Introduction
Patients with severe non traumatic injuries to the central nervous system .i.e. the brain and / spinal cord are bedridden for prolonged periods. Soule, in [1], reported para-articular calcification round the hips of war injured paraplegics, and he pointed out the severity of the neurological deficit, and that some cases were associated with infection. Damanski, in [2], while reviewing the subject, mentioned the frequency of the phenomenon in association with spastic paraplegia from lower dorsal injuries. Isolated cases have been described in hemiplegia, to be caused by cerebrovascular accidents by Voss in [3], Irving and LeBrun in [4], Roberts in [5], Radt in [6], and Rosin in [7].
Other conditions have been mentioned in published reports in which para-articular calcifications which occur have been listed to be multiple sclerosis, encephalitis, and cerebral tumour (Storey and Tegner, [8]. In addition, calcifications occurring around joints in patients suffering unconsciousness and neurological damage as a result of head injuries, have also been reported (Roberts in 5; Pryor in 1970 [9]; Money in [10].
Sullivan et al., in [11], have published the latest current review on heterotopic ossification after central nervous system trauma. Alfieri KA et al., in [12], focussed on blast injuries and heterotopic ossification, while Patil SG et al., in [13], reported an unusual presentation in a paediatric patient in which these ossifications occurred in close proximity to temporo- mandibular joint and affected the development of mandible and maxilla. Mavrogenis AF et al., in [14], revisited heterotopic ossification and discussed its causes, diagnosis and management. Mishra MV et al., in [15], highlighted the safety and efficacy of radiation therapy as secondary prophylaxis for heterotopic ossifications of non-hip joints, whereas Halas RA and Karuppiah S, in [16], concentrated on heterotopic ossifications of the hip after stroke. Genêt F et al., in [17], studied troublesome heterotopic ossifications which followed central nervous system damage by performing a survey on 570 surgeries.
This rare phenomenon [11,14,16,18] consists of ectopic calcification within the muscles around large joints of affected limbs, without involvement of the interior of the joint itself. The calcifying process proceeds to ossification, ranging from a large mass of bone surrounding the joint and even uniting with adjoining bony structures to discrete knots of bone in the muscular tissues near the joint. Another type of calcifying process occasionally described is that of subperiosteal calcification with subsequent regression of the process, leaving a residual thickening of the bony cortex in the subarticular zone.
Heterotopic ossification (HO) is abnormal formation of mature bone in soft tissues, where it is normally not expected to exist. It cannot be differentiated from normal bone structurally. Central nervous system damage caused by traumatic injuries [11,12,19, 20] or which rarely follows a nontraumatic insult [14,16,21,22], can lead to HO.
A prospective study 22 done on heterotopic ossifications in non-traumatic myelopathies, showed that 6.04 % of patients who had non traumatic spinal cord injuries developed HO. They also concluded that any neurologic insult could lead to HO. It is more common with traumatic injuries than with non traumatic injuries. Moreover, its incidence is more common with spinal cord lesions than with brain lesions.
Perigenicular HO is rare sequelae in patients who have had an injury or insult to central nervous system. Its cause or exact mechanism is still unknown. According to Buring K [23], local or distant mesenchymal cells transform into bone forming osteoblasts and they thus, start this new ossification into areas where normally no bone exists. HO which occurs due to neurogenic causes, arises in the connective tissues, away from joint space and joint capsule [16,24].
Case Report –How a typical process of HO evolves
HO has typical clinico-radiological features. Clinically, at the onset, there are local signs and symptoms which are similar to inflammation [11, 23, 25]. The patients usually present with swollen joints and a decreased range of motion. Three phase bone scan is the investigation of choice for detecting the onset of HO [11, 14, 26].
The following case shows how the process evolves and the mystery unfolds in a bizarre clinical presentation. A twenty one year old male was admitted to the intensive care unit after his relatives found him in a state of sudden unconsciousness. There was neither history of trauma nor fever. He had not sustained any injury to head, spine or knees. He was kept in intensive care unit for 45 days and had not received any intramuscular injection in the thighs. He was given physiotherapy after one and half months of initial care. However, he left it against medical advice and returned eight months later, with history of difficulty in walking. It was insidious in onset and was gradually progressive.
