The endometrium is uniquely endowed throughout the female reproductive lifespan with complex regular cycle of periodic proliferation, differentiation, breakdown and regeneration [1]. Menstruation is the cyclic uterine bleeding experienced by almost all women of reproductive age. Normal menstruation is defined as “the bleeding from secretory endometrium associated with an ovulatory cycle, not exceeding a length of five days”. Any bleeding not fulfilling these criteria is referred to as abnormal uterine bleeding [2].
Abnormal uterine bleeding is a very common gynaecological condition that affects all age groups. One third of patients attending gynaecology OPD present with complaints of abnormal uterine bleeding [3]. Bleeding is said to be abnormal when the pattern is irregular, abnormal duration (>7days), or menorrhagia or abnormal amount (>80 ml/menses) [4].
During climacteric, ovarian activity declines. Initially, ovulation fails, no corpus luteum forms, and no progesterone is secreted by the ovary. Therefore the premenopausal menstrual cycles are shortened, often anovulatory and irregular. The irregularity in menstrual cycle during perimenopause can be due to anovulation or to irregular maturation of follicles [5]. The increased risk of endometrial hyperplasia and endometrial carcinoma is more evident in peri-menopausal and post-menopausal women with abnormal uterine bleeding [6]. The varied pattern of endometrial changes attracted our attention in peri-menopausal and post-menopausal age so to study them in detail with the help of available clinical data.
Material and Methods
The prospective histopathological study of 119 cases of endometrium in abnormal uterine bleeding was carried out in the Department of pathology, ACPM Medical College, Dhule, India, over a period of 2 years from July 2010 to August 2012.
The age of patients with abnormal uterine bleeding ranged from 40-65 years. Detailed clinical history like age, menstrual status including dysmenorrhoea, menorrhagia, period & regularity of cycle were obtained. Relevant findings of general, systemic examination were recorded. Inadequate endometrial samples and hysterectomy specimens were excluded from our study.
Endometrial samples were obtained from dilatation and curettage or endometrial biopsy.
Specimens were received in 10% formalin. These were studied grossly and multiple sections were taken from each. The specimens were processed in automated tissue processor. Four to five micron thick paraffin embedded sections were taken and stained by Haematoxylin and Eosin. Histopathological endometrial patterns were studied.
Results
A total of 119 numbers of endometrial samples were received during the study period. Patients were categorized into peri-menopausal (40-49years) and post-menopausal (>50years) age groups. Out of 119 cases, 88 cases were peri-menopausal (40-49years) age group and 31 cases were post-menopausal (>50years) age group. Maximum numbers of patients were in the age group of 40-49 years (73.94%). The commonest symptoms presented were menorrhagia 43(48.86%) followed by metrorrhagia 37(31.55%) and post-menopausal bleeding 31(26.05%). The predominant histopathological finding was proliferative endometrium (30.25%) followed by hyperplastic endometrium (22.68%) in both age groups.
In peri-menopausal age group, the proliferative endometrium was the most common finding observed in 30 cases (34.09%) followed by endometrial hyperplasia in 21cases (23.86%). Out of 21 cases of endometrial hyperplasia simple hyperplasia constitute 17 cases and 4 cases of complex hyperplasia without atypia were observed [Table/Fig-1].
Endometrial pattern in peri-menopausal (40-49 years.) age group
| Histopathological findings | No.of patients (88) | Percentage |
|---|
| Proliferative endometrium | 30 | 34.09 |
| Secretory endometrium | 7 | 7.95 |
| Disordered proliferative | 14 | 15.90 |
| Atrophic endometrium | 2 | 2.27 |
| Irregular shedding | 5 | 13 |
| Endometrium hyperplasia | 21 | 23.86 |
| Endometrial Carcinoma | 0 | 0.0 |
| Endometrial polyp | 3 | 3.40 |
| Chronic endometritis | 5 | 5.68 |
| Tuberculous endometritis | 1 | 1.13 |
In post-menopausal women most frequent finding was atrophic endometrium seen in 8 cases followed by endometrial hyperplasia in six cases. Out of which 4 cases showed complex hyperplasia without atypia and 2 cases showed complex hyperplasia with atypia [Table/Fig-2].
