Amelogenesis Imperfecta (AI) is a hereditary enamel defect which is characterized by developmental abnormalities in the quantity and/ or quality of enamel. This condition has been associated with dental anomalies, including taurodontism, congenitally missing teeth, delayed eruption, crown resorption, pulpal calcifications and odontogenic fibromas. This paper presents two cases of AI which were associated with multiple impacted permanent teeth in both the cases; and pulpal calcifications and pericoronal odontogenic fibromas of W.H.O type additionally, in one of the cases.
Developmental anomaly, Impacted teeth, Odontogenic fibroma, Pulpal calcifications
Case Report
In case 1, A 16-year-old female patient reported to the dental operatory with chief complaint of small teeth. She also complained of sensitivity and difficulty in chewing food. Detailed family history revealed that her parents had a consanguineous marriage and that she had a normal dentition. However, her elder brother also had a similar problem. Medical history was noncontributory and she did not report any major illness or prolonged hospitalization and medication. General physical examination revealed no abnormality. Intraoral soft tissue examination showed slight generalized gingival inflammation, presumably caused by plaque and calculus deposits. Hard tissue examination revealed retained 52, 53, 63, 73, 83, 84 and 85, with skeletal crossbite [Table/Fig-1]. Teeth showed a generalized yellowish discolouration, with smooth surfaces. The posterior teeth showed severe attrition, exposing the dentine, which appeared to be normal [Table/Fig-2]. A provisional diagnosis of AI was given. A panoramic radiograph revealed impacted 13, 23, 27, 33, 43, 44, and 45. Enamel was thinned out/ completely absent on the crown surface of all the teeth and wherever it was present, it showed a distinction from underlying dentine [Table/Fig-3]. Depending on the clinical and radiographic findings, it was finally diagnosed as a hypoplastic type of AI.
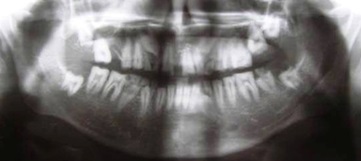
In case 2, a 17-year-old boy who was a sibling of case 1, showed retained deciduous canines and molars, missing permanent teeth and a generalized gingival enlargement [Table/Fig-4]. There was a generalized yellowish to brown discolouration of the teeth, with open contact points [Table/Fig-5]. The condition was provisionally diagnosed as AI. A radiographic examination showed that 19 permanent teeth which were not visible clinically were impacted. The maxillary impacted teeth were at the level of the maxillary sinus and the mandibular teeth were at the level of the inferior border. Above all, an interesting finding was that each impacted tooth had a pericoronal radiolucent zone which was greater than 2mm, which was delineated by a sclerotic border and the presence of free pulpal calcifications in the teeth [Table/Fig-6].
A differential diagnosis of hyperplastic follicles, dentigerous cysts and odontogenic keratocyst was given for the pericoronal radiolucent zone, based on its radiographic appearance.
No abnormal values were noticed in routine pre-operative haematological investigations and in serum calcium and alkaline phosphatase levels. To evaluate the nature of the pathology in relation to the pericoronal radiolucency, an incisinal biopsy was made by making a window in the buccal cortical plate in relation to 13, as it was more accessible, leaving the tooth intact under local anaesthesia.
Histopathological examination of the excised tissue showed mature fibrocollagenous stroma, strands of odontogenic epithelium and few areas of calcification, which confirmed the diagnosis of an odontogenic fibroma (W.H.O type) [Table/Fig-7]. Based on the clinical and radiographic findings, it was finally diagnosed as a hypoplastic type of AI which was associated with a variety of non- enamel manifestations.
In both the cases, aesthetics, phonetics and mastication were the aspects of concern for the patients. In case I, encouraging proper oral hygiene practice; extraction of over retained primary teeth and 37; use of stainless steel crowns for restoring the vertical dimension in relation to 26, 36, 46; replacing missing teeth with removable partial dentures; providing palliative treatment for sensitivity (use of desensitizing pastes) and an orthodontic opinion were planned. In case II, along with the thorough oral hygiene measures, extraction of mobile primary teeth and 36 was advocated. To improve the functional ability, removable partial dentures were planned in relation to the impacted /missing teeth. As none of the impacted teeth were symptomatic a conservative approach (not to extract) was planned. However, the patient was kept under follow up, to evaluate any pathological changes which were associated with impacted teeth.
Hypoplastic teeth with anterior cross bite


OPG revealing impacted permanent teeth
Hypoplastic teeth with anterior cross bite and inflammatory gingival enlargement


OPG showing multiple impacted teeth with pericoronal radiolucencies

Photomicrograph of a pericoronal lesion showing features of an odontogenic fibroma (W.H.O type)