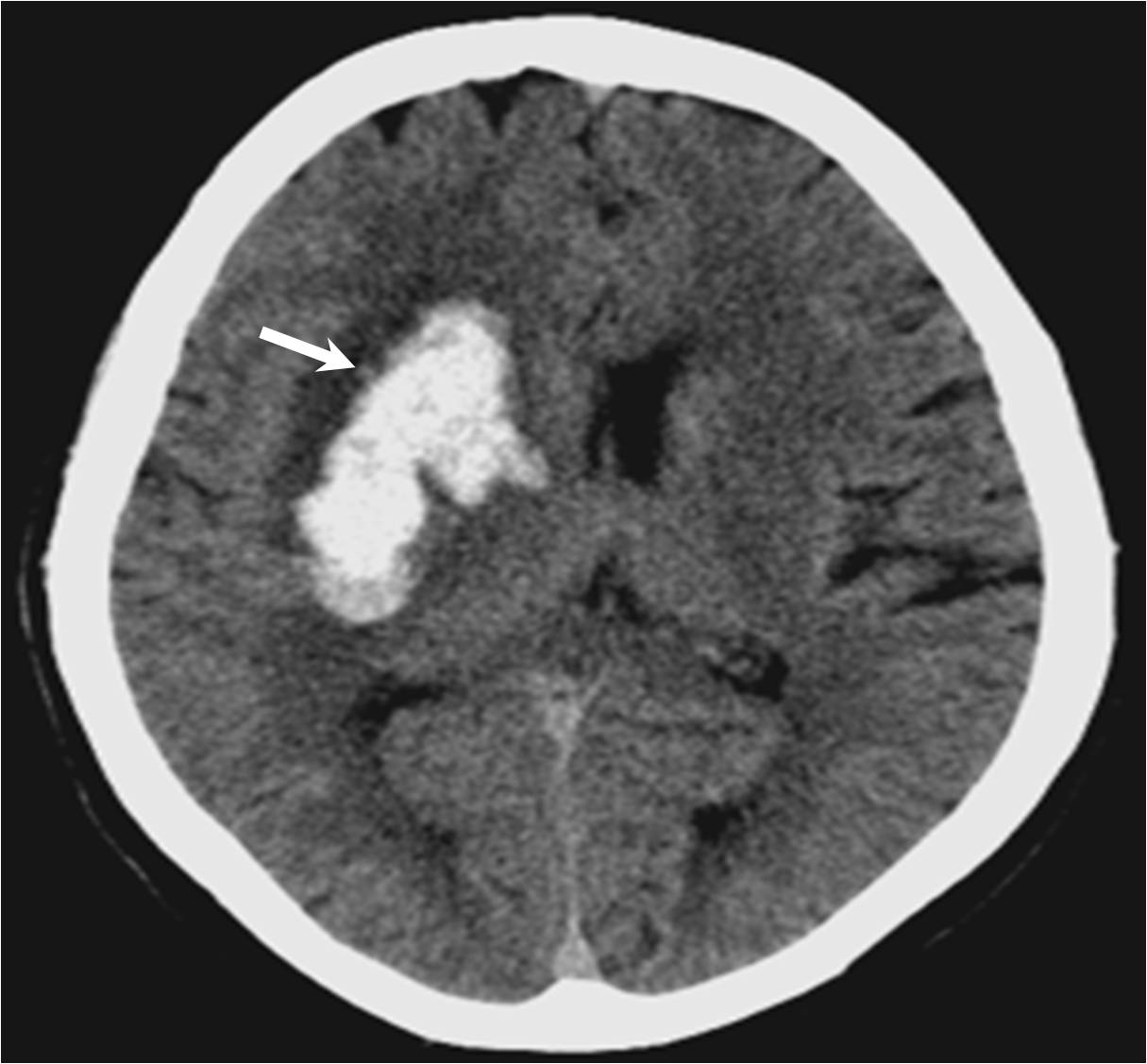
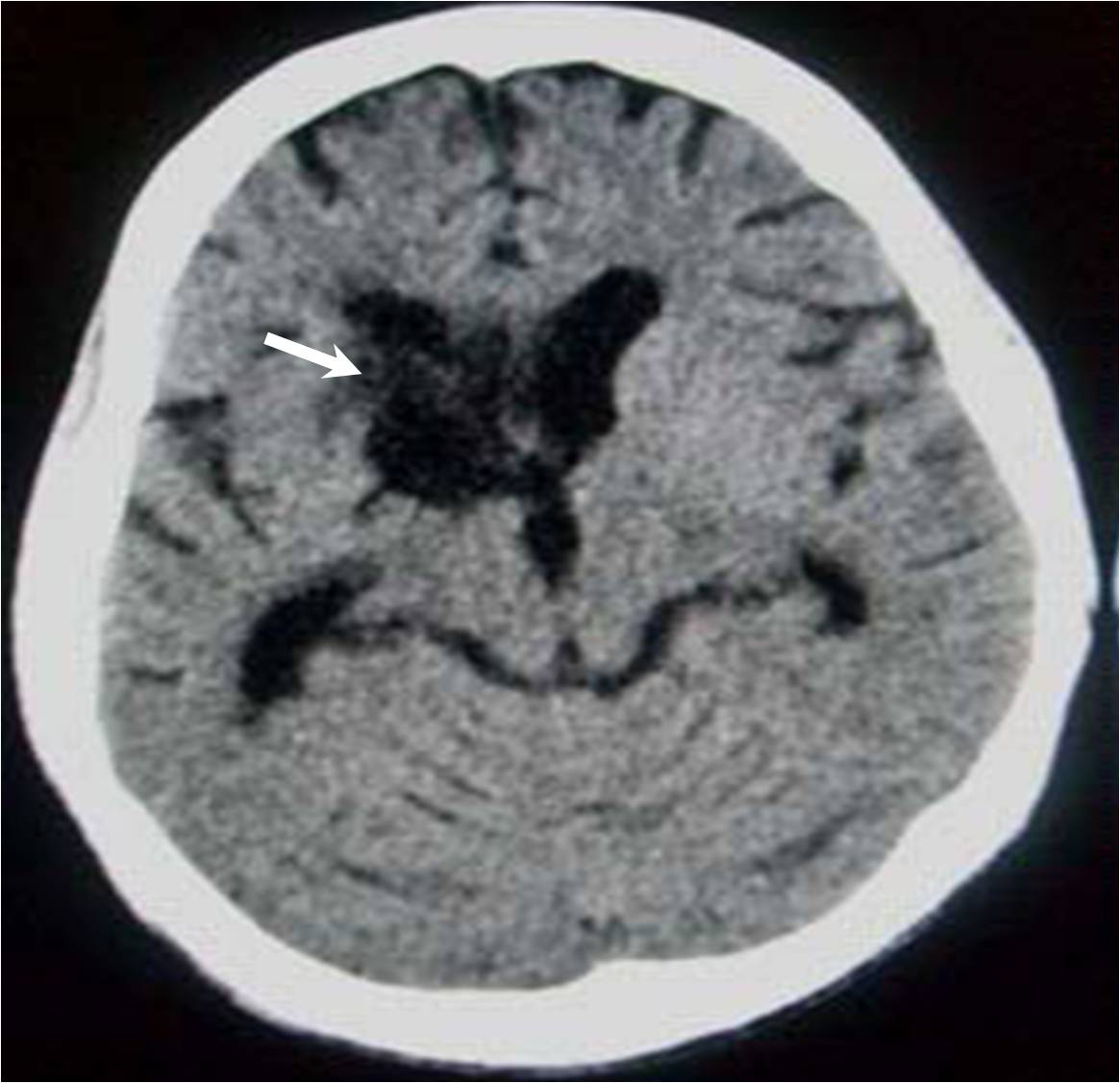
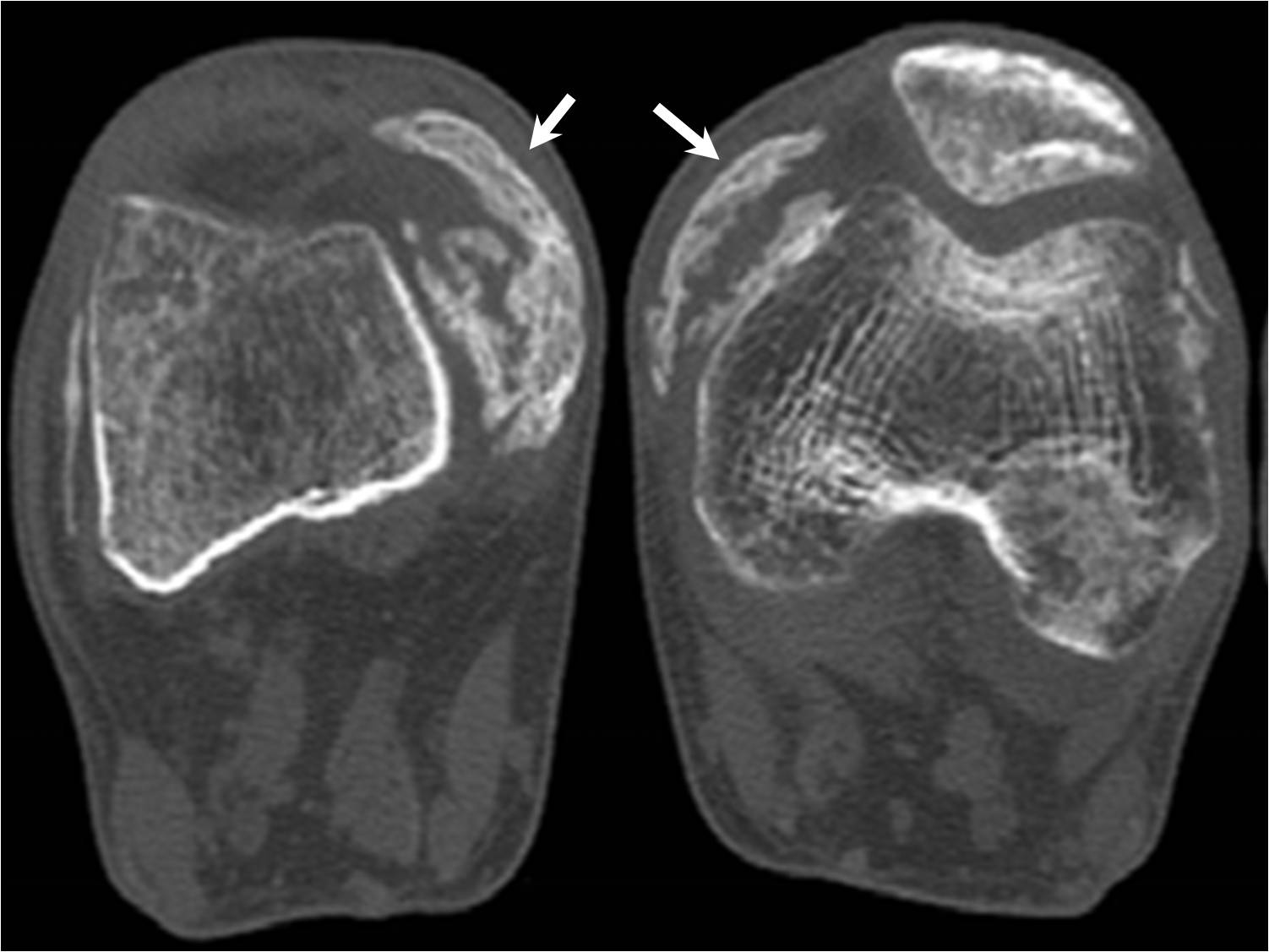
CT scan done at the time of ictus [Table/Fig-1] showed fresh right ganglio-capsular bleeding, which was the cause of his sudden unconsciousness. However, he slowly recovered from it. Plain CT done at the time of presentation with difficulty in walking [Table/Fig-2], showed resolved intracranial bleeding and areas of residual gliosis. Plain radiographs [Table/Fig-3] and Axial CT images [Table/Fig-4] demonstrated bilateral peri genicular areas of well formed bone on medial aspect. Thus, a diagnosis of bilateral peri genicular heterotopic ossification was made. MRI of both knees [Table/Fig-5] confirmed the areas of altered signal intensities in perigenicular soft tissues, in addition to the heterotopic bone formation on medial aspect of distal part of femurs.
