Vesiculobullous disorders represent a heterogenous group of dermatoses with protean manifestations. They have remarkable impact on the patient and their family, and have severe economic consequences. The diseases have been the subject of intensive investigation in recent years [1].
Pathologic evaluation of blisters involves systematic analysis, which includes the blister separation plane, the mechanism of blister formation and the character of the inflammatory infiltrate, including its presence or absence [2]. Recent advances in investigative dermatology have created new horizons. The most important techniques for the investigation of patients with vesiculobullous disease are conventional histopathology and confirmative tests like direct and indirect immunofluorescence [1].
Immunofluorescence has greatly contributed to the diagnosis, treatment and understanding of the pathophysiology of vesiculobullous lesions of skin [3]. It is also an important prognostic tool as positive direct immunofluorescence (DIF) findings in patients in remission predict early relapse of disease [4]. Research techniques such as immunoblotting and immunoelectron microscopy may refine the diagnosis in the individual patient. However, these investigations are available only in advanced research laboratories. Even DIF is done only in a few centres in developing countries like India. With the availability of transport media like Michel’s media, majority of dermatologists can have access to DIF. Therefore, this study was undertaken to evaluate the clinical features, histopathology and DIF findings of various vesiculobullous disorders of the skin for their role in diagnosis.
Material and Methods
A cross-sectional, descriptive hospital based study of clinical, histopathological and DIF features of vesiculobullous diseases was conducted on patients attending department of dermatology and pathology of tertiary care hospital over a period of two year.
After obtaining institutional ethical committee clearance and written consent, all the patients attending out-patient department of dermatology were screened for presence of vesiculobullous lesions. In patients with vesiculobullous lesions, detailed history and clinical examination was done with particular reference to age, gender, morphology of lesions, site of involvement and clinical tests such as Nikolsky’s sign and Bulla spread sign. The patients with clinical features suggestive of immunobullous, mechanobullous, severe adverse cutaneous drug reactions or metabolic disorders were included in the study as these disorders show varied clinical manifestations. Histopathology and DIF in these disorders help in the final diagnosis, exclusion of differential diagnosis and determining course of the disease and their response to treatment. Vesiculobullous lesions secondary to infections, eczemas and burns (chemical or thermal) were excluded from the study as these disorders present with characteristic clinical features, and histopathology and DIF are not the main diagnostic methods.
In all the patients, punch biopsy from the lesional skin or oral mucosa preferably including intact vesicle was performed for histopathological study and another biopsy from perilesional normal looking skin or oral mucosa was taken for DIF. Of the two biopsies, one was sent in normal saline or Michel’s medium for DIF and the other in 10% neutral buffered formalin for hematoxylin and eosin staining (H and E).
Histopathological diagnosis was based on level of blister separation, inflammatory infiltrate, altered keratinocytes such as acanthocytes and dyskeratotic cells and pattern of arrangement of keratinocytes e.g. row of tombstone, dilapidated brick wall appearance. Based on these features the vesiculobullous diseases were divided into subcorneal [PF, Pemphigus Erythematosus (PE), Subcorneal pustular dermatosis (SCPD)], intraspinous [toxic epidermal necrosis (TEN), erythema multiforme (EM)], suprabasal (PV, Hailey- Hailey disease) and subepidermal [BP, DH, bullous systemic lupus erythematosis (BSLE)] blistering disorders.
The DIF result was based on site (intercellular, along basement membrane zone or dermal papillae), type (IgG, IgM, IgA or C3), pattern (granular or linear) and intensity of deposition of immune reactants.
Results
During the period of 24 months, 68 biopsy specimens of vesiculobullous lesions of skin were received which constituted 22.08% of all skin biopsies. Majority of patients presented between 40-49 years of age (20 %). Youngest patient was two year old and oldest of 83 years. Female patients were more in number with male: female ratio of 1:1.27.
PV (18/26) and BP (7/11) showed lesions all over the body. Oral mucosal involvement was present in 84.6% (22/26) cases in PV and 18.2% cases in BP. Half the number of patients of PE, PF and BSLE had lesions over the trunk. Involvement of limbs was seen in 18.2% of BP and 100% of IBR cases.
