Acute Retention of Urine, Tubercular Prostatitis: A Rare Case
Prasad Mylarappa1, H.C. Srikantaiah2
1 Faculty, Department of Urology, M.S. Ramaiah Medical College, Bangalore-54, India.
2 Faculty, Department of General Surgery, M.S. Ramaiah Medical College, Bangalore-54, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. H.C. Srikantaiah, Faculty, Department of General Surgery, M.S. Ramaiah Medical College, Bangalore-54, India.
Phone: 9845208352,
E-mail: drsrikantaiah@gmail.com
Prostate tuberculosis is a very rare condition and only few isolated cases have been reported in the literature in immunocompetent individuals. We, report a case of a 58-year-old man, who presented to us with features of lower urinary tract symptoms. On evaluation, prostatomegaly was found which was treated conservatively. Due to failed conservative treatment, transuretheral resection of prostate was performed. Histopathological examination along with Polymerase chain reaction and Ziehl-Neelsen staining confirmed tubercular prostatitis. He received nine months course of antitubercular treatment with good response.
Tuberculosis, Pyelonephritis, Prostate
Case Report
A 58-year-old male presented to our hospital with history of right flank pain, fever and lower urinary tract symptoms (increased frequency, dysuria, nocturia and difficulty in voiding). On physical examination, he had mild right flank tenderness with grade-2 enlargement of the prostate.
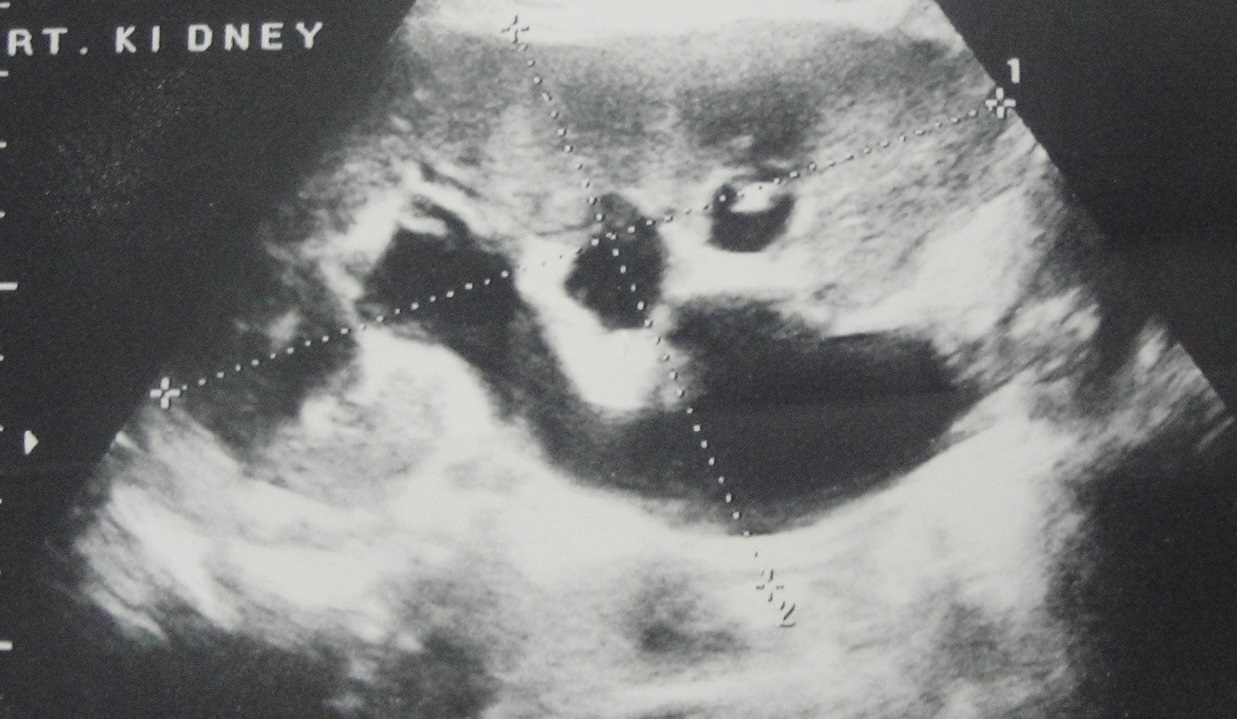
Urine analysis showed plenty of pus cells and culture grew E.coli. Blood examination revealed leucocytes with neutrophilia and raised ESR. Urine cytology and AFB smear were negative. Blood urea, Serum creatinine, Serum prostate-specific antigen and chest x-ray were normal. Ultrasonography of abdomen and KUB region revealed hypo echoic bulky right kidney with hydronephrosis and moderate enlargement of prostate with significant post void urine [Table/Fig-1a,1b]. CT-KUB region showed features suggestive of acute pyelonephritis of right kidney with prostatomegaly [Table/Fig-2]. Uroflowmetry findings were consistent with obstructive voiding pattern with peak flow of 6ml/sec.
Ultrasonography picture showing hydronephrotic changes
Ultrasonography showing prostate enlargement

CT-KUB showing prostate enlargement

He was treated conservatively with a course of antibiotics and α-blockers. After six months, in spite of being on alpha blockers, he presented to our urological services with history of acute retention of urine. He had grossly distended bladder and grade-2 prostatomegaly. Repeat ultrasonography revealed prostatomegaly with over distended bladder with mild bilateral hydroureteronephrosis. Bladder decompression was done by continuous indwelling catheter. After pre-operative optimization, he underwent transurethral resection of prostate for prostatomegaly. Histopathological examination showed features suggestive of granulomatous prostatitis [Table/Fig-3]. Polymerase chain reaction and Ziehl Neelsen staining of the prostate specimen identified M.tuberculosis. After confirmation of diagnosis, he was treated with 9 months course of antitubercular treatment. At 3 months follow-up urine was negative for pus cells and bacteria. His urine AFB smear was negative and uroflowmetry showed peak flow of 22ml/sec.