Plain CT scan of brain showing acute right gangliocapsular bleed
Plain CT follow up scan showing resolved bleed and gliotic changes
Plain radiograph showing mature bone in soft tissues around knees

Plain CT scan axial images showing mature bone in perigenicular soft tissues
MRI STIR coronal image showing hyper intense signals in soft tissues on medial aspect of both knees
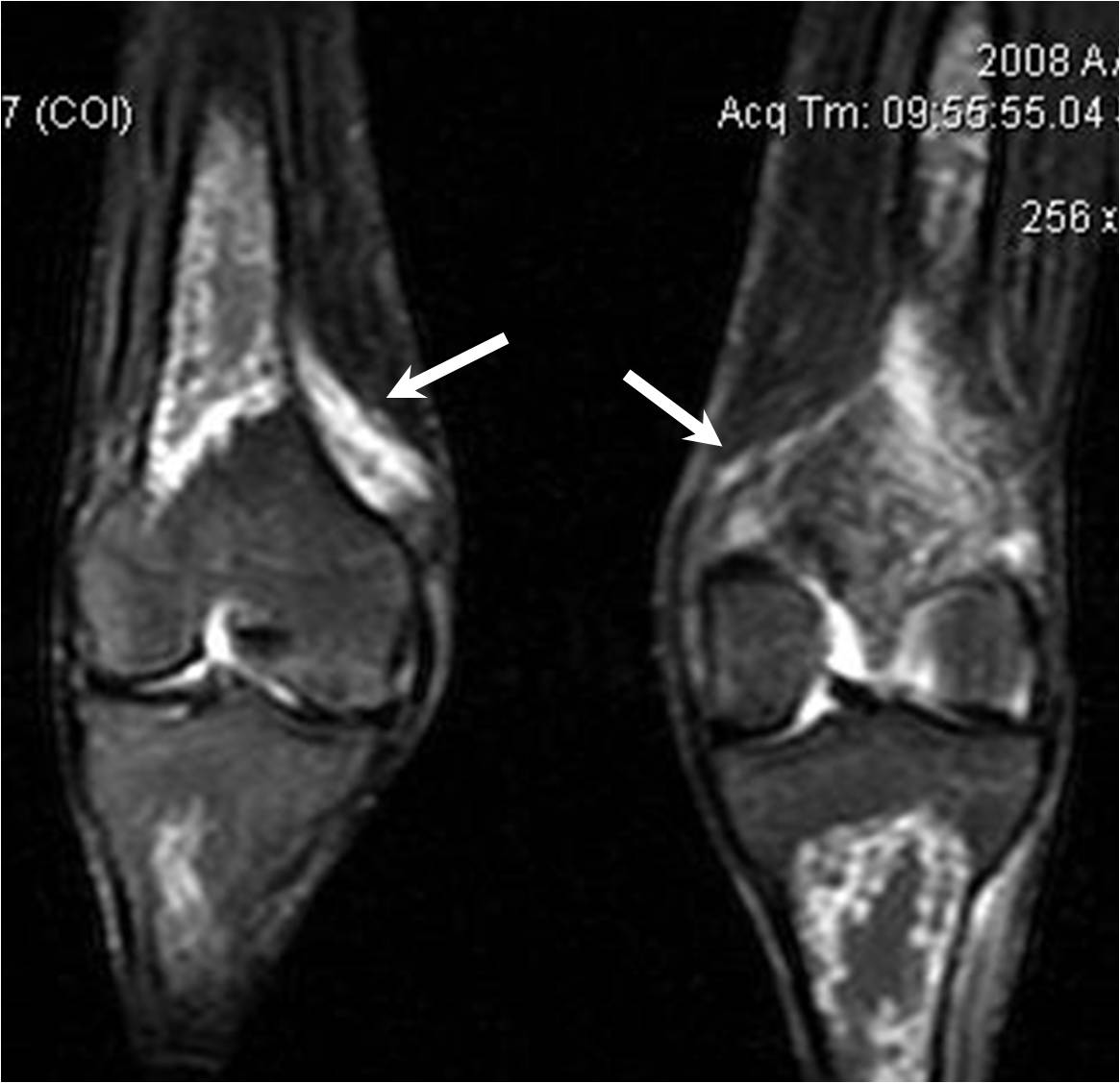
Clinical examination revealed small bulges on medial aspects of both knees [Table/Fig-1]. There was restriction of range of motion at both the knee joints. Knee flexion was possible to only 20 degrees from neutral position on either side. Patient was advised to get MRI of knees performed as soon as possible, as MRI was supposed to be most informative for evaluating soft tissues in and around joints.
Plain MRI of knees showed abnormal hyper intense areas in the soft tissues around knees on coronal Short Tau Inversion Sequence (STIR), suggestive of oedema. Heterotopic bone formation on medial aspect of distal part of femurs was also seen as abnormal osseous structure, which was same in signal intensity to that of the bone on STIR.
Imaging helped in realizing that heterotopic ossification had occurred in this patient. Immediately, physiotherapy was started to rescue the joint movements. The patient was counseled and was given a choice of surgical excision of the excess bone, if it hampered joint movements. He was asked to come for follow up every 6 months, so that he could undergo surgery if the bone matured. Unfortunately, once discharged; the patient did not turn up.
Discussion
In a series 18 published on ectopic calcification around joints of paralyzed limbs in hemiplegia, diffuse brain damage, and other neurological diseases, most of the patients who had subsequently developed ectopic calcifications had initially complained of pain, which emphasizes the inclusion of ectopic calcification as a cause of pain which was associated with hemiplegia. In such cases, the cause of pain in extremities is not apparent until 4 weeks to 4 months after the stroke, when the first signs of calcification appear around the adjacent joint. In such cases, the diagnosis can be made clinically by rotating the joint hip and palpating an unexpected hard mass overlying it.