In BP, EB, EM and herpes gestationis (HG) 100% of cases showed vesicle and/or bulla. In PE, SCPD and BSLE 50% of the cases showed vesicles. In PV 76.9% of cases showed vesicles and/or bulla. Nikolsky’s sign and Bulla spread sign was positive in 84.6% and 19.23% of PV patients and 50% and 25% of PF patients respectively.
Clinical provisional diagnosis and histopathological features of different vesiculobullous lesions are shown in [Table/Fig-1,2,3,4,56]. Predominant inflammatory infiltrate consisted of neutrophils in PV. BP showed presence of subepidermal blisters containing eosinophils.
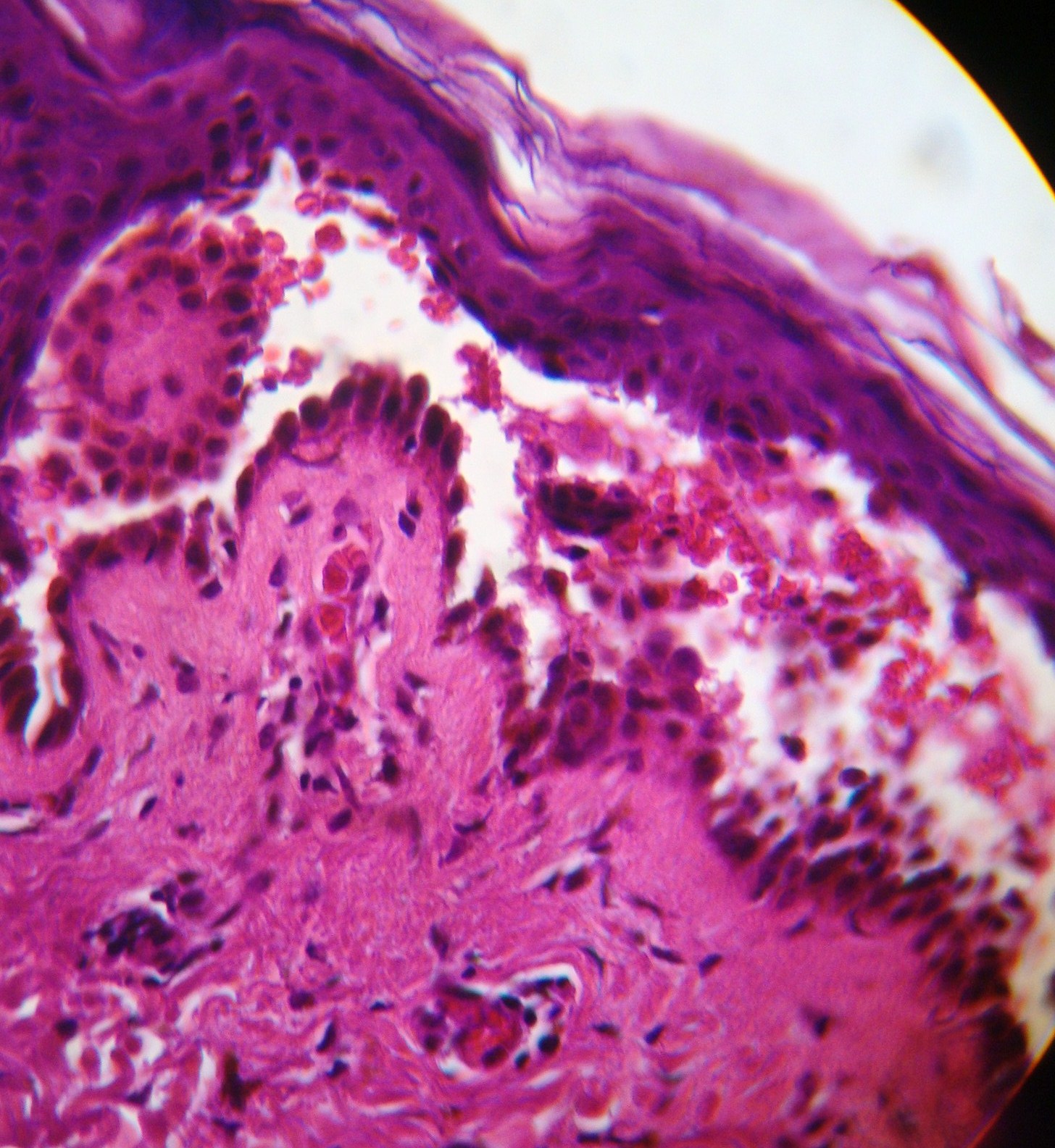
Pemphigus vulgaris. Suprabasal blister, acantholytic cells and tomb stone appearance (H&E, 40X)
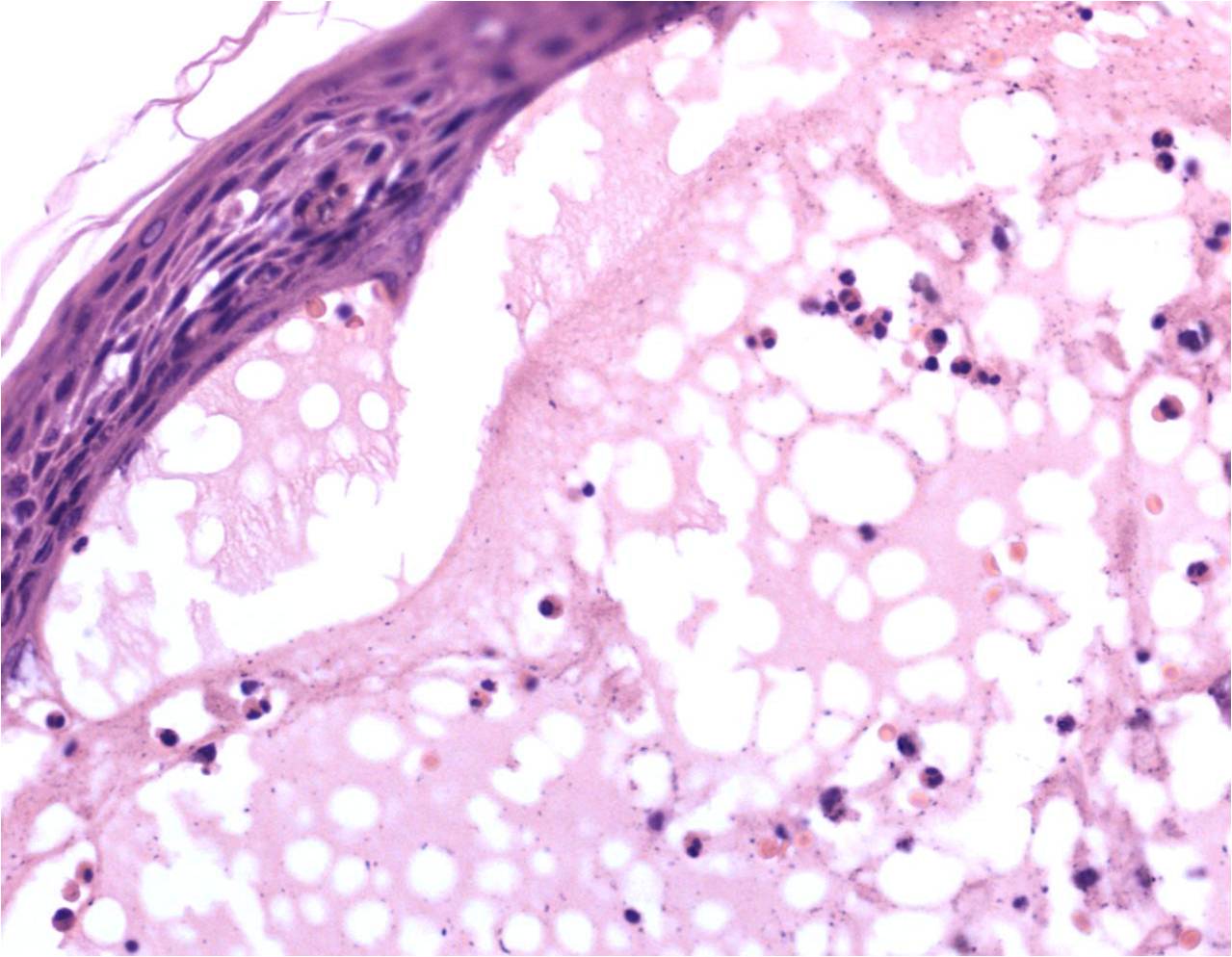
Bullous pemphigoid. Subepidermal bulla filled with eosinophils (H & E, 40X)
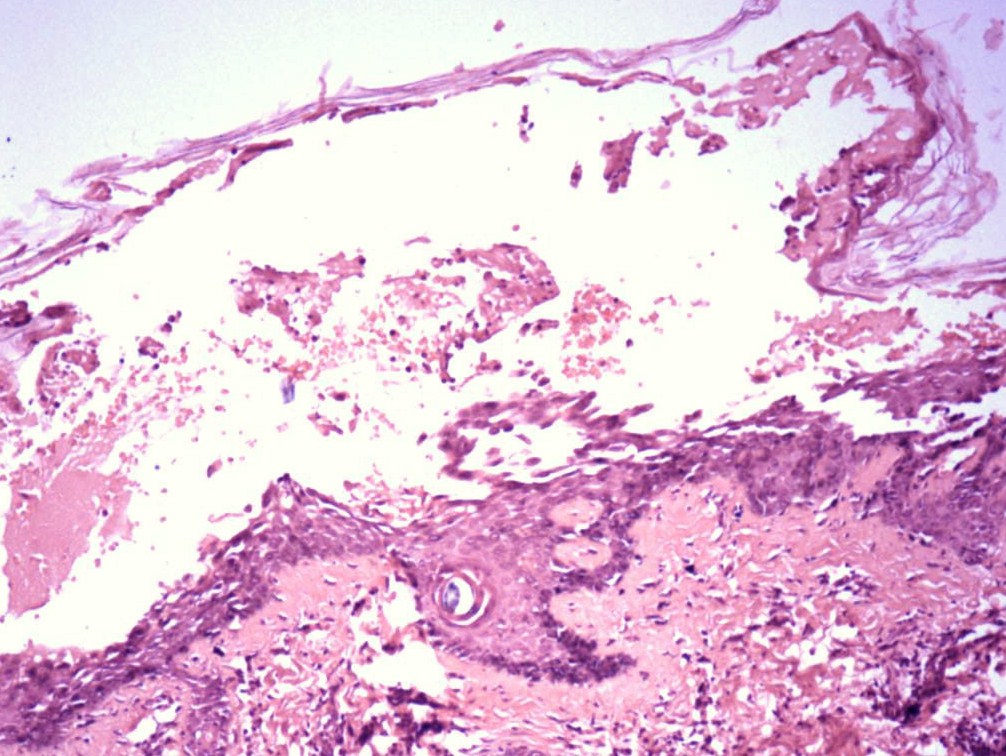
Pemphigus foliaceous. Subcorneal bulla with acanthocytes (H &E, 10X)
Discordance between clinical, histopathological and DIF findings
| Disease | Clinical diagnosis | Histopathological diagnosis | DIF | Final diagnosis# | Percentage (n=68) |
|---|
| Positive | Negative |
|---|
| PV | 36 | 26 | 24 | 2 | 26 | 38.2 |
| PF | 6 | 4 | 3 | 1 | 4 | 05.8 |
| PE | 2 | 1 | 2 | 0 | 2 | 02.9 |
| BP* | 8 | 9 | 9 | 1 | 11 | 16.2 |
