Microsurgical Aesthetic Treatment of Gingival Fenestration by a Coronally Repositioned Partial Thickness Graft: A Case Report
Punit Vaibhav Patel1, Naresh Kumar2, Farhan Durrani3
1 Faculty of Dental Sciences, Institute of Medical Sciences, Banaras Hindu University (B.H.U.), Varanasi,-05, U.P., India.
2 Faculty of Dental Sciences, Institute of Medical Sciences, Banaras Hindu University (B.H.U.), Varanasi,-05, U.P., India.
3 Faculty of Dental Sciences, Institute of Medical Sciences, Banaras Hindu University (B.H.U.), Varanasi,-05, U.P., India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Punit Vaibhav Patel, Faculty of Dental Sciences, Institute of Medical Sciences, Banaras Hindu University (B.H.U.), Varanasi,-05, U.P., India.
Phone: 91-7275832787,
E-mail: punitvai@gmail.com
Gingival fenestration is a rare pathological entity, scarcely described in the literature. The present paper has reported a case of a 22-year-old male patient with a “Gingival fenestration” in the lower left central incisor. The lesion was successfully treated using a coronally positioned partial thickness graft under 4 X magnification, with excellent aesthetic results.
Gingival Fenestration, Periodontal plastic surgery, Periodontal microsurgery
Introduction
Gingival fenestration is an opening through oral keratinized tissue, usually unattached, that is observed in thin gingiva, with usually thick subgingival calculus deposits. This lesion is seen infrequently, but may be more common than has been reported; lack of symptoms may inhibit patient awareness. Because surgical correction is not usually required, there are very few reports in the literature concerning this lesion [1]. The following report has described a unique case of gingival fenestration and its surgical treatment with a coronally positioned partial thickness graft under 4 X magnification, with excellent aesthetic results.
Case Report
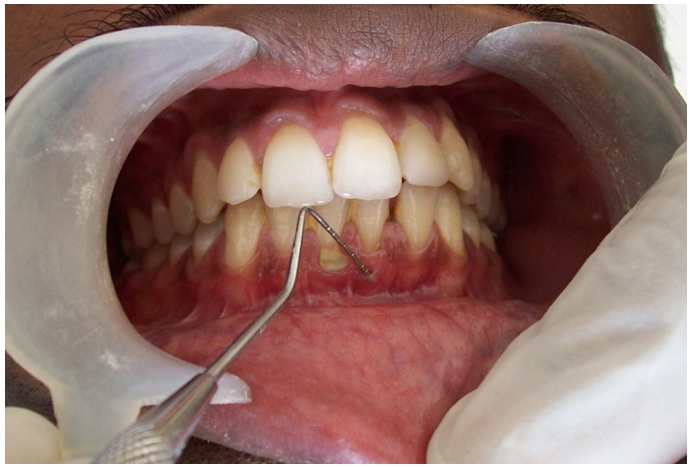
A 22-year-old male patient reported to the Department of Dental Surgery, with chief complaints of sensitivity to cold food/fluids in lower front tooth since one year and an unpleasant look. The patient was systemically healthy. On examination, it was seen that there were two mucogingival problems in lower anterior teeth region. Firstly, there was a gingival fenestration in 31 with visible root surface. Secondly, there was a gingival recession in 41 with vertical component of 4 mm, probing depth of 2 mm, clinical attachment level of 6 mm, and keratinized gingiva of 2 mm. Plaque and thick subgingival calculus were present and marginal gingiva was inflamed in the region [Table/Fig-1]. IOPAR showed there was minimal bone loss in the area, with good prognosis. Diagnosis of the lesion was made as “Gingival fenestration on 31 and Miller’s class-I gingival recession in 41”.
Treatment included phase-I therapy (scaling and root planning of the involved teeth), followed by maintenance [Table/Fig-2]. Phase-II therapy consisted of coronally repositioned partial thickness graft using microsurgical technique. Initially, coronally repositioned partial thickness with connective tissue graft was considered, but patient did not agree for second donor site surgery. Therefore, coronally repositioned partial thickness graft using microsurgical technique was considered.

Clinical procedure
Patient was motivated and educated about the surgical procedure and oral hygiene instructions were given. Thorough scaling and root planning was done. Patient was called on recall visits to assess his oral hygiene and gingival status. Informed consent was taken from patient.
Baseline data was recorded preoperatively with a gingival fenestration in 31 with visible root surface and a gingival recession in 41 with vertical component of 4 mm, probing depth of 2 mm, clinical attachment level of 6 mm, and keratinized gingiva width of 2 mm. An operating microscopic loupe adjusted to 4 × magnification was used for the entire procedure. After administration of local anaesthesia, a partial thickness flap was created. Two vertical incisions were placed with extension from a point coronal to the CEJ, at the mesial line axis of 42 and distal line axis of 31, running apically into the lining mucosa [Table/Fig-3]. The coronal margin of the flap was started with a horizontal sulcular incision to preserve all existing radicular gingiva. The interproximal papillae were left intact. Care was taken to extend the flap to the mucobuccal fold without perforations, which could seriously affect the blood supply. Thorough root planning was done. The concavity in the root was reduced with air-rotor hand piece. The partial thickness flap was positioned coronally in a manner to cover as much of the recession defect and fenestration area. It was sutured in this position using 6-0 vicyrl absorbalabe suture [Table/Fig-4]. Periodontal dressing with a protective thin tin foil was applied to the surgical site, and the patient was instructed in normal post-surgical management.
Reflection of partial thickness flap under 4x magnification

