Actual perinatal period commences from 22 weeks of gestation period i.e., 154 days to seven days of life. At this time, foetus approximately weighs 500 gms. However as standard perinatal statistics include births weighing 1000 gms in both numerator and denominator, which is achieved at 28 weeks of gestation. Hence, for international comparision, it is defined as, “Period between 28 weeks of gestation and seven days after life”. Crown to heel length is also ascertained if gestational age and birth weight are unavailable. Body length of 35 cm corresponds to this age and weight, (International Classification of Diseases-10) [1,2]. Perinatal period accounts for just 0.5% of the average life span, but deaths in this period are more than that in the next 30-40years [3]. With the reduction of national IMR below 50, Perinatal Mortality Rate is being considered as an important epidemiological indicator of Maternal and Child Health care of the country because of its sensitivity for both maternal and newborn care. Moreover, it avoids the confusion between late foetal deaths, still births and deaths within hours after birth. Deaths during this period can result because of inadequate care of both maternal and newborn care.
Over 130 million babies are born every year, and more than 10 million children die before their fifth birthday, almost 8 million before their first. Infant mortality rate of India in the year 2009 was 50. For rural & urban areas it was 55 & 34 respectively [4]. Perinatal mortality rate of India in 2007 was 37, 41 & 24 for total, rural & urban areas respectively per 1000 live births [5]. Karnataka had prevalence of 35, 26 & 40 for total, urban & rural areas respectively [5,6]. There are various socio-biological risk factors contributing for perinatal mortality. Some of which are, low Socio-economic Status, illiteracy, high maternal age, teenage pregnancies, high parity, short spacing, poor obstetric history, malnutrition & severe anemia [1]. The causes of perinatal mortality can be classified into antenatal, intra-natal, Post-natal. Important causes include, intra-uterine and birth asphyxia, low birth weight, birth trauma, intra-uterine and neonatal infections [1]. Study of mortality during this period will give a clear picture of the Maternal and Child Health care facilities in an area. In this background the present study was conducted with the objectives of estimating the prevalence and factors influencing of perinatal mortality in rural areas of Mysore district, India.
Methodology
Study Design: Cross sectional community based study was conducted to know the prevalence in the field practice area. Whole population of the Primary health centre was covered (hence no sampling procedure was used). All the births and deaths to the permanent resident mothers during the study period (one year), in the study area were included in the study.
This cross sectional, community based study was carried out in villages under Hadinaru primary health centre catering population of 26,977 in Nanjangud talluk of Mysore district, India. All the mothers who had delivered during the period of January to December 2010 and permanently residing in the villages under the study area were included in the study. Women residing outside the study area but who had come to their maternal house for delivery were excluded.
Institutional ethics committee approval was obtained before starting the study. Data collection was carried out during the first half of the year 2011. On visiting each village, mothers who delivered during January to December 2010 were line listed with the help of Anganwadi and ASHA(Accredited Social Health Activist) workers. Then every mother was visited at her house along with ASHA worker. Information about any other deliveries in their surrounding was taken from the family members and they were also covered. Thus, by snow ball sampling method all the mothers eligible to be included in the study were covered. This ensured that the mothers who were missed by anganawadi and ASHA workers were also included in the study. purpose of study was explained to the mother and consent was taken before starting the interview. Details about antenatal, intra-natal and post-natal events were collected using a pre-tested, semi-structured proforma including all the major risk factors for the perinatal deaths. Factors like, height, weight, age of the mother, past obstetric history, haemoglobin percentage, parity, time interval between successive pregnancies, socio-economic status, literacy status of the mother, birth weight of the baby, intra-partal complications, neonatal complications, gestational age at birth and number of antenatal check-ups and weight gain during pregnancy, time for initiation of breast feeding, prelacteal feeds given, any unusual feeding habits (if practiced) were included in the proforma. Hospital records like antenatal check up card, hospital discharge card, vaccination card were referred wherever available, otherwise mother was asked for the details required.
There was no scope for clinical examination. In all cases mother was the main respondent as there were no maternal deaths. At the time of interview help of other family members (Husband and mother in law) was also utilized to gather the information.
Data analysis was carried out by using Epi-info software. Association between perinatal mortality and various risk factors were studied by applying Chi-square test or Fishers exact test(if observed frequency less than five).