| EBA | 2 | 1 | 0 | 1 | 1 | 01.5 |
| Vasculitis | 1 | 0 | 0 | 1 | 0 | 0 |
| DH | 4 | 0 | 0 | 0 | 0 | 0 |
| Darier’s disease± | 1 | 1 | - | - | 1 | 01.5 |
| SJS | 1 | 0 | 0 | 0 | 0 | 0 |
| BSLE | 1 | 2 | 2 | 0 | 2 | 02.9 |
| IBR* | 3 | 2 | 0 | 1 | 2 | 02.9 |
| PCT ± | 1 | 1 | - | - | 1 | 01.5 |
| IgA pemphigus | 1 | 0 | 0 | 0 | 0 | 0 |
| Hailey-Hailey disease | 1 | 1 | 0 | 1 | 1 | 01.5 |
| EM | 0 | 2 | 0 | 2 | 2 | 02.9 |
| Non-specific* | 0 | 12 | 0 | 11 | 12 | 17.7 |
| HG | 0 | 1 | 1 | 0 | 1 | 01.5 |
| SCPD | 0 | 2 | 0 | 2 | 2 | 02.9 |
Note: * - DIF not done in one case; ± - DIF not done, # - final diagnosis based on histopathology and DIF. PV- Pemphigus vulgaris, PF – Pemphigus foliaceus, PE – Pemphigus erythematosus, BP- Bullous pemphigoid, EBA- Epidermolysis bullosa acquisita, DH- Dermatitis herpetiformis, SJS- Steven Johnson syndrome, BSLE- Bullous systemic lupus erythematosus, IBR- Insect bite reaction, PCT – Porphyria cutanea tarda, EM – Erythema multiforme, HG- Herpes gestationis, SCPD- Subcutaneous pustular dermatosis
Level of blister in vesiculobullous disorders
| Final diagnosis | Suprabasal | Subcorneal | Dermoepidermal junction | Intraepidermal | No seperation |
|---|
| PV | 25(96.2%) | 0 | 0 | 0 | 1(3.8%) |
| PF | | 4(100%) | 0 | 0 | 0 |
| PE | 0 | 1(50%) | 0 | 0 | 1(50%) |
