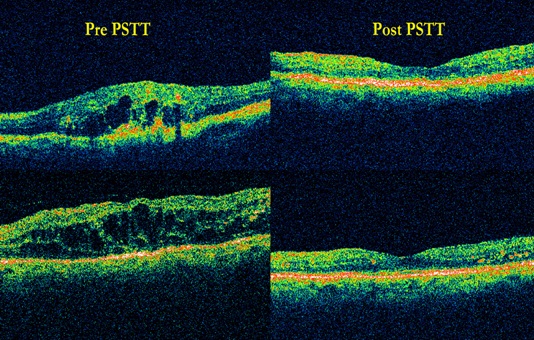
Examples for the OCT changes in the macula pre and post-PSTT are shown in [Table/Fig-7].
Optical Coherence Tomography (OCT) images of Pre and Post-PSTT
Discussion
Macular edema is the most common cause for decreased vision in patients with RVO. The macular edema is of vasogenic edema unlike in ischemic RVO where the edema is cytotoxic macular edema.
Due to vein obstruction, blood stagnates in the venous system, thus increasing pressure in the capillary system leading to derangement in Starling’s forces. These changes also lead to secondary inflammation and result ultimately in the breakdown of the blood- retinal barrier with exudation of blood, fluid, and lipid into the retina leading to the development of macular edema. Many cytokines such as VEGF, Transforming Growth Factor, Tumor Necrosis Factor, Platelet Derived Growth Factor, Interleukin-6,Fibroblast Growth Factoretc are involved in this process. VEGF is the major vasopermeability factor that disrupts the blood–retinal barrier in RVO by inducing fenestrations in capillaries and venules.
The average vitreal concentration of VEGF in CRVO is 8.6 ng/ml in CRVO and 2.0 ng/ml in BRVO as compared to 0.26 ng/ml in normal eyes [26].A lower concentration of intraocular VEGF is required to increase vascular permeability than that required to induce neovascularisation.
Untreated macular edema in RVO typically persists for a long time. In one study, the median time for macular edema resolution was 23 months for Non-ischemic CRVO and 29 months for Ischemic CRVO [9]. Chronic macular edema and macular cysts in CRVO can result in a lamellar or full thickness macular hole [27].
Early treatment of macular edema may be better for visual improvement before longstanding macular edema results in irreversible photoreceptor damage [28].
Intravitreal Triamcinolone and anti-VEGF agents are being used for several years now [20,28].
Posterior sub-tenon Triamcinolone has been used for many indications like DME, Uveitis etc [23,24].
Lin et al., in a prospective, non-comparative study treated 18 eyes of 18 patients of severe CME with recent onset CRVO, with PSTT. They concluded that PSTT is effective in reversing CME and improving VA in recent-onset CRVO. They also recommended early treatment before long-standing macular edema results in irreversible photoreceptor damage [29].
In another prospective study, Nil et al., evaluated 24 eyes with macular edema secondary to RVO. All the eyes were treated with PSTT. 58.3% showed increased BCVA with no major complications. They concluded that PSTT was an effective therapeutic method to treat ME associated with RVO [30]. The percentage of people improving VA in our study is 79%which is high compared to the above mentioned study. This can be explained by the fact that we excluded Ischemic RVO and we studied recent onset macular edema unlike Nil et al.
The patients were put on Timolol eye drops post PSTT. Three eyes developed raised IOP more than 21mmHg. Treatment with Brimonidine was started and the IOP was controlled. No other complications were noted in any of the eyes. This was similar to other studies.
Short follow-up is the major limitation of this study. Long term follow-up was needed to know the long-term effect of PSTT and its complications. Comparative studies of PSTT with Intravitreal Steroids or anti-VEGF are required.
Conclusion
Posterior sub-tenon injection of Triamcinolone Acetonide is beneficial in increasing visual acuity and decreasing central macular thickness in cases of recent onset macular edema due to retinal vein occlusions. No complications were noted. In view of reported complications with intravitreal injections, PSTT can be tried as the first line of treatment, before contemplating intravitreal injections.
Multicenter trials with controls and longer follow-ups are needed to evaluate the long term safety and efficacy of this treatment. Comparative studies are needed to compare PSTT with intravitreal Triamcinolone and Avastin.
