Fibromatoses are a heterogeneous group of distinct entities which differ in biological behaviour, but arehistologically very similar. This group of fibrous tumor or tumor like lesions, present considerable difficulties in pathologic diagnosis. Aggressive fibromatosis (AF) of the oral or para-oral structures is a very uncommon finding and its intra-osseous component is even relatively unusual. Such lesions with their origin from within the bone are termed desmoplastic fibromatosis (DF). These lesions must be distinguished from other fibroblastic tumors of the head and neck such as benign fibrous histiocytoma (BFH), fibrosarcoma, nerve sheath tumors and tumors of muscular origin. The major challenge in dealing with lesions of fibromatosis is to avoid an overdiagnosis of fibrosarcoma or an underdiagnosis of reactive fibrosis.Problems of differential diagnosis concern a wide range of diseases and immunohistochemical analysis may be helpful in diagnosis. With respect to the patient’s post-operative well-being and if periodic follow-ups are guaranteed, the tumor should be carefully resected with only narrow safety margins. A rare case of aggressive desmoplastic fibromatosis in a 12–year–old girl is presented in this article with emphasis on the need and challenges for diagnosing such lesions as they have to be differentiated from other soft tissue tumors which display borderline pathological features regarding benign or malignant behaviour. Synonyms listed for the same include extra-abdominal desmoids, extra-abdominal fibromatosis, desmoids tumor, aggressive fibromatosis, juvenile desmoids-type fibromatosis, infantile fibromatosis.
Case Report
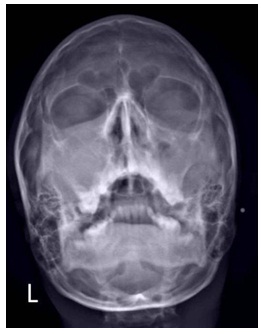
A 12-year-old female presented with a three month history of a rapidly expanding, painless swelling in the left anterior maxillary region [Table/Fig-1]. Past medical history revealed that the patient had visited a general physician two months back for facial asymmetry and a diffuse swelling in that region which rapidly increased in size. Extraoral examination revealed a solitary, diffused globular swelling of size 6 cm x 5 cm extending superiorly from the infraorbital margin of the eye to the angle of the mouth inferiorly. Medially it extended from the lateral aspect of nose, involving the malar region to the preauricular region laterally. Swelling was firm and non tender on palpation. Intra orally on inspection, a diffuse swelling of size 4 cm x 2 cm was seen extending from distal aspect of canine to the distal aspect of first molar, with normal palatal borders [Table/Fig-1], Inset). The buccal vestibule was obliterated and second premolar was missing. The overlying mucosa was normal with no ulceration. On palpation the swelling was firm and non tender. The teeth associated were vital and mobile with normal periodontal condition. The remainder of head and neck examination was within normal limits with no significant lymph node enlargement. Periapical radiographic revealed a diffuse radiolucent lesionwith thick ill defined septae [Table/Fig-2], inset). Panaromic radiograph showed a diffuse radiolucent lesion of size 4 cm x 2 cm with displaced roots of # 24 and # 26 [Table/Fig-2]. Waters view showed haziness of the left maxillary sinus with expansion and thinning of the sinus walls [Table/Fig-3]. Correlating with the clinical and radiological findings a provisional diagnosis of fibro-osseous lesion/adenomatoid odontogenic tumor (AOT) was made. Under local anesthesia, an incisional biopsy of the lesion was obtained and submitted for histological evaluation.