| BP | 1(9.1%) | 0 | 8(72.3%) | 1(9.1%) | 1(9.1%) |
| EBA | 0 | 1(100%) | 0 | 0 | 0 |
| EM | 0 | 0 | 1(50%) | 0 | 1(50%) |
| Non Specific | 1(8.3%) | 0 | 1(8.3%) | 2(16.7%) | 8(66.7%) |
| Darier’s | 1(100%) | 0 | 0 | 0 | 0 |
| Herpes Gestationis | 0 | 0 | 1(100%) | 0 | 0 |
| Insect Bite | 0 | 0 | 1(50%) | 1(50%) | 0 |
| PCT | 0 | 0 | 0 | 0 | 1(100%) |
| Hailey- Hailey | 1(100%) | 0 | 0 | 0 | 0 |
| SCPD | 0 | 2(100%) | 0 | 0 | 0 |
| BSLE | 0 | 0 | 2(100%) | 0 | 0 |
Note: PV- Pemphigus vulgaris, PF – Pemphigus foliaceus, PE – Pemphigus erythematosus
BP- Bullous pemphigoid, EBA- Epidermolysis bullosa acquisita, EM – Erythema multiforme
PCT – Porphyria cutanea tarda, SCPD- Subcutaneous pustular dermatosis, BSLE- Bullous systemic lupus erythematosus
Histopathological findings in vesiculobullous disorders
| Final diagnosis | Epidermal changes n(%) |
|---|
| Tomb stone appearance | Villi | Hyperkeratosis | Acanthosis | Dyskeratosis | Acanthocytes |
|---|
| PV | 23(88.5) | 10(38.5) | 2(7.7) | 3(11.5) | 0 | 20(76.9) |
| PF | 0 | 1(25) | 0 | 0 | 1(25) | 3(75) |
| PE | 0 | 0 | 0 | 0 | 0 | 2(100) |
| BP | 0 | 0 | 0 | 0 | 0 | 0 |
| EBA | 0 | 0 | 0 | 0 | 0 | 0 |
| EM | 0 | 0 | 1(50) | 1(50) | 0 | 0 |
| Non-specific | 1(8.3) | 0 | 4(33.3) | 7(58.3) | 0 | 0 |
| Darier’s disease | 0 | 1(100) | 1(100) | 1(100) | 1(100) | 1(100) |