[1]. The Branch Vein Occlusion Study GroupArgon laser photocoagulation for macular edema in branch vein occlusionAm J Ophthalmol 1984 98:271-82. [Google Scholar]
[2]. Jonas JB, Nangia V, Khare A, Sinha A, Lambat S, Prevalence and associations of retinal vein occlusions: the Central India Eye and Medical StudyRetina 2013 33(1):152-9. [Google Scholar]
[3]. Hayreh Sohan Singh, Retinal vein occlusionIJO 1994 42(3):109-32. [Google Scholar]
[4]. The Central Vein Occlusion Study GroupNatural history and clinical management of central retinal vein occlusionArch Ophthalmol 1997 115:486-91. [Google Scholar]
[5]. Lee HB, Pulido JS, McCannel CA, Buettner H, Role of inflammation in retinal vein occlusionCan J Ophthalmol 2007 42(1):131-33. [Google Scholar]
[6]. Behzadian MA, Wang XL, Al-Shabrawey M, Caldwell RB, Effects of hypoxia on glial cell expression of angiogenesis–regulating factors VEGF and TGF–betaGlia 1998 24:216-25. [Google Scholar]
[7]. Schlingemann RO, van Hinsbergh VWM, Role of vascular permeability factor/vascular endothelial growth factor in eye diseaseBr J Ophthalmol 1997 81:501-12. [Google Scholar]
[8]. McIntosh RL, Rogers SL, Lim L, Cheung N, Wang JJ, Mitchell P, Kowalski JW, Nguyen HP, Wong TY, Natural history of central retinal vein occlusion: Evidence -based systematic reviewOphthalmology 2010 117:1113-23. [Google Scholar]
[9]. Hayreh SS, Podhajsky PA, Zimmerman MB, Natural history of visual outcome in central retinal vein occlusionOphthalmology 2011 118:119-33. [Google Scholar]
[10]. Haller JA, Bandello F, Belfort R Jr, Blumenkranz MS, Gillies M, Heier J, OZURDEX GENEVA Study Group: randomised, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusionOphthalmology 2010 117:1134-46. [Google Scholar]
[11]. Arnarsson A, Stefánsson E, Laser treatment and the mechanism of edema reduction in branch retinal vein occlusionInvest Ophthalmol Vis Sci 2000 41:877-09. [Google Scholar]
[12]. The Central Vein Occlusion Study GroupEvaluation of grid pattern photocoagulation for macular edema in central vein occlusion: The Central Vein Occlusion Study Group M reportOphthalmology 1995 102:1425-33. [Google Scholar]
[13]. Oh JY, Seo JH, Ahn JK, Heo JW, Chung H, Early versus late intravitreal triamcinolone acetonide for macular edema associated with branch retinal vein occlusionKorean J Ophthalmol 2007 21:18-20. [Google Scholar]
[14]. Lin JM, Chiu YT, Hung PT, Tsai YY, Early treatment of severe cystoid macular edema in central retinal vein occlusion with posterior sub-tenon triamcinolone acetonideRetina 2007 27:180-89. [Google Scholar]
[15]. Nauck M, Roth M, Tamm M, Induction of vascular endothelial growth factor by platelet-activating factor and platelet-derived growth factor is down regulated by corticosteroidsAm J Resp Cell Mol Biol 1997 16:398-406. [Google Scholar]
[16]. Ip MS, Gottlieb JL, Kahana A, Scott IU, Altaweel MM, Blodi BA, Intravitreal triamcinolone for the treatment of macular edema associated with central retinal vein occlusionArch Ophthalmol 2004 122(8):1131-36. [Google Scholar]
[17]. Karacorlu M, Ozdemir H, Karacorlu SA, Resolution of serous macular detachment after intravitreal triamcinolone acetonide treatment of patients with branch retinal vein occlusionRetina 2005 25:856-60. [Google Scholar]
[18]. Konstantopoulos A, Williams CP, Newsom RS, Luff AJ, Ocular morbidity associated with intravitreal triamcinolone acetonideEye (Lond) 2007 21(3):317-20. [Google Scholar]
[19]. Ozkiri A, Erkiliç K, Complications of intravitreal injection of triamcinolone acetonideCan J Ophthalmol 2005 40:63-68. [Google Scholar]
[20]. Rosenfeld PJ, Fung AE, Puliafito CA, Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for macular edema from central vein occlusionOphthalmic Surg Lasers Imaging 2005 36:336-39. [Google Scholar]
[21]. Hsu J, Kaiser RS, Sivalingam A, Intravitreal bevacizumab (avastin) in central vein occlusionRetina 2007 27:1013-19. [Google Scholar]
[22]. Shima C, Sakaguchi H, Gomi F, Kamei M, Ikuno Y, Oshima Y, Complications in patients after intravitreal injection of bevacizumabActa Ophthalmol 2008 86(4):372-76. [Google Scholar]
[23]. Bakri SJ, Kaiser PK, Posterior subtenon triamcinolone acetonide for refractory diabetic macular edemaAm J Ophthalmol 2005 139:290-94. [Google Scholar]
[24]. Helm JH, Holland GN, The effects of posterior sub tenon injection of triamcinolone acetonide in patients with intermediate uveitisAm J Ophthalmol 1995 120:55-64. [Google Scholar]
[25]. Nozik RA, Periocular injection of steroidsTrans Am Acad Ophthalmol Otolaryngol 1972 76:695-705. [Google Scholar]
[26]. Ehlken C, Rennel ES, Michels D, Levels of VEGF but not VEGF 165b are increased in the vitreous of patients with retinal vein occlusionAm J Ophthalmol 2011 152:298-303. [Google Scholar]
[27]. Shukla D, Rajendran A, Kim R, Macular hole formation and spontaneous closure after vitrectomy for central retinal vein occlusionGraefes Arch Clin Exp Ophthalmol 2006 244:1350-52. [Google Scholar]
[28]. Lee Henry, Shah Gaurav K, Intravitreal Triamcinolone As Primary Treatment of Cystoid Macular Edema Secondary to Branch Retinal Vein OcclusionRetina July/August 2005 25(5):551-55. [Google Scholar]
[29]. Lin JM, Chiu YT, Hung PT, Tsai YY, Early treatment of severe cystoid macular edema in central retinal vein occlusion with posterior sub-tenon triamcinolone acetonideRetina 2007 Feb 27(2):180-89. [Google Scholar]
[30]. Nil Rem, Mehmet Cenk Zeliha Gursel Emin, Posterior Subtenon Triamcinolone Acetonide in the Treatment of Macular Edema Secondary to the Retinal VeinOcclusion Journal of Retina-Vitreous 2004 12(3):180-83. [Google Scholar]