Photograph showing swelling in the left anterior maxillary region. Inset showing an expansion of the buccal cortical plate with normal palatal borders

Panaromic radiograph showing a diffuse radiolucent lesion with displacement of roots of # 24 and #26. Inset shows periapical radiograph revealing radiolucent lesion with thick ill defined septae

Waters view showed haziness of the left maxillary sinus with expansion and thinning of the sinus walls
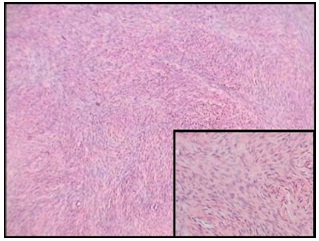
Microscopic examination revealed spindle shaped cells in a collagenized stroma. The architectural arrangement of the spindle cells varied with groups of cells arranged in storiform to parallel fashion, mixed with short interlacing fascicles and intertwining strands [Table/Fig-4]. The nuclei of these cells were uniformly bland with rare mitosis and no cytological atypia. Few round to oval cells with vesicular nuclei were present in one area of the field which resembled histiocytes. Residual bony fragments were noted at the periphery of the section. Since there is a histological overlap between desmoplastic fibromatosis, reactive fibrosis, non ossifying fibroma, benign fibrous histiocytoma, and low grade fibrosarcoman and these lesions display borderline pathological features regarding benign or malignant behaviour, hence a diagnostic challenge was posed.To ascertain the nature of origin of this spindle cell lesion immunohistochemical analysis was performed.
Spindle cells arranged in storiform to parallel fashion, mixed with short interlacing fascicles and intertwining strands (H& E, X10). Inset showing the same in X40
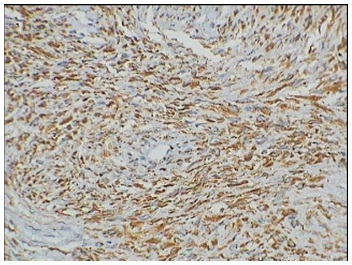
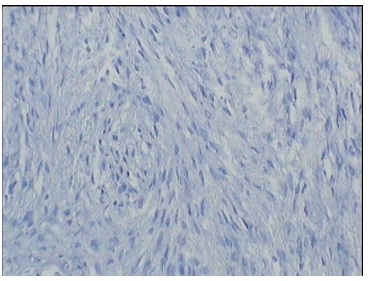
Paraffin-embedded tissue sections, fixed in formalin, were stained with the following antibodies obtained from Dako Corporation (Carpinteria, CA), according to manufacturer’s recommendations: a) antivimentin, b) anti-SMA, c) anti- S-100 and d) anti-CD68. Diffuse positive staining was seen for vimentin [Table/Fig-5], while the tissue was nonreactive for rest of the antibodies [Table/Fig-6]. Based on clinical behaviour and histomorphological features, a definitive diagnosis of aggressive desmoplastic fibromatosis was rendered.
Diffuse positive staining seen for vimentin (IHC, X40)
Non reactive stain for CD68 (IHC, X40)
Discussion
Desmoid tumors, also called aggressive fibromatosis (AF), are rare neoplasms, occurring both sporadically and in the context of familial adenomatous polyposis, also recognized as Gardner’s syndrome. Although their growth is locally infiltrative they never metastasize [1,2]. On the other hand 10% exhibit unpredictable biological behaviour with extremely aggressive growth potential. Others tend to regress spontaneously [2,3]. The lesion usually arises from the tissue of the musculo-aponeurotic system. Between 7% and 15% of extra abdominal fibromatosis occur in the head and neck region, 26% of which arise from the soft tissues (including the periosteum) around the mandible [3,4].
Fibromatosis constitutes part of a spectrum of poorly understood proliferative lesions whose histologic features overlap to such an extent that the pathologist may be more influenced by the anatomic location of the lesion, sex and clinical behaviour than by the histologic appearance in rendering diagnosis. Wherever it occurs, the diagnosis of fibromatosis is always a source of concern [5].
DF represents the osseous manifestation of AF and was first reported by Jaffe in 1958 [6] who described multiple sites of involvement in the tibia, scapula, and femur. The first report of gnathic involvement with DF is attributed to Griffith and Irby in 1965 [7].