| Herpes Gestationis | 0 | 0 | 0 | 1(100) | 0 | 0 |
| Insect Bite | 0 | 0 | 0 | 1(50) | 0 | 1(50) |
| PCT | 0 | 0 | 1(100) | 1(100) | 0 | 0 |
| Hailey- Hailey disease | 0 | 1(100) | 0 | 0 | 0 | 1(100) |
| SCPD | 0 | 0 | 0 | 1(50) | 0 | 1(50) |
| BSLE | 0 | 0 | 1(50) | 0 | 0 | 0 |
Note: PV- Pemphigus vulgaris, PF – Pemphigus foliaceus, PE – Pemphigus erythematosus, BP- Bullous pemphigoid, EBA- Epidermolysis bullosa acquisita, EM – Erythema multiforme, PCT – Porphyria cutanea tarda, SCPD- Subcutaneous pustular dermatosis, BSLE- Bullous systemic lupus erythematosus
DIF pattern of deposition of immune reactants in different vesiculobullous disorders are shown in [Table/Fig-7,Table/Fig-8 and 9]. Five cases showed discordance between histopathological diagnosis and DIF findings. DIF was negative in all the five cases. In these cases, histopathological findings were diagnostic.
Antibody deposition in direct immunofluorescence
| Final diagnosis | Antibody deposition |
|---|
| IgG | IgM | IgA | C3 | Both IgG and C3 | Negative |
|---|
| PV | 15(57.7%) | 0 | 0 | 0 | 9(34.6%) | 2(7.7%) |
| PF | 2(50%) | 0 | 0 | 0 | 1(25%) | 1(25%) |
| PE | 2(100%) | 0 | 0 | 0 | 0 | 0 |
| BP* | 1(9.1%) | 0 | 0 | 3(27.3%) | 5(45.5%) | 1(9.1%) |
| EBA | 0 | 0 | 0 | 0 | 0 | 1(100%) |
| EM | 0 | 0 | 0 | 0 | 0 | 2(100%) |