Discussion
Robert Koch discovered M. tuberculosis in the year 1882 and he succeeded in transmitting the disease to other animals which were found to be susceptible hosts [1]. In 1937, Wildbolz first described the lesion “Genitourinary tuberculosis” to demonstrate that it was a local manifestation of a systemic disease. Changing patterns of population migration and the development of large pools of immunocompromised individuals has increased the trend of tuberculosis [2]. Today, Extrapulmonary tuberculosis is becoming common specially involving the urogenital tract.
Genitourinary tuberculosis has been reported to constitute 10-14% of the Extrapulmonary tuberculosis with involvement of any part of the kidney to the urethra [3]. Extrapulmonary tuberculosis has been reported to be steadily increasing in patients with AIDS. Predisposing factors associated with development of extrapulmonary tuberculosis include immunocompromised status, immunosuppressive therapy, prolonged steroid use and diseases with poor immune mechanism. Isolated tubercular prostatitis cases is uncommon especially in immunocompetent patients. In our case, patient was immunocompetent and no other predisposing factors apart from pyelonephritis were found. Mycobacterium tuberculosis is the most common pathogen involved but others such as, M. kansasii or fortuitum have been described.
In the genitourinary tract, kidney and prostate are the commonly affected organs by tuberculosis, as the primary site is often asymptomatic. The possible mode of spread to genitourinary organs is by hematogenous route from the lungs. Other organs can get involved either by ascending infection from the prostate to the bladder or descending infection from the kidney to the bladder or prostate to epididymis. The lesion may get involved by direct extension from the epididymis. Tuberculosis of the prostate is usually secondary to tuberculous infection of the upper urinary tract but it can occur primarily or secondary to tuberculosis infection of the epididymis or seminal vesicle.
Tubercular prostatitis usually is asymptomatic, except when it involves the epididymis and in acute cases, when it evolves into perianal abscess. It can also present with features of lower urinary tract symptoms and retention of urine, as in our case. Tubercular prostate can be normal on digital rectal examination or can present with localized nodule with normal or raised serum prostate specific antigen. Our patient had presented with features of lower urinary tract symptoms and acute pyelonephritis, initially digital rectal examination was normal with normal serum prostate-specific antigen level but urine culture grew E. coli which was treated with a course of culture specific antibiotic (E. coli was sensitive to ceftriaxone). He also received α–blocker for the enlarged prostate with significant post void residue. In spite of α–blockers for six months he had developed retention of urine and hence, transurethral resection of prostate was considered [4].
Transrectal ultrasonography is a well-established imaging technique for evaluation of prostate and for diagnosis of carcinoma when combined with biopsy, but both granulomatous prostatitis and carcinoma can produce similar findings on transrectal ultrasonography. In our case, transrectal ultrasonography was done.
Histopathological prostatatic tuberculosis can exhibit diffuse caseating epitheloid cell granulomas or focal caseating necrosis with calcification, which are not confined to the periglandular or periductal region, as seen in cases of non-specific granulomatous prostatitis. Causes of granulomatous prostatitis include treponema pallidum, viruses, various fungi and intra-vesical BCG. One needs to differentiate non-specific granulomatous prostatitis as this type is self limiting benign condition, while the latter requires specific treatment [5]. In our case, histopathological examination revealed features suggestive of granulomatous inflammation of the prostate [Table/Fig-3]. Polymerase chain reaction and Ziehl-Neelsen staining of the specimen were positive for mycobacterium tuberculosis. After confirmation of diagnosis, he received nine months course of anti tubercular treatment with good recovery.
Conclusion
Tubercular prostatitis is a very rare condition and it can present with varied clinical features including lower urinary tract symptoms and benign prostatic hypertrophy with retention of urine. It is usually found incidentally following histopathological examination of prostate. A high index of suspicion helps in early diagnosis and avoids unnecessary surgery in case of benign prostatic hypertrophy with tubercular prostatitis.
[1]. Kostakopoulos A, Economou G, Picramenos D, Macrichoritis C, Tekerlekis P, Kalliakmanis N, Tuberculosis of the prostateIntUrolNephrol 1998 30:153-7. [Google Scholar]
[2]. Wise Gilbert J, Venkata K, Genitourinary manifestations of tuberculosisUrologic Clinics of North America 03/2003 30(1):111-21. [Google Scholar]
[3]. Colabawalla BB, Reflections on urogenital tuberculosisIndian J Urol 1990 6:51-9. [Google Scholar]
[4]. Tanagho EA, McAninch JW, Smith’s general urology 2000 15th EdMc grawhill publication:265-71. [Google Scholar]
[5]. O’dea MJ, Non specific granulomatous prostatitisJ Urology July 1997 118:58-60. [Google Scholar]