Endometrial pattern in post-menopausal (>50 years)age group
| Histopathological findings | No.of patients (31) | Percentage |
|---|
| Proliferative endometrium | 6 | 19.35 |
| Secretory endometrium | 4 | 12.90 |
| Disordered proliferative | 2 | 6.45 |
| Atrophic endometrium | 8 | 25.80 |
| Irregular shedding | 0 | 0.0 |
| Endometrial hyperplasia | 6 | 19.35 |
| Endometrial Carcinoma | 3 | 9.67 |
| Endometrial polyp | 0 | 0.0 |
| Chronic endometritis | 2 | 6.45 |
| Tuberculous endometritis | 0 | 0.0 |
Discussion
The endometrium is a remarkably dynamic tissue. It undergoes regular cyclical changes in response to the recurrent hormonal changes of the ovulatory cycles [7].
Abnormal uterine bleeding occurring as heavy, prolonged or acyclic flow at menopausal transition or as spotting or minimal bleeding at post-menopausal period may be alarming and needs thorough evaluation, since this may be the only clinical manifestation pointing towards endometrial cancer [8].
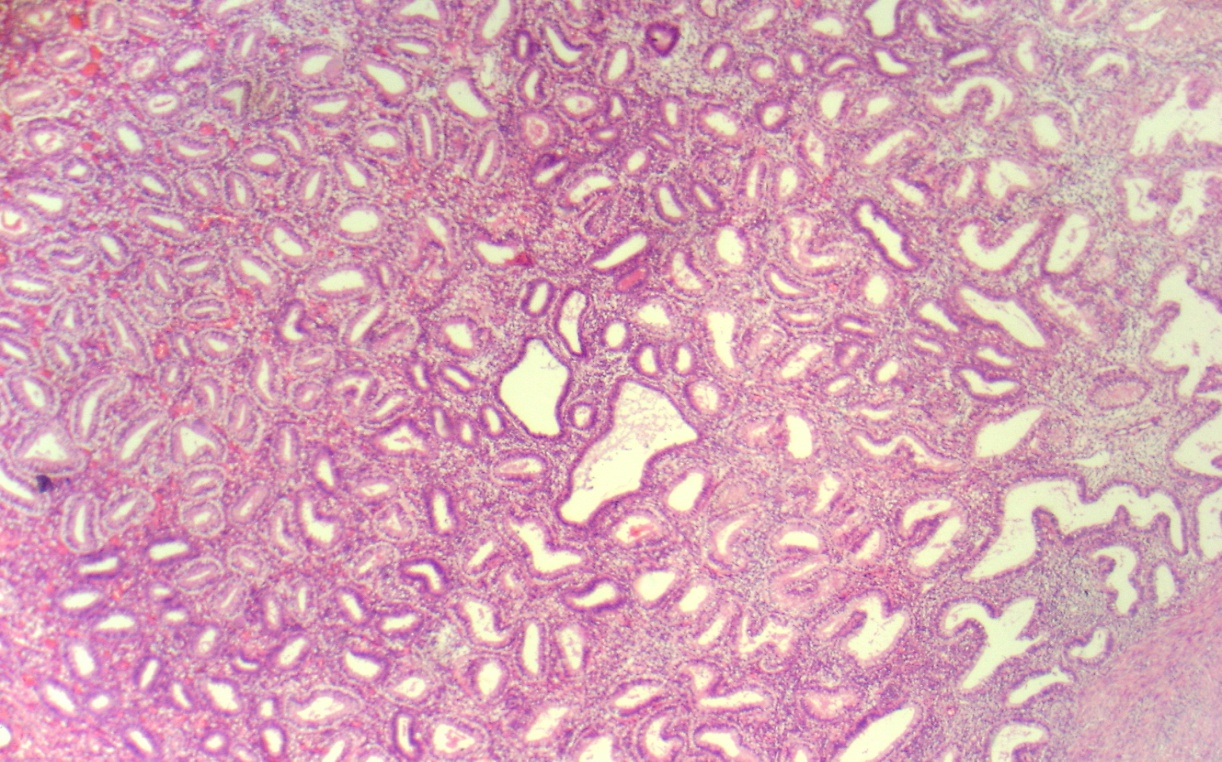
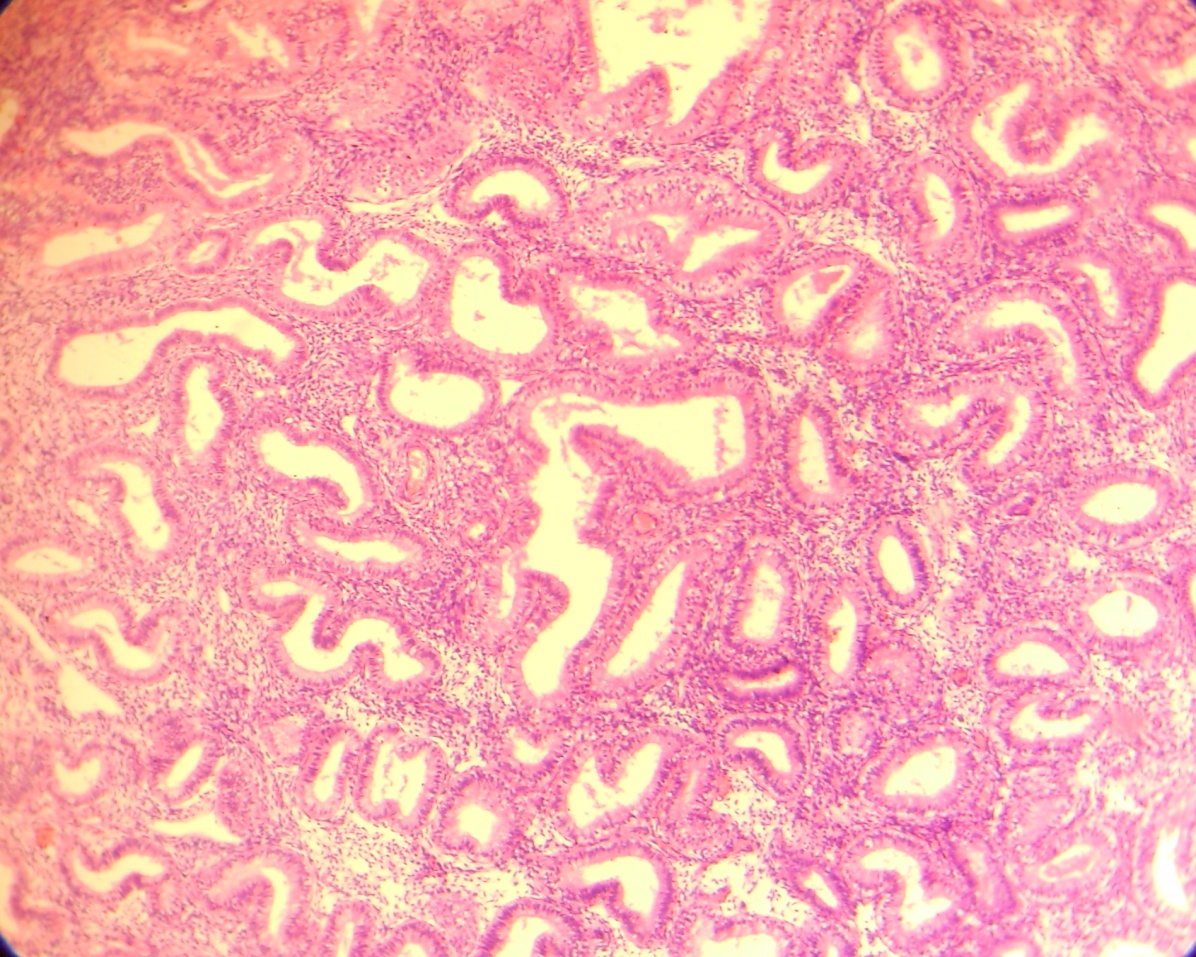
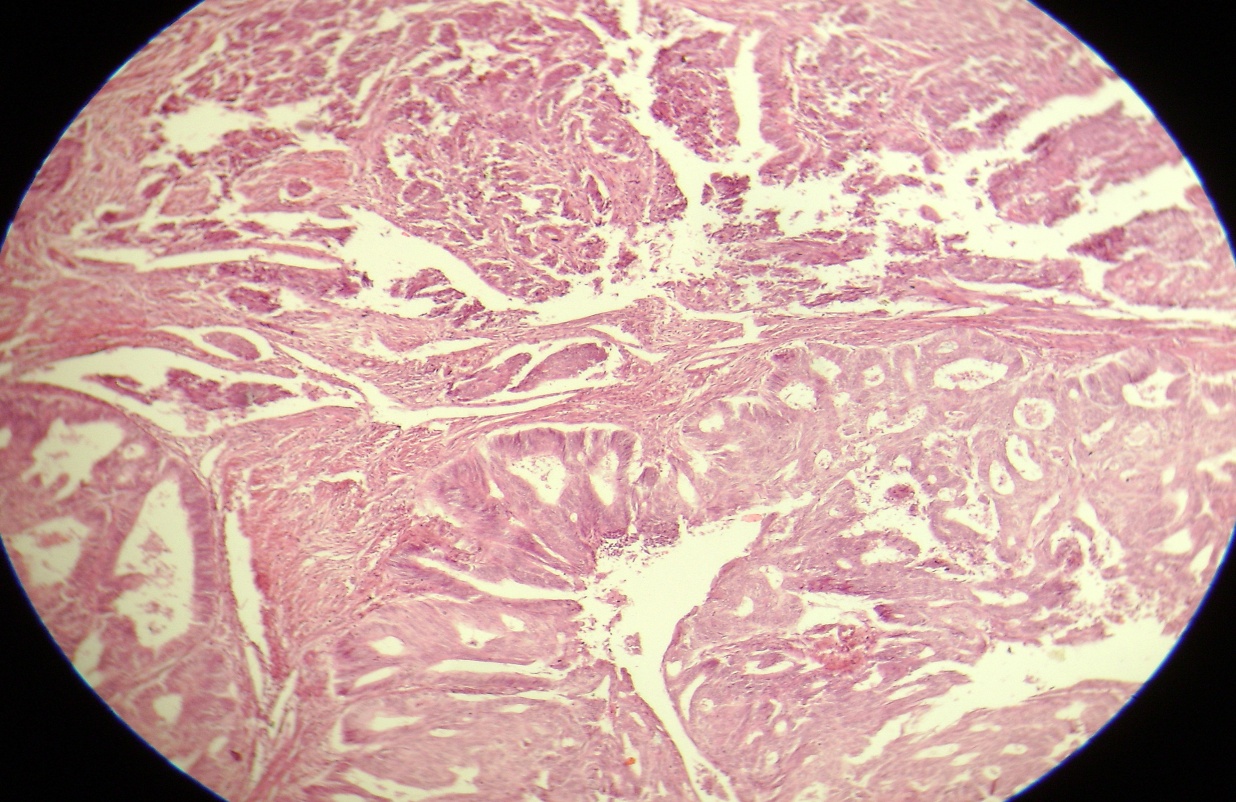
According to WHO the endometrial hyperplasia are classified as simple or complex based on the absence or presence of architectural abnormalities such as glandular complexity and crowding [Table/Fig-3]. Hyperplasia are further designated as atypical if they show nuclear atypia [Table/Fig-4 and 5] [2].