The etiology of DF remains unknown, however trauma [6], endocrine [8] and genetic factors [8] have all been suggested as possible etiologic agents. While most investigators believe that DF represents the osseous counterpart of soft tissue fibromatosis, [8] others have classified it as a variant of nonossifying fibroma (NOF) of bone, [9] and considered it to be biologically intermediate between benign fibrous lesions and fibrosarcoma [10].
Review of literature suggests that most cases of AF are clinically misdiagnosed. Preliminary diagnosis considered ranged from fibroma, fibrous histiocytoma, granuloma, cyst, ameloblastoma, fibrous dysplasia to sarcoma [11]. Similarly in the present case with correlation of age, site, gender and radiographic features a misdiagnosis of a fibro osseous lesion / AOT was made.
World Health Organization defines the histological criteria for desmoplastic fibromatosis as that of a benign tumor of low to variable cellularity, whose cells can be ovoid or elongated with uniform nuclei that lack atypia, pleomorphism and mitotic activity. The tumor cells are supported by a matrix of collagenized, variably hyalinized fibrous connective tissue [12].
In the present case microscopic examination revealed spindle shaped tumor cells in a storiform to interwining pattern with rare mitosis and no cellular atypia, and this ruled out the possibility of a fibro osseous lesion /AOT. The foremost situation was to differentiate between fibromatosis, low grade fibrosarcoma, reactive fibrosis and fibrous histiocytoma. For surgical pathologist the major challenge in dealing with lesions of fibromatosis is to avoid an overdiagnosis of fibrosarcoma or an underdiagnosis of reactive fibrosis [13]. Fibromatosis has a more uniform growth pattern, more mature cells, and a paucity of mitosis compared with fibrosarcoma. Reactive fibrosis such as that following injury or trauma has a more variable growth pattern than fibromatosis and may show areas of focal hemorrhage or hemosiderin deposition. The absence of above mentioned features in the present case helped it in differentiating it from reactive fibrosis and low grade fibrosarcoma.
Some childhood lesions proliferate very rapidly and histologically can be very cellular and active so that a diagnosis of sarcoma is seriously entertained and radical treatment carried out. Occasionally, the histomorphology may fail to reflect the biological behaviour of the lesions which can occasionally be localized, such as myofibromatosis, and as such be amenable to conservative surgery. On the other hand, some childhood fibrous lesions such as infantile fibromatosis may grow in a persistent and infiltrative manner. These lesions continue to present a difficult diagnostic problem, especially to pathologists.
Fibrous histiocytoma consists of proliferating fibrohistiocytic cells showing a storiform pattern arrangement, and various numbers of foam cells and giant cells and histologically it is indistinguishable from NOF. Both should be differentiated based on clinical radiographic setting. Clinically, BFH in bone frequently occurs in adults and causes pain, without bone fractures. NOF is centered in the metaphysis of the long bones and radiologically show a lytic lesion with a sharply circumscribed sclerotic rim, whereas BFH occurs in non-long bones, or lack of metaphyseal involvement even if in a long bone. Furthermore, radiographic sclerotic rim is generally seen in NOF, but not in BFH [14].
Immunohistochemical analysis performed to distinguish this lesion from other spindle cell lesions showed a diffuse positivity for vimentin and non reactivity for other antibodies. A negative stain for CD 68 negated the possibility of BFH. Non reactivity for SMA and S 100 confirmed the fibrous origin of this lesion and ruled out origin from muscular or neural tissue respectively. Optimal management of AF is based on clear diagnosis by histologic and clinical examination, therefore, adequate biopsy is mandatory. According to literature, surgery is the most common treatment of AF in head and neck region, and inadequate excision results in recurrences [15]. Extensive and mutilating resection of a benign neoplasm is a difficult decision. However, the disease can result in a lethal outcome. Therefore, complete excision of AF with a generous border of histologically tumor free tissue is generally recommended.