Results
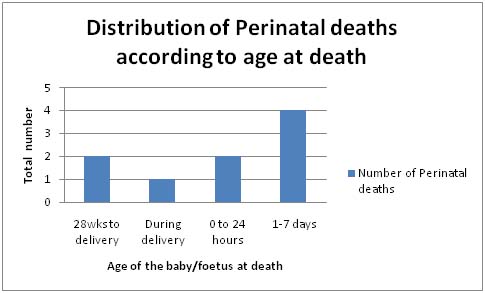
Three hundred and forteen births occurred to 311 mothers with a birth rate of 11.6 per 1000 population. There were 3 twin deliveries. Male babies were 141(45%) and female 173(55%) with a favourable sex ratio of 1226 females per 1000 male births. Nine perinatal deaths were observed which brings about Perinatal Mortality Rate of 28.93 per 1000 live births. As evident from [Table/Fig-1], there were three still births (Still birth rate of 9.55 per 1000 total births), six early neonatal deaths (Early neonatal mortality rate was 19.29 per 1000 live births).
Socio-demographic details of study population (n=311)
| Parameter | Number | Percentage |
|---|
| Age of mothers (in years) |
| ≤20 | 154 | 49.5 |
| 21-25 | 140 | 45.1 |
| 26-30 | 15 | 4.8 |
| >30 | 02 | 0.6 |
| Sex of children born during 2010 (n314) |
| Male | 141 | 44.9 |
| Female | 173 | 55.1 |
| Educational status of Mothers |
| Illiterate | 48 | 15.6 |
| Primary (Class 1 to 4) | 22 | 7.0 |
| Middle (Class 5 to 7) | 75 | 24.2 |
| High school and PUC | 155 | 49.7 |
| Degree & diploma | 11 | 3.5 |
| Mother’s occupation |
| Housewives | 301 | 96.8 |
| Working | 10 | 3.2 |
| Father’s occupation |
| Labour | 182 | 59.2 |
| Semi-skilled | 63 | 20.4 |
| Skilled | 58 | 18.5 |
| Professional | 8 | 1.9 |
| Socio-economic status |
| Class I | 12 | 3.9 |
| Class II | 59 | 18.9 |
| Class III | 120 | 38.6 |
| Class IV | 112 | 36.0 |
| Class V | 8 | 2.6 |
One hundred and eleven (35.7%) mothers were married before the age of 18 years and 154 (49.5%) had delivered before 20 years of age (teenage). Anemia was a major problem with 193 (62%) mothers suffering from it. There were 15 (4.8%) home deliveries out of which birth weight was not recorded in 8 cases. In others it was measured by the health worker on subsequent days. Twelve (3.8%) deliveries were conducted by untrained personnel, either by relatives or by traditional dais. Prevalence of Low Birth Weight was 20.1% with mean birth weight of 2713 ± 576 gms. Among the 61 LBW babies only two were in very low birth weight category (less than 1500 gms). There were no cases of extremely low birth weight. Fourteen babies weighed above 3500 gms.
As observed from [Table/Fig-2], infants who had suffered from intra- uterine complications, intra-partal complications, premature babies, babies with delayed onset of first cry, twin babies had higher risk for perinatal mortality which was found to be statistically significant.
Risk factors associated with perinatal mortality
| Parameter | Number | Percentage | p-value |
|---|
| Intrapartal complication | | | |
| Present | 19 | 04 | 0.01 |
| Absent | 286 | 05 | |
| Intra uterine complication | | | |
| Present | 01 | 03 | 0.01 |
| Absent | 304 | 06 | |
| Gestational age at birth | | | |
| Premature | 06 | 03 | 0.01 |
| Mature | 299 | 06 | |
| Time taken for first cry | | | |
| Immediate | 305 | 07 | 0.01 |
| Delayed/dint cry | 0 | 02 | |
| Multiple pregnancy | | | |
| Twin | 03 | 03 | 0.01 |
| Single | 302 | 06 | |
| Note: Chi-square/Fisher’s exact test was applied |
Higher Perinatal Mortality Rate [Table/Fig-3] was also observed in mothers who had married before 18 years of age, conceived before 20 years (teenage mothers), belonging to lower Socio-economic status, those who dint consume Iron and Folic Acid(IFA) tablets, anemic during third trimester, had antenatal complications like pre eclampsia and had normal vaginal delivery. Higher Perinatal Mortality Rate was seen in male babies, babies fed with pre-lacteal feeds and having low birth weight, but the difference was not statistically significant.