Suture placed (6-0, vicryl) under 4X magnification

Patient was instructed to avoid any mechanical trauma in the surgical area tooth-brushing. Chlorhexidine rinses (twice daily for 1 minute), antibiotics and anti-inflammatory analgesics were prescribed for five days after surgery. Ten days after surgery, periodontal dressing and the remaining absorbable sutures were removed. About 3 weeks after surgery, patient was instructed to continue his mechanical tooth-cleaning with soft toothbrush and toothpaste in the treated area.
The patient was recalled regularly and at the end of one month, there was a gain in attached gingiva with closure of gingival fenestration in 31 and root coverage of 3 mm in 41 [Table/Fig-5].
Post operative after 8 weeks

Discussion
A ginigval fenestration is a window of bone loss on the facial or lingual aspect of a tooth. This places the exposed root surface directly in contact with gingiva or alveolar mucosa. It can be distinguished from dehiscence in that the fenestration is bordered by alveolar bone along its coronal aspect [1]. Gingival fenestrations of uncertain aetiology have rarely been reported in the dental literature.
Several surgical techniques have been introduced to treat gingival fenestration, including Connective Tissue Grafting (CTG), various flap designs; orthodontics; and Guided Tissue Regeneration (GTR) [2]. However, none of these methods have been proved to be predictable for treating fenestration in human gingival tissues. Among various flap designs, the Coronally Positioned Flap (CPF), solely or combined with other procedures, e.g., subepithelial connective tissue graft (SCTG), has been one of the most widely used procedures in the treatment of Miller Class I gingival recessions. Therefore, in the present case, we selected coronally repositioned flap to treat both the fenestration and the adjacent recession lesion.
The Coronally positioned flap (CPF) is a modality of root coverage surgery that does not involve a palatal donor site and has been demonstrated to be a safe and predictable approach. Successful (83% is the mean percentage of root coverage) and predictable (58% is the mean percentage of teeth with complete root coverage) results have been reported in a meta-analysis [3] for single type recession. These favourable results are maintained over long term observation period. In patients with high aesthetic expectations, when there is adequate keratinized tissue apical to the root exposure, the coronally advanced flap is the first choice [4–6]. In this approach, the soft tissue utilized to cover the root exposure is similar in colour, texture and thickness to that originally present at the buccal aspect of the tooth with the recession defect and thus, the aesthetic result is more satisfactory [7–8].
Currently, the application of microsurgery is a part of this process and has helped Periodontists in treating the patient in a conservative manner, using enhanced visibility of the surgical field and minimizing surgical wounds, to achieve a favourable treatment outcome. Thus, the superior end point of aesthetic appearance following microsurgery as compared to conventional surgery results from remarkable advantage magnification offers to microsurgery. Burkhardt and Lang, [9] in their study, showed that root surface coverage with a sub epithelial connective tissue graft using a microsurgical approach, substantially improved the vascularization of the grafts, seen with fluorescent angiograms. This resulted in increased percentage of root coverage as compared to applying a conventional macroscopic approach.
Conclusion
In the present case, we applied the concept of CPF under 4 X magnification to treat both lesions. The result outcome demonstrated that CPF under microsurgical technique has strong practical application, especially in the field of periodontal plastic surgery. It reduces tissue trauma, aids in early postoperative healing, and increased comfort to patients. Further, long term studies are anticipated to focus on precise effects of such surgeries.
[1]. Santos-Pinto LA, Seale NS, Reddy AK, Cordeiro RC, Fenestration gingival defect in erupting permanent mandibular incisors: a case reportQuintessence Int 1998 29:239-42. [Google Scholar]
[2]. Shanelec DA, Tibbets LA, Periodontal microsurgeryDental Clinics North Am 1998 42:339-59. [Google Scholar]
[3]. Cairo F, Pagliaro U, Nieri M, Treatment of gingival recession with coronally advanced flap procedures. A systematic reviewJ Clin Periodontol 2008 35(supplement):136-62. [Google Scholar]
[4]. Roccuzzo M, Bunino M, Needleman I, Sanz M, Periodontal plastic surgery for treatment of localized gingival recessions: a systematic reviewJ Clin Periodontol 2002 29:178-94. [Google Scholar]
[5]. Carvalho PF, da Silva RC, Cury PR, Joly JC, Modified coronally advanced flap associated with a subepithelial connective tissue graft for the treatment of adjacent multiple gingival recessionsJ Periodontol 2006 77:1901-06. [Google Scholar]
[6]. Chambrone LA, Chambrone L, Subepithelial connective tissue grafts in the treatment of multiple recession-type defectsJ Periodontol 2006 77:909-16. [Google Scholar]
[7]. Zabalegui I, Sicilia A, Cambra J, Gil J, Sanz M, Treatment of multiple adjacent gingival recessions with the tunnel subepithelial connective tissue graft: a clinical reportInt J Periodontics Restorative Dent 1999 19(199-206)PubMed [Google Scholar]
[8]. Wennstrom JL, Pini Prato GP, ucogingival therapy. In Lindhe J, Karring T, Lang NP, edsClinical Periodontology and Implant Dentistry 1997 CopenhagenMunksgaard:550-96. [Google Scholar]
[9]. Burkhardt R, Lang NP, Coverage of localized gingival recessions- comparison of micro” and miacrosurgical techniquesJ Clin Periodontol 2005 32:287-93. [Google Scholar]