The presence of calcification around the joints might occur in grossly rigid limbs, and it might therefore not be suspected. Comparison of hemiplegic patients with and without para-articular calcifications revealed no differences regarding side of hemiplegia, incidence of unconsciousness at the outset, or sensory signs [18]. Moreover, fracture of the femur at the time of the onset of a hemiplegia or shortly thereafter, is not uncommon, but is not usually associated with excessive callus to the extent of myositis ossificans.
The Pathophysiology
Perigenicular HO is a rare sequelae in patients who have had an injury or insult to central nervous system. Its cause or exact mechanism is still unknown. According to Buring K [11,14,23], local or distant mesenchymal cells transform into bone forming osteoblasts and they thus start this new ossification into areas where normally no bone exists. HO which occurs due to neurogenic causes, arises in the connective tissues, away from joint space and joint capsule [16,17,24].
The cause of the condition remains a mystery [11,14,18]. Age had no influence on the appearance of periarticular ossification in patients with paraplegia or hemiplegia. The neurological lesion had caused spasticity in most of the cases. However, spasticity was not an invariable finding, and the degree of increase of muscle tone bore no correlation with the disposition of the periarticular calcification. No correlation was found between the occurrence of calcification around joints and the incidence of unconsciousness at the onset of the stroke, the degree of neurological or functional recovery, or the degree of sensory impairment.
The relationship of a rising alkaline phosphatase with the development of the bony mass [27,28] is a reflection of active bone formation and it may be used as an indication that the suspected ectopic calcification is proceeding despite the absence of symptoms. The occurrence of excessive calluses around fractures in such patients points to an exaggerated response to proliferation of repaired bony tissue. However, this does not happen in every case of fracture in a hemiplegic limb. Moreover, the possibility of a traumatic haematoma seems unlikely, since no predisposing feature rendering the limb more liable to traction was seen in those cases as compared to that in hemiplegics without calcifications [18]. Myositis ossificans can also occur around a subluxated shoulder of a hemiplegic limb, in which rupture of the supraspinatus is said to take place [29]. Although severe infection near the area of calcification has been suggested as an aetiological factor, many of patients reported by Rosin [18] had no infection and many para-articular calcifying masses were located remotely from pressure sores. One of the early descriptions of ‘atypical myositis ossificans’ [30] concerned cases of burns in which calcifications occurred around joints which were immobilized, either because of the burn or because of the treatment. In most of the cases, the ossifications occurred around joints remote from the burnt site. This common factor of immobilization of the limb also appeared in the cases which have been quoted above.
What was strange was that ossifications did not occur more often in hemiplegia, that neurological recovery with limb movement took place in some cases, and ossifications were seen around some joints and not around others after severe head and brain injuries [18].
Another theory which has been suggested is that sympathetic dysfunction causes changes in vascularization to the periarticular tissues, with osteoporosis of the bone and transfer of calcium to the tissues outside the joint [31]. The rapid and firm union of the fractures in cases with excessive calluses does not favour this, but it instead supports the idea of change in mesenchymal cell function from that of making connective tissue to that of making bone. How this stimulus is caused by the disturbance of neurological function is not known, but the result seems to be a rapid, localized vascularization near the joint, with ossification in the connective tissue and muscle.
The Health Impacts of HO
The para-articular calcification described in the series by Rosin; AJ [11,14,18] occurred around the joints and it was sometimes so extensive, as to resemble myositis ossificans. Two positive symptoms and two negative ones were apparent. There was pain in most cases of hemiplegia, associated with the growth and development of the calcification. The paraplegic patients with sensory loss did not however, feel pain, nor did patients with head injuries who developed calcifications while they were in a state of impaired consciousness. The other important symptom was mechanical loss of movement at the joint, caused by ankylosis from around it. This might result in difficulty in sitting, because of only minimal flexion position of the hips, or inability to stand, because of fixation of knees or hips in flexion, both of which complications were seen among their patients.
It was also noted [18] that a feature which was lacking in this syndrome of heterotopic calcification was involvement or destruction of the joint itself, for example, which occurs in Charcot joints which are associated with sensory nerve disturbances.
Furthermore, apart from ectopic calcification near joints of limbs involved in the neurological deficit, calcium is not laid down in soft tissues elsewhere, and this differentiates this condition from myositis ossificans progressiva, or calcinosis universalis.
A case of subperiosteal calcification has also been described [18] which differed from the para articular form in that it regressed and after a year only, a spur of bone remained protruding from the cortex. In rest of the cases, the mass of calcification progressively calcified and even ossified, but it did not regress.
Small calcifications and HO cannot significantly affect range of movement of joint. However, larger areas of HO can be distressing, as the restricted joint movement can significantly impair day to day activities. Massive HO can even lead to bony ankylosis.