| Non-specific * | 0 | 0 | 0 | 0 | 0 | 11(100%) |
| Darier’s ± | 0 | 0 | 0 | 0 | 0 | 0 |
| Herpes Gestationis | 0 | 0 | 0 | 1(100%) | 0 | 0 |
| Insect Bite* | 0 | 0 | 0 | 0 | 0 | 1(100%) |
| PCT ± | 0 | 0 | 0 | 0 | 0 | 0 |
| Hailey- Hailey | 0 | 0 | 0 | 0 | 0 | 1(100%) |
| SCPD | 0 | 0 | 0 | 0 | 0 | 2(100%) |
| BSLE | 0 | 0 | 0 | 1(50%) | 1(50%) | 0 |
Note: *- DIF not done in one case, ±- DIF not done
PV- Pemphigus vulgaris, PF – Pemphigus foliaceus, PE – Pemphigus erythematosus, BP- Bullous pemphigoid, EBA- Epidermolysis bullosa acquisita, EM – Erythema multiforme, PCT – Porphyria cutanea tarda, SCPD- Subcutaneous pustular dermatosis, BSLE- Bullous systemic lupus erythematosus
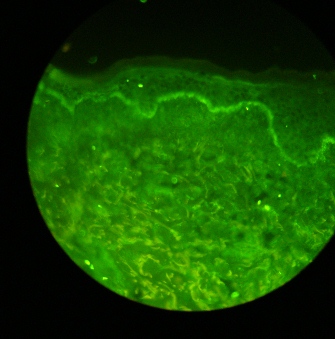
Pemphigus vulgaris. Deposition of IgG in intercellular spaces giving a fish net appearance (DIF, 40X)
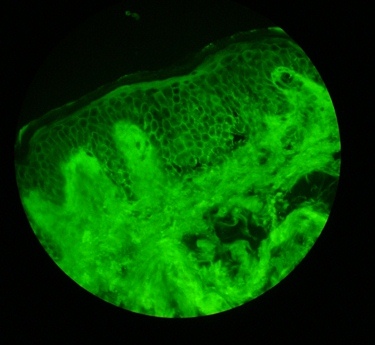
Bullous pemphigoid. Linear deposition of C3 along the basement membrane zone (DIF, 4X)
Discordance between clinical, histopathological and DIF findings were noted [Table/Fig-4 and 10]. Certain disorders like BSLE, SCPD were not part of initial clinical diagnosis. Similarly, all clinically suspected cases of DH were not confirmed either by histopathology or DIF. The final diagnosis was based on histopathology and DIF findings [Table/Fig-4].
Discordance between clinical and final diagnosis
| Clinical diagnosis (n) | Histopathological diagnosis in conjunction with DIF (final diagnosis) |
|---|
| Non specific | BP | PF | SCPD | PV | BSLE | EM | HG |
|---|
| PV (10) | 2 | 3 | 2 | - | - | 1 | 1 | 1 |
| Vasculitis(1) | 1 | - | - | - | - | - | - | - |
| BP (1) | 1 | - | - | - | - | - | - | - |
| DH (4) | 3 | 1 | - | - | - | - | - | - |
| PF (4) | 1 | 0 | - | 2 | 1 | - | - | - |
| EBA (1) | 1 | - | - | - | - | - | - | - |
| SJS (1) | - | - | - | - | - | - | 1 | - |
| Insect bite (1) | 1 | - | - | - | - | - | - | - |
| IgA pemphigus (1) | - | - | - | - | 1 | - | - | - |
Note: PV- Pemphigus vulgaris, BP- Bullous pemphigoid, DH- Dermatitis herpetiformis, PF – Pemphigus foliaceus, EBA- Epidermolysis bullosa acquisita, SJS- Steven Johnson syndrome
Discussion
Though, various primary cutaneous diseases present clinically with vesiculobullous lesions, their etiology, pathogenesis, severity and course differs. Therefore, accurate diagnosis of these diseases is essential for appropriate management to avoid or minimize associated morbidity and mortality.
Clinically, all the patients with vesiculobullous diseases may not present with classical morphology and distribution of the lesions. The number of patients presenting with clinical features like vesicles and bullae, involvement of mucous membranes, Nikolsky’s sign and Bulla spread sign is different in various studies conducted in India [5]. The difference may be due to prevalence of the diseases, severity and stage of the disease at presentation and status of the treatment. Oral mucosa can be only site of involvement in the early stage of pemphigus vulgaris [6] as noted in the present study. In these clinical scenarios where clinical diagnosis is difficult, histopathology and DIF of biopsy specimen will help in arriving at final diagnosis.
All the vesiculobullous diseases show specific histopathological changes which are demonstrated only when early intact vesicle or bulla is included in the biopsy specimen. Similar to clinical features, the number of specimen showing specific histopathological changes is different in various studies conducted in India. In PV, suprabasal separation has been observed in 81.4 [5] - 97% [6], a row of tomb stone appearance was seen in 41.8% [5], acanthocytes in 93 [5]-97% [6], and inflammatory cells in bullous cavity in 53.5 [5]-97% [6] of specimens. In PF, subcorneal separation has been observed in 60% and acanthocytes in 96% of specimen [5]. In BP, subepidermal separation has been observed in 72.3% of specimen which is less compared to study by Nishioka K et al., [7]. These variations may be due to differences in site or type of lesion selected for biopsy. The histopathological changes noted in SCPD and BSLE were consistent with other studies [8,9]. In some cases, the histopathological changes can be non-specific. In the present study, non-specific changes were seen in cases clinically diagnosed as dermatitis herpetiformis and pemphigus vulgaris. In all these patients the clinical presentation was either excoriated papules as in the former or erosions as in the latter. If the histopathological study is non-confirmatory and clinical features strongly suggestive of one of the immunobullous disease, DIF study is recommended.