Mutilating tumor resections should be avoided whenever possible: Therefore extended tumors require a multimodal, multidisciplinary treatment approach. The therapy alternatives in AF include: chemotherapy, hyperthermy, therapy with hormonal agents and NSAID therapy [2].
Management of AF in children must be tailored to the individual patient and the clinical situation, requiring cooperation between surgeons, pathologists and oncologists.
Conclusion
Soft tissue tumors in the head and neck region sometimes display borderline pathological features regarding benign or malignant behaviour. The present case highlights the perplexity in diagnosing a lesion of spindle cell origin. Problems of differential diagnosis concern a wide range of other diseases and immunohistochemical analysis may be helpful in diagnosis. With respect of the patient’s post-operative well-being and if periodic follow-ups are guaranteed, the tumor should be carefully resected with only narrow safety margins.
[1]. Chaudhuri B, Das Gupta TK, Pathology of soft tissue sarcomas. In: Das Gupta TK, Chaudhuri PK, editorsTumors of the soft tissues 1998 Stamford (Conn)Appleton and Lange:63-200. [Google Scholar]
[2]. Seper L, Burger H, Vormoor J, Joos U, Kleinheinz J, Agressive fibromatosis involving the mandible- Case report and review of the literatureOral Surg Oral Med Oral Pathol Oral Radiol Endod 2005 99:30-8. [Google Scholar]
[3]. Peterschulte G, Lickfeld T, Moslein G, The deskoid problemChirurg 2000 711:894-903. [Google Scholar]
[4]. Carr RJ, Zaki GA, Leader MB, Langdon JD, Infantile fibromatosis with involvement of the mandibleBr J Oral Maxillofac Surg 1992 30:257-62. [Google Scholar]
[5]. Batsakis JG, Tumors of the head and neck 1979 2nd edBaltimoreWilliams & Wilkins:252-79. [Google Scholar]
[6]. Jaffe HL, Tumors and timorous conditions of the bone and joints 1958 PhiladelphiaLea & Febiger:298-308. [Google Scholar]
[7]. Griffith JG, Irby WB, Desmoplastic fibroma: report of a rare tumor of the oral structuresOral Surg Oral Med Oral Pathol 1965 20:269-75. [Google Scholar]
[8]. Said-Al-Naief N, Fernandes R, Louis P, Bell W, Siegal GP, Desmoplastic fibroma of the jaw: A case report and review of literatureOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101:82-94. [Google Scholar]
[9]. Siemssen SJ, Anagnostaki T, Aggressive fibromatosis (extraabdominal desmoids) of the head and neckBr J Plast Surg 1984 37:453-7. [Google Scholar]
[10]. Neville B, Damm D, Allen C, Bouquot J, Textbook of oral and maxillofacial pathology 2002 2nd edPhiladelphia, PA, USAWB Saunders Company:573-4. [Google Scholar]
[11]. Donohue WB, Malexos D, Pham H, Aggressive fibromatosis of the maxillaOral Surg Oral Med Oral Pathol 1990 69:420-6. [Google Scholar]
[12]. Fowler CB, Hartman KS, Brannon RB, Fibromatosis of the oral and paraoral regionOral Surg Oral Med Oral Pathol 1994 77:373-86. [Google Scholar]
[13]. Fletcher CDM, Uni KK, Mertens F, WHO classification of tumorsPathology and genetics of tumors of soft tissue and bone 2002 LyonIARC Press:288 [Google Scholar]
[14]. Kishino M, Murakami S, Toyosawa S, Nakatani A, Ogawa Y, Ishida T, Ijuhin N, Benign fibrous histiocytoma of the mandibleJ Oral Pathol Med 2005 34:190-2. [Google Scholar]
[15]. Melrose RJ, Abrams AM, Juvenile fibromatosis affecting the jaws. Report of 3 casesOral Surg Oral Med Oral Pathol Oral Radiol Endod 1980 49:317-24. [Google Scholar]