Hence, it is necessary to prevent and treat HO. Slow passive movements that do not cause much stress and strain on the affected joints play a vital role towards this and they can maintain adequate function even though HO has started [11,14, 32].
Treatment is directed towards relieving pain and correcting mechanical contracture, where this is functionally inconvenient. Since this is a vascular growing tissue during the ossifying stage; any attempts made to remove it surgically usually fail, because of gross bleeding and regrowth of the bone [6]. Deep X-ray therapy was tried [7,15, 28], and the pain remitted after a few weeks, but in some other cases, it subsided spontaneously after several weeks. A diphosphonate compound has been used in the treatment of systemic myositis ossificans [33] because of its property of inhibiting the crystallization of hydroxyapatite, and it has been found to be successful in arresting the disease. A trial of this substance during the developing phase of the ossified mass in brain injury or vascular disease is therefore recommended.
Surgery is indicated after the completion of ossification, from 6 months after onset, when the removal of hard bone may not necessarily be followed by bleeding or by re-calcifications.
Medications like non steroidal anti- inflammatory drugs (NSAIDs) and diphosphonates [34] have been found to be useful in prevention and treatment of HO. Garland et al., [35] proposed that diphosphonates could inhibit occurrence and even post resection recurrence of HO.
Another study done [36] believes that NSAIDs are more useful in preventing post surgical recurrence. Preventive local radiotherapy in such cases was not studied earlier [37], but recent reports [15] have found it to be as safe and effective as secondary prophylaxis for heterotopic ossification of non-hip joints. Surgery for removing this newly formed distressing bone should only be done when the newly formed bone has fully matured. Radiotherapy and surgery have a debatable status in primary prevention [38].
The closest differential is myositis ossificans, that can occur after local trauma and massage. A careful history, clinical examination and evaluation for haematuria caused by rhabdomyolysis can differentiate them satisfactorily.
Conclusion
Thus, although rare; in all patients with a traumatic as well as a nontraumatic injury or insult to central nervous system; heterotopic ossification must always be kept in mind, so that it can either be prevented from occurring in the first place by early detection and timely management or from exceeding its limits; thereby, delimiting quality of life of the affected individual.
[1]. Soule AB, Neurogenic ossifying fibromyopathiesJournal of Neurosurg 1945 2:485 [Google Scholar]
[2]. Damanski MJ, Heterotopic calcification in paraplegiaBone Jt Surg 1961 43B:286 [Google Scholar]
[3]. Voss H, Uber die parostalen und para-artikularen Kuschen neubildungenbei organischen Nervenkrankleiten FortschrRontgenstr 1937 55:423 [Google Scholar]
[4]. Irving J, Le Brun H, Myositis ossificans in hemiplegiaIbid 1954 36B:440 [Google Scholar]
[5]. Roberts PH, J. Heterotopic ossification complicating paralysis of intracranial originBone Jt Surg 1968 50B:70 [Google Scholar]
[6]. Radt P, Peri-articular ectopic ossification in hemiplegicsGeriatrics 1970 25:142 [Google Scholar]
[7]. Rosin A J, Periarticular calcification in a hemiplegic limbJ. Amer. Geriat. Soc 1970 18:916 [Google Scholar]
[8]. Storey G, Tegner WS, Paraplegic para-articular calcificationAnn. Rheum. Dis 1955 14:176 [Google Scholar]
[9]. Pryor JP, Dystrophic muscle calcification following cerebral damageJ. Neurosurg 1970 32:353 [Google Scholar]
[10]. Money R, Ectopic para-articular ossification after head injuryMed. J. Aust 1972 1:125 [Google Scholar]
[11]. Sullivan MP, Torres SJ, Mehta S, Ahn J, Heterotopic ossification after central nervous system trauma -A current reviewBone Joint Res 2013 2(3):51-57. [Google Scholar]
[12]. Alfieri KA, Forsberg JA, Potter BK, Blast injuries and heterotopic ossificationBone Joint Res August. 2012 1:174-79. [Google Scholar]