Microphotograph of simple cystic hyperplasia showing few glands are large and cystically dilated and others are normal proliferative glands with compact stroma. (H&E×100)
Microphotograph of complex hyperplasia showing crowded, irregular glands lined by columnar epithelium with back to back arrangement and without nuclear atypia. (H&E×100)
Microphotograph of complex hyperplasia with atypia showing intense crowding of glands lined by stratified epithelium with loss of polarity, reduction in the intervening stroma and show nuclear atypia (H&E×100)
In current study 119 specimens of endometrium (curettage /biopsy) were evaluated to find out age incidence, clinical and pathological features. The incidence of abnormal uterine bleeding was more in peri-menopausal age group than post-menopausal age group. The reason may be due to earlier evaluation and treatment of those patients.
In our study majority of patients were between 40-49 years (73.94%) age group which compared favourably with 89.13% by Sagar S [9] and very much higher than that reported by previous studies [10,11]. The menstrual disorders increases with advancing age. The most common symptoms were menorrhagia (48.86%) followed by post-menopausal bleeding (26.05%). Similar findings were also noted by Sagar S [9], Muzaffar et al., [11] and Samal et al., [12].
In our study of peri-menopausal age group, 35.09 % of proliferative endometrium was observed which is very much in alliance with study done by Dangal G (38.5%) [13]. Khare et al., [14] reported 21.2% while Bhatta S [15] reported 29.16% of proliferative endometrium in peri-menopausal age group. Sagar S [9] and Muzaffar et al., [11] also observed proliferative endometrium in peri-menopausal age which are slightly higher than our study. Bleeding in the proliferative phase may be due to anovulatory cycle in such cases shows progressive rise of estrogen to comparatively high levels, which is then followed by a sudden fall in estrogen due to feedback inhibition of pituitary or of FSH secretion and bleeding results.
In post-menopausal age group we observed 6 cases of proliferative endometrium. Similar results also noted by Bhatta S [15]. Khare et al., [14] noted no case of proliferative endometrium in postmenopausaul age group.
In present study 7.95% of secretory endometrium observed in 40-49 years of age. The incidence was slightly lower when compared with results observed by Sagar S [9] and Bhatta S [15]. Bleeding in the secretory phase is due to ovulatory dysfunction uterine bleeding. This ovulatory bleeding is explained by the inability of the corpus luteum to synthesize adequate amount of progesterone, although it remains active throughout the entire period of 12-14 days. The exact aetiology of ovulatory bleeding can be further clarified by daily serum progesterone assay.
The second most common lesion was endometrial hyperplasia (23.86 %) with maximum age incidence in the age group of 40-49 years which is in concordance with Dangal G (23%) [13] and Slobada L (22.6%) [10]. Khare et al., (36.2%) [14], Doroiswami S et al., (68%) [16] observed high incidence of endometrial hyperplasia in 40-49 years of age group. The incidence of simple endometrial hyperplasia was more common in the 40-49 years age group.
In post-menopausal women we observed only complex hyperplasia without atypia and complex hyperplasia with atypia. Our findings are comparable with Khare et al., [14]. Endometrial hyperplasia is commonly seen in peri-menopausal age due to failure of ovulation. Persistent unriped follicles expose the endometrium to an abnormally excessive and prolonged estrogenic action.
Sixteen cases (15.90%) showed disordered proliferative pattern in our study which is similar to Abdulla LS [17]. It is very difficult to define which is an exaggeration of normal proliferative phase without increasing endometrial volume. A higher incidence of disordered proliferative pattern was observed in our study as compared to Bhatta S [15] in 40-49 years of age.
In our study, we observed 5.58% of cases of irregular shedding of endometrium which is comparable with 6% by Baral R [18] in 40-49 years of age group.
Chronic endometritis was seen in (5.68%) in peri-menopausal group which is similar with the findings of Khare et al., [14] and Abdulla LSl [17] and only 2 cases in post-menopausal group which is in comparable with Bhatta S [15]. We found only single case of tuberculous endometritis in 40-49 years of age which is similar with 0.68% by Sagar [9]. Diagnosis of endometritis depends upon findings of neutrophils in the stroma of a nonmenstruating endometrium in acute endometritis and presence of plasma cells in the stroma in chronic endometritis.
The incidence of endometrial polyp in our study was less as compared to Bhatta S [15]. Tuberculous endometritis and endometrial polyp were not seen in our study in post-menopausal age group.