Distribution of Perinatal deaths according to age of the baby/foetus at death
Discussion
Perinatal Mortality Rate in India has decreased considerably in past decade. The overall prevalence was 48.1 per 1000 live births in 1986 with urban and rural prevalence being 32.7 and 51.8 per 1000 live births respectively. It has been reduced to 37 per 1000 live births with urban area having rate of 24 and rural area 41 per 1000 live births in the year 2009 [1]. Karnataka has Perinatal Mortality Rate of 35, 15 and 44 per 1000 live births for total, urban and rural areas respectively [3].
Prevalence of Perinatal Mortality Rate in the present study was 28.93 per 1000 live births which is well below the national average for rural community. This is in contrast to the findings of various community based studies, which have reported Perinatal Mortality Rate in the range of 88.5 (Jabalpur, 1986) [7], 81(Pune, 1988) [8], 59 (Luknow,1993) [9] and 51(Pune, 2005) [10] per 1000 live births and another study conducted in Mysore by Narayanamurthy MR [11] in 1998 had observed a prevalence of 67.75 per 1000 live births. This lower prevalence in the present study can be attributed to the better healthcare facilities provided in this area as most of the villages in study area could access a hospital within ten kms radius. Mothers in study area were fairly educated and were aware of the facilities. They had help of ASHA workers in every village and Junior health assistants for better care. After implementation of National Rural Health Mission, the transport facility is being provided to the pregnant mothers. This has greatly improved the proportion of institutional deliveries. All the pregnancies were registered and more than 95% were institutional deliveries. But the problem of early marriage is still prevalent as 35% of the mothers got married before 18 years. If this can be controlled the mortality can be reduced further.
Perinatal mortalities in present study among complicated pregnancies were double compared to uncomplicated pregnancies. Pregnancy induced hypertension, anaemia, antepartal haemorrhage were present in the mothers of babies who died.
High Perinatal Mortality Rate of 87 per 1000 live births was noted in mothers who had intrapartal complications compared to 17 per 1000 live births in uncomplicated deliveries. Studies conducted in Bellary [12] and Bijapur [13] reported a very high Perinatal Mortality Rate of 160.8 and 180 per 1000 live births respectively among complicated labours compared to the present study. This huge difference in Perinatal Mortality Rate may be due to the fact that the above mentioned studies were hospital based studies which usually caters to high risk/complicated cases.
High Perinatal Mortality Rate was noted in babies who suffered from intra-uterine complications like growth retardation and meconium aspiration etc. Three out of four babies with complications died during perinatal period. Study by R Kulkarni [14] reported Intra- Uterine Growth Retardation as an important cause of perinatal mortality. Other complications like growth retardation, congenital anomalies foetal distress and meconium aspiration were the causes of deaths in present study.
Three out of 9 preterm babies died in the present study (33.4%). This is similar to the results of studies conducted in Lucknow [15], Ludhiana [16] and Ahmedabad [17] which had reported a Realtive risk of 1.96, 8.2 and 21 respectively. Sachar [18] reported prematurity to be the leading cause of perinatal mortality in their study. Premature babies being more vulnerable to the infections and susceptible to external environmental adversities have higher chances of morbidity and mortality.
Birth asphyxia has been reported as leading cause of perinatal mortality. It accounted for 10.6%, 26% and 26.2% of perinatal mortalities in studies conducted in Maharashtra [14], West Bengal [19] and Orissa [20] respectively. In the present study it had 100% mortality as both the asphyxiated babies died during birth. It accounted for 22% of the perinatal mortalities, which is similar to other studies.
There were 3 twin pregnancies in the present study and in every twin pregnancy one baby died during perinatal period. Singleton pregnancies on the other hand experienced six perinatal deaths out of 308 births thus indicating a higher risk of perinatal death in multiple pregnancies. Study from Maharashtra reported a higher Perinatal Mortality Rate of 105 per 1000 live births among twins than singletons. Study on multiple pregnancies reported a significant increase in Perinatal Mortality Rate with increase in number of foetuses [21].
Conclusion
Prevalence of perinatal mortality in the present study was 28.93 per 1000 live births. Even though this was well below the national and state values indicating improved quality of Maternal and Child Health care, it can be further reduced by ensuring 100% hospital delivery and improving early neonatal care.
Limitations
The present study had been conducted in a limited area (one Primary Health Centre) with lower sample size in order to explore the facts regarding perinatal mortalities at the basic functional unit of health care delivery system. Thus, authors declare that the results of the present study have limited scope for generalization. Authors recommend further studies on this issue covering larger sample size at widespread geographical areas for generalization of results.