Radiation Induced Sarcoma of Oral Cavity-A Rare Case Report and a Short Review
Sivaraman Ganesan1, Elizabeth Mathew Iype2, Aravind S. Kapali3, Renu S.4
1 Fellow in Head and Neck, Department of Surgical Oncology, Regional Cancer Center, Trivandrum, India.
2 Additional Professor, Department of Surgical Oncology, Regional Cancer Center, Trivandrum, India.
3 Mch Resident, Department of Surgical Oncology, Regional Cancer Center, Trivandrum, India.
4 Assistant Professor, Department of Pathology, Regional Cancer Center, Trivandrum, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sivaraman Ganesan, Fellow in Head and Neck, Department of Surgical Oncology, Regional Cancer center, Trivandrum, India.
Phone: 8592848732,
E-mail: gsivram@gmail.com
Radiation - Induced Sarcomas(RIS) are rare clinical entity. They arise from the previously irradiated areas with a prolonged latency period. In this case report we present a rare case of radiation induced sarcoma with a brief review of literature. We report radiation-induced sarcoma in a 67–year–old male, involving the left Retromolar Trigone region following treatment of squamous cell carcinoma of tongue with wide excision, neck dissection and post-operative radiation. Diagnosis of radiation induced sarcoma was confirmed by history, latency period and biopsy.
Radiation - Induced Sarcoma, Squamous cell carcinoma
Case Report
Radiation therapy is an adjuvant in treatment of many tumors. Second primary malignancy following radiotherapy is one of the late sequelae of radiation therapy, which is of concern in long term cancer survivors. We present an interesting & rare case of Radiation Induced Sarcoma (RIS) with a brief review of literature.
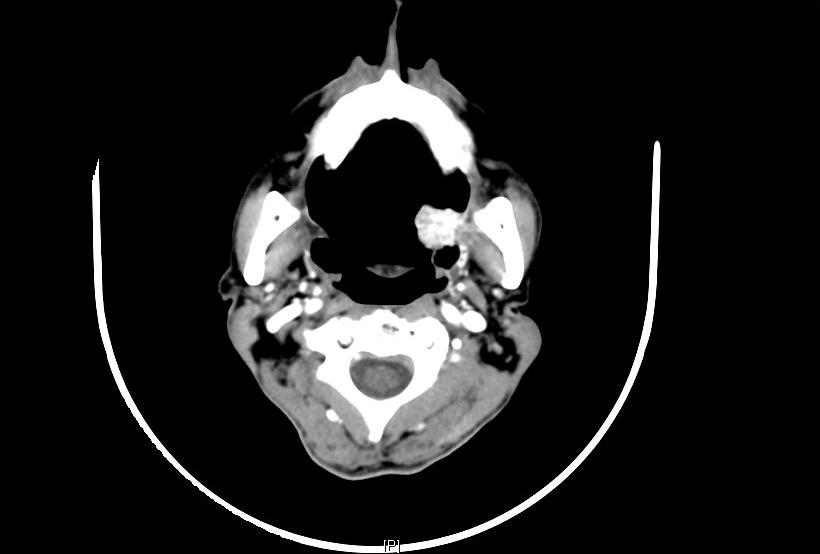
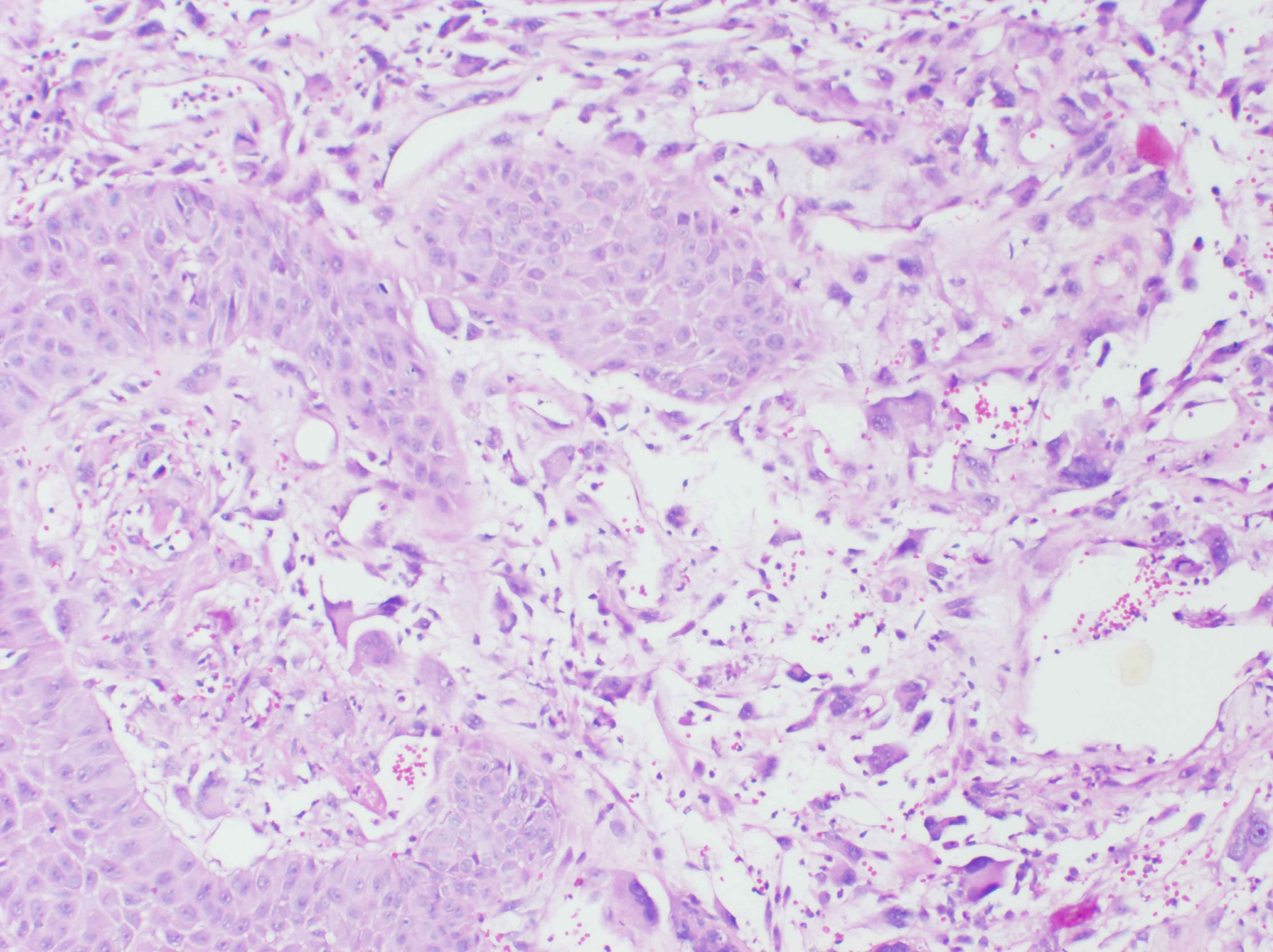