Atrophic endometrium was seen predominantly in post-menopausal age group due to absence of estrogenic stimulation leading to thin atrophic endometrium susceptible to minor injury [19]. Lidor (45%) [20] and Gredmark (50%) [21] studied that atrophic endometrium was the most common cause of post-menopausal bleeding. We observed 25.80% of atrophic endometrium in postmenopausaul age group in our study.
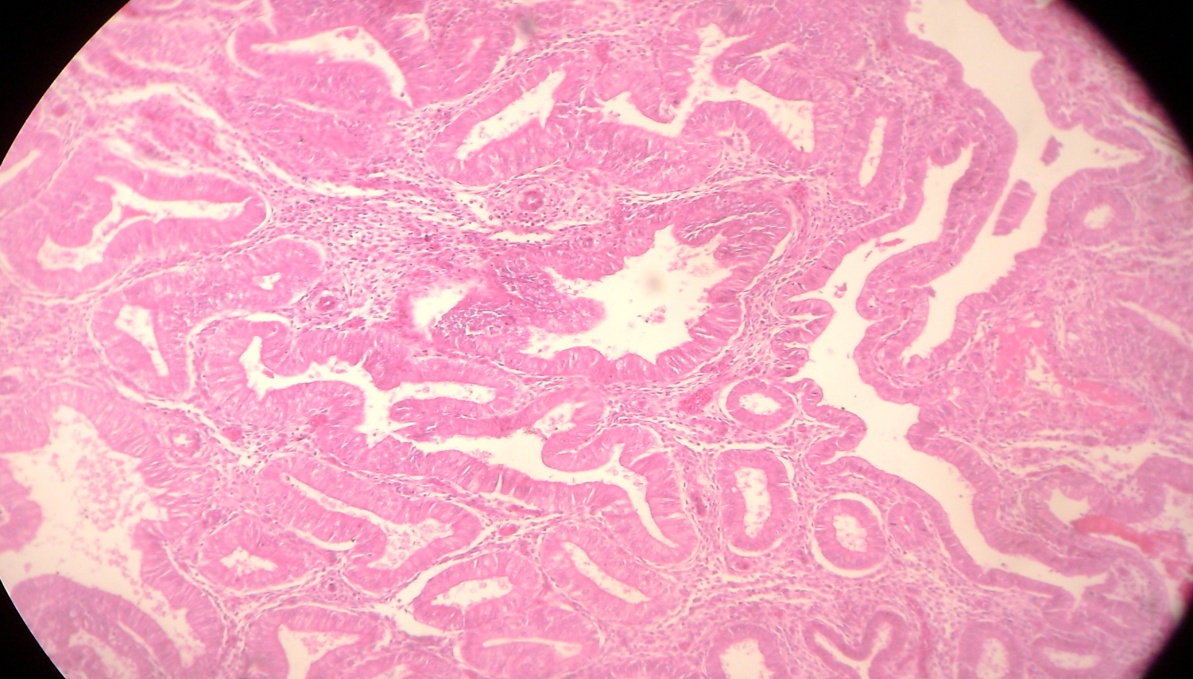
We encountered 3 cases (9.67%) of endometrial carcinoma all were above the age of 50 years [Table/Fig-6]. Similar results were also reported by Dangal G [13] and Khare et al., [14].
Microphotograph of endometrial carcinoma showing less well defined glandular pattern and solid sheets of tumour cells. The cells are more irregular with multilayering and large, pleomorphic nuclei.(H&E×100)
Conclusion
The histopathological study of endometrium in females with abnormal uterine bleeding above the age of 40 years plays an important role in diagnosing various histological patterns and aetiopathological factors. Hence, histopathological examination is mandatory, in cases of peri-menopausal and post-menopausaul abnormal uterine bleeding. It gives bright avenues not only to find out cases in which organic lesions like polyps, hyperplasia can be detected but also helps to search out early atypical hyperplasia and cancer of endometrium which has excellent prognosis if detected early.