Ischaemic Fasciitis: A Very Rare Entity with Unusual Presentation
Jyotsna Wader1, Neha Gajbi2, Sujata Kumbhar3
1 Associate Professor, Department of Pathology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
2 PG Resident, Department of Pathology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
3 Assistant Professor, Department of Pathology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Neha Gajbi, Department of Pathology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
Phone: 9404215297,
E-mail: dr.komalgajbi@gmail.com
We are reporting a case of ischaemic fasciitis which occurred in a 55-year-old female with no debilitating or long bed ridden history. She presented with a large swelling over left gluteal region. On evaluation, swelling was found to be of size, 5x5 cm, slightly tender and with induration. The operative findings led to a probable diagnosis of a calcified lesion, due to its hard consistency. However, the microscopic picture was typical of ischaemic fasciitis, because of its characteristic central necrosis, vascular and atypical fibroblastic proliferations. Also seen was presence of foreign body giant cell reactions, inflammatory cells and extravasated RBCs. Ischaemic fasciitis is a very rare pseudo sarcomatous proliferation of atypical fibroblasts, which has been described to be located over bony protuberances and said to develop most often in immobile elderly or debilitated patients. Recognition of this distinct entity as a reactive process, mostly associated with debilitation is rare in occurrence.
Ischaemic fasciitis, Atypical fibroblast
Introduction
Ischemic fasciitis is a type of reactive, nonneoplastic, reparative or regenerative response to some sort of ischemia typically seen in older debilitated patients at pressure points [1].
It belongs to a group of pseudosarcomatous lesions that include nodular fasciitis, proliferative fasciitis and proliferative myositis [1].
These soft tissue lesions are fascia-based fibroblastic and myofibroblastic proliferation and as this lesion simulates soft-tissue sarcoma, either clinically, cytologically or even histologically, it is important to recognize and limit overdiagnosis of sarcoma [2].
Case Report
A case of 55-year-old female with no debilitating or long bed ridden history. There is history of hospitality with bed rest for 8 days, three months back. She presented with a large swelling over left gluteal region. On evaluation swelling was 5x5 cm, mobile, slightly tender and with induration. No history of ulceration or discharge, no local rise of temperature was present.
Excision specimen consisted of an irregular mass with brown yellow, soft to hard tissue measuring 5x5x3 cm and cut section revealed grey white lobular appearance with chalky white dots. So, the operative findings led to a probable diagnosis of calcified lesion due to its hard consistency.
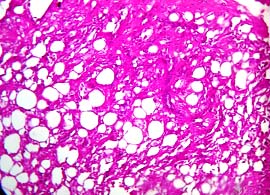
The microscopic examination was typical of Ischemic fasciitis by its characteristic lesion with irregular outlines showing central necrosis, vascular and atypical fibroblastic proliferation, also seen is the presence of foreign body giant cell reaction, inflammatory cells predominantly lymphocytes with few polymorphs and extravasated RBCs.
Ischemic fasciitis can be mistaken clinically, cytologically and histologically for sarcoma. The histological findings seen in this case, when combined with the clinical history, were sufficient to avoid misdiagnosis of malignancy in a benign, proliferative lesion.
Gross photograph of external surface of tissue

Gross photograph of cut surface of the tissue

H & E stain (400x) - central necrosis, atypical fibroblastic proliferation, foreign body giant cell reaction, inflammatory cells
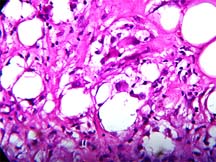
H & E stain (400x) – irregular outlines with central fibrinoid necrosis surrounded by granulation tissue , fibrin and atypical fibroblastic component
Discussion
Decubital ischemic fasciitis was first described as “atypical decubital fibroplasia” in 1992 by Montgomery et al., [3]. And is recently described as a distinctive fibroblastic proliferation occurring predominantly in elderly, bed-ridden individuals and is very rare in occurrence [4].
In ischemic fasciitis, females tend to be more affected than males. Eighth and ninth decades of life are the peak age. However, younger age groups have also been reported [1].
Ischemic fasciitis has been reported in the deep dermis and subcutaneous tissue of pressure areas.
The etiology - of most pseudosarcomatous soft tissue lesions is unknown but a preceding trauma is the most accepted offending agent. There may be different types of trauma: history of catheterization is considered as the etiology for ossifying fasciitis and birth trauma for cranial fasciitis.
The reported pathogenesis for ischemic fasciitis is related to intermittent ischemia that leads to tissue necrosis and breakdown followed by regenerative and reparative process. This explains the characteristic location of ischemic fasciitis in close opposition to bone, in addition to its origin in debilitated or immobilized patients.
Short history of bed rest in the recent past probably causes trauma and aggravated the event. This may be the predisposing fact in our case as the lesion was in the gluteal region but the patient was neither debilitated nor immobilized for a long duration. A site of axillary fold with no history of debilitation is quoted in one past report.
Conclusion
It is a rare soft-tissue tumor sarcoma simulator. Clinically and also histologically, ischemic fasciitis can mimic a soft tissue sarcoma and therefore, it is important to recognize this lesion as a pseudosarcomatous proliferation of fibroblasts. The morphologically distinctive zonal appearance with central fibrinoid necrosis surrounded by granulation tissue like vascular proliferation mixed with the proliferative fasciitis like fibroblastic component is the hallmark of ischemic fasciitis.
In addition, the presence of infarcted fat, fat necrosis, extravasated RBCs, hemosiderin deposition, myxoid changes, and an inflammatory infiltrate in variable amounts are helpful in recognizing this lesion as a reactive proliferation instead of a sarcoma.
Pathologists should be aware that immobility or debilitation is most significant finding in ischemic fasciitis but not always the long duration history of immobility is present as in our case which is unsual presentation. A subset of these lesions can occur in younger patients and infiltration of skeletal muscle and tendinous tissue as well as entirely intramuscular development can be seen.
[1]. Liegl B, Ischemic fasciitis: analysis of 44 cases indicating an inconsistent association with immobility or debilitation, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA 02115, USAAm J Surg Pathol 2008 Oct 32(10):1546-52. [Google Scholar]
[2]. Daoudi A, Amarti A, Bennis S, Boutayeb F, Znati K, Chbani L, Elfatemi H; Ischemic fasciitis - A case report, Ann Chir Plast Esthet. 54 4 392-5. Source:http://linkedlifedata.com/resource/pubmed/id/19223110 [Google Scholar]
[3]. Montgomery EA, Meis JM, Mitchell MS, Enzinger FM, Atypical decubital fibroplasias. A distinctive fibroplastic pseudotumor occurring in debilitated patientsAm J Surg Pathol 1992 16:708-15.[Pubmed] [Google Scholar]
[4]. Bernadette Liegl, Christopher D. M. Fletcher, Ischemic Fasciitis: Analysis of 44 Cases Indicating an Inconsistent Association With Immobility or DebilitationAm J Surg Pathol 2008 32:1546-52. [Google Scholar]