[13]. Patil SG, Siddiqua A, Joshi UK, Deshmukh PK, Patil BS, Mangalgi A, Heterotopic Ossification: An Unusual PresentationCase Reports in Dentistry 2012 Article ID 516717, 4 pages, 2012. doi:10.1155/2012/516717 [Google Scholar]
[14]. Mavrogenis AF, Soucacos PN, Papagelopoulos PJ, Heterotopic Ossification RevisitedOrthopedics 2011 34(3):177 [Google Scholar]
[15]. Mishra MV, Austin L, Parvizi J, Ramsey M, Showalter TN, Safety and efficacy of radiation therapy as secondary prophylaxis for heterotopic ossification of non-hip jointsJ Med Imaging Radiat Oncol 2011 55:333-36. [Google Scholar]
[16]. Halas RA, Karuppiah S, Heterotopic ossification of the hip after strokeCurr Orthop Pract 2011 22:E19-E21. [Google Scholar]
[17]. Genêt F, Jourdan C, Schnitzler A, Troublesome heterotopic ossification after central nervous system damage: a survey of 570 surgeriesPloS One 2011 6:16632 [Google Scholar]
[18]. Rosin AJ, Ectopic calcification around joints of paralyzed limbs in hemiplegia, diffuse brain damage, and other neurological diseasesAnnals of the Rheumatic Diseases 1975 34:499-505. [Google Scholar]
[19]. Melamed E, Robinson D, Halperin N, Brain injury related heterotopic bone formation: treatment strategy and resultsAm J Phys Med Rehabil 2002 81:670-674. [Google Scholar]
[20]. Van Kuijk AA, Geurts ACH, van Kuppevelt HJM, Neurogenic heterotopic ossification in spinal cord injurySpinal Cord 2002 40:313-26. [Google Scholar]
[21]. Gardner MJ, Ong BC, Liporace F, Koval KJ, Orthopedic issues after cerebrovascular accidentAm J Orthop 2002 31:559-68. [Google Scholar]
[22]. Taly AB, Nair KP, Kumar MV, Heterotopic ossification in non-traumatic myelopathiesSpinal cord 1999 37:47-49. [Google Scholar]
[23]. Buring K, On the origin of cells in heterotopic bone formationClin Orthop 1975 110:293-301. [Google Scholar]
[24]. van Kuijk AA, Geurts ACH, van Kuppevelt HJM, Neurogenic heterotopic ossification in spinal cord injurySpinal Cord 2002 40:313-26. [Google Scholar]
[25]. Baron M, Stern J, Lander P, Heterotopic ossification heralded by a knee effusionJ Rheumatol 1983 10:961-64. [Google Scholar]
[26]. Zellig G, Zwecker M, Weingarden H, Wolf M, Heterotopic ossification of the vocal cords after spinal cord injurySpinal Cord Med 2007 30(5):518-20. [Google Scholar]
[27]. Nechwatal E, Early recognition of heterotopic calcification by means of alkaline phosphataseParaplegia 1973 11:79 [Google Scholar]
[28]. Furman R, Nicholas JJ, Jivoff L, Elevation of the serum alkaline phosphatase co-incident with ectopic bone formation in paraplegic patientsIbid 1970 52A:1131 [Google Scholar]
[29]. Chaco J, Wolf E, Subluxation of the gleno-humeral joint in hemiplegiaAmer. J. Phys. Med 1971 50:139 [Google Scholar]
[30]. Johnson JTH, Atypical myositis ossificationJ. Bone Jt Surg 1957 39A:189 [Google Scholar]
[31]. Lippman M, Heterotopic calcification-a problem in rehabilitation medicineArch. Phys. Med 1960 41:351 [Google Scholar]
[32]. Stover SL, Hataway CJ, Zieger HE, Heterotopic Ossification in spinal cord injury patientsArch Phys Med Rehabil 1975 56:199-204. [Google Scholar]
[33]. Russell RGG, Smith R, Bishop MC, Price DA, Squire CM, Treatment of myositis ossificans progressive with a diphosphonateLancet 1972 1:10 [Google Scholar]
[34]. Ritter MA, Indomethacin: An adjunct to surgical excision of immature heterotopic bone formation in patient with severe head injuryOrthopedics 1987 10:1379-81. [Google Scholar]
[35]. Garland DE, Blum CE, Water RL, Periarticular heterotopic ossification in head injured adults: incidence and locationJ Bone Joint Surg 1980 62:1143-46. [Google Scholar]
[36]. Mital MA, Garber JE, Stinson JT, Ectopic bone formation in children and adolescents with head injuries: its managementJ Pediatr Orthop 1987 7:83-90. [Google Scholar]
[37]. Ayers DC, Evarts CM, Parkinson JR, The prevention of heterotopic ossification in high risk patients by low dose radiation after total hip arthroplastyJ Bone Jt Surg 1986 68:1423-30. [Google Scholar]
[38]. Maheswarappa BM, Nair KPS, Taly AB, Heterotopic Ossification at unusual site in traumatic brain injuryIJPMR 2004 15:34-37. [Google Scholar]