DIF identifies the deposition of immune reactants like antibodies and complements in the specimen. Hence, DIF is helpful in diagnosis of immunobullous diseases as intraepidermal and subepidermal. DIF positivity has been reported in 100% [10] and 93.28% [11] of PV cases, 100% [4, 10] and 88% [11] of PF cases and 100% [12,13] of cases of BP. As the DIF finding of PF is similar to PV, histopathology helps in differentiating PV from PF. In PE, DIF was helpful as both PE and PF show similar histopathology findings. PE usually shows granular depositions in basement membrane zone (BMZ) along with intercellular deposits in 80% of cases. The final diagnosis of PE was made based on classical malar rash in one case and positive antinuclear antibody titre in other.
In the present study, two cases with clinical and histopathological features of PV showed negative DIF. Selection of biopsy site, treatment status, and technical errors may result in false negativity of DIF. In the absence of these factors, the negative DIF indicates prolonged remission. Negative DIF helps in differentiating SCPD, Hailey-Hailey disease and Darier’s disease from intraepidermal immunobullous diseases. In the present study, negative DIF also helped to exclude DH.
In the present study, discordance between clinical, histopathological and DIF features has been noted [Table/Fig-4 and 10] as these features are affected by duration of the disease, stage of disease at presentation, selection of biopsy site and treatment status. This underlines the importance of considering all these features in combination to arrive at final diagnosis.
Conclusion
Clinical examination is the initial step in making a diagnosis of vesiculobullous disorders. Histopathological examination and DIF are required for making a definitive diagnosis. DIF is helpful in scenarios where clinical and/ or histopathological features are inconclusive. In comparison to DIF, histopathology remains the cornerstone in differentiating PV from PF. Hence, clinical, histopathological and DIF features are considered together to arrive at final diagnosis as these methods may not be diagnostic individually in each and every case.
Note: * - DIF not done in one case; ± - DIF not done, # - final diagnosis based on histopathology and DIF. PV- Pemphigus vulgaris, PF – Pemphigus foliaceus, PE – Pemphigus erythematosus, BP- Bullous pemphigoid, EBA- Epidermolysis bullosa acquisita, DH- Dermatitis herpetiformis, SJS- Steven Johnson syndrome, BSLE- Bullous systemic lupus erythematosus, IBR- Insect bite reaction, PCT – Porphyria cutanea tarda, EM – Erythema multiforme, HG- Herpes gestationis, SCPD- Subcutaneous pustular dermatosis
Note: PV- Pemphigus vulgaris, PF – Pemphigus foliaceus, PE – Pemphigus erythematosus
BP- Bullous pemphigoid, EBA- Epidermolysis bullosa acquisita, EM – Erythema multiforme
PCT – Porphyria cutanea tarda, SCPD- Subcutaneous pustular dermatosis, BSLE- Bullous systemic lupus erythematosus
Note: PV- Pemphigus vulgaris, PF – Pemphigus foliaceus, PE – Pemphigus erythematosus, BP- Bullous pemphigoid, EBA- Epidermolysis bullosa acquisita, EM – Erythema multiforme, PCT – Porphyria cutanea tarda, SCPD- Subcutaneous pustular dermatosis, BSLE- Bullous systemic lupus erythematosus
Note: *- DIF not done in one case, ±- DIF not done
PV- Pemphigus vulgaris, PF – Pemphigus foliaceus, PE – Pemphigus erythematosus, BP- Bullous pemphigoid, EBA- Epidermolysis bullosa acquisita, EM – Erythema multiforme, PCT – Porphyria cutanea tarda, SCPD- Subcutaneous pustular dermatosis, BSLE- Bullous systemic lupus erythematosus
Note: PV- Pemphigus vulgaris, BP- Bullous pemphigoid, DH- Dermatitis herpetiformis, PF – Pemphigus foliaceus, EBA- Epidermolysis bullosa acquisita, SJS- Steven Johnson syndrome