Discussion
AI is a developmental condition of the dental enamel that shows autosomal dominant, autosomal recessive and sex linked inheritance patterns and sporadic cases. Based on enamel appearance and hypothesized developmental defects, AI is classified into four patterns: hypoplastic, hypomaturation, hypocalcified, and hypomaturation-hypoplastic [1]. Dental features which are associated with AI include qualitatively and quantitatively deficient enamel. It is also associated as a spectrum of other features such as progressive root and crown resorptions, pulpal calcifications, taurodontism, malformations of root, impaction of permanent teeth and congenitally missing teeth [2].
Multiple impacted teeth may be related to various syndromes and metabolic disorders like Cleidocranial dysostosis, Gardner’s syndrome and Mucopolysaccharidosis. However, local factors like lack of space, crowded dental arches, premature loss of primary teeth with subsequent space closure, rotation of tooth buds and lack of eruptive forces, may lead to this condition. In the present case, presence of any syndrome or a metabolic disorder was ruled out by doing physical and medical examinations of the patients. Failure of multiple permanent teeth to erupt into the oral cavity has been described in several cases of AI [2-4].
Odontogenic fibroma is a rare and most controversial of all odontogenic tumours. It consists of fibrous connective tissue with varying amounts of odontogenic epithelium and it may contain foci of dysplastic dentine and a material which resembles cementum. Gardner calls this lesion, the “Central Odontogenic Fibroma” (W.H.O type) [5]. They are found to be associated with the crowns of impacted teeth and it is considered that they prevent normal eruption. Similar findings were reported in this case.
Pulpal calcifications are often visible on radiographs. They are classified as true or false denticles according to their microscopic structures. The true denticles were further subdivided into free or attached types, depending on their attachment to the wall of the pulp chamber [6]. In patients with certain systemic/genetic diseases, the pulp chamber calcifications are occasionally found throughout the dentition. But in this case, there were no systemic and local disorders that could be related to their occurrence.
In a study which was conducted on “Dental anomalies associated with AI” by Collins MA et al., showed an increased incidence of impacted permanent teeth, taurodontism, pulpal calcifications and odontogenic fibromas [7].
The co-segregation of hypoplastic enamel, pulpal calcifications, failure of dental eruption and odontogenic fibromas strongly suggests that the mutation which had caused the AI type may not have only involved a gene expressed in ameloblasts but which may have been expressed in other odontogenic tissues also. The clinical presentation of AI depends on the specific gene involved and the type of mutation. Over 25 different AI associated mutations have been identified, but mutations in four main genes-amelogenin (AMELX), enamelin (ENAM), kallikrein4 (KLK4) and enamelysin (MMP-20) have been reported to be involved in AI till date. Most of the X-linked hypoplastic AI cases are said to be caused by mutations in the AMELX gene which encode for the amelogenin protein. Because of the merging mode of inheritance and genetic heterogenecity of AI, it still remains to be understood and determined as to whether these features had occurred as a direct consequence of the molecular defect (d1), that had caused enamel malformation or as a result of unknown secondary factors [8].
An interdisciplinary approach is necessary to evaluate, diagnose and resolve the problems which are associated with AI by using a combination of orthodontic, periodontal, prosthodontic and restorative treatments.
Conclusion
As dental anomalies are common in daily practice, a thorough knowledge on the aetiology and associated non enamel dental anomalies will help clinicians in effectively managing these sorts of conditions.
[1]. EM Canger, P Celenk, M Yenisey, SZ Odyakmaz, Amelogenesis Imperfecta, Hypoplastic type associated with some dental abnormalities: A case report.Braz Dent J. 2010 21:170-4. [Google Scholar]
[2]. S Hegde, Multiple unerupted teeth with Amelogenesis Imperfecta in siblingsN Am J Med Sci 2012 4:235-7. [Google Scholar]
[3]. WK Seow, Dental development in amelogenesis imperfecta: A case controlled studyPediatr Dent 1995 17:26-30. [Google Scholar]
[4]. H Lehmann, Amelogenesis imperfecta - a case with multiple retentions.Tandlaegebladet 1979 83:38-42. [Google Scholar]
[5]. HJ Sandler, RR Nersasian, E Cataldo, S Pochebit, Y Dayal, Multiple dental follicles with odontogenic fibroma-like changes (WHO type).Oral Surg Oral Med Oral Pathol. 1988 66:78-84. [Google Scholar]
[6]. R Rajendran, Sivapathasundharam Shafer’s textbook of oral pathology 2009 578NoidaElsevier [Google Scholar]
[7]. MA Collins, SM Mauriello, DA Tyndall, JT Wright, Dental anomalies associated with amelogenesis imperfecta- A radiographic assessmentOral Surg Oral Med Oral Pathol Oral Radiol Endod 1999 8:358-64. [Google Scholar]
[8]. JT Wright, The Molecular Etiologies and Associated Phenotypes of Amelogenesis Imperfecta.Am J Med Genet A 2006 140:2547-55. [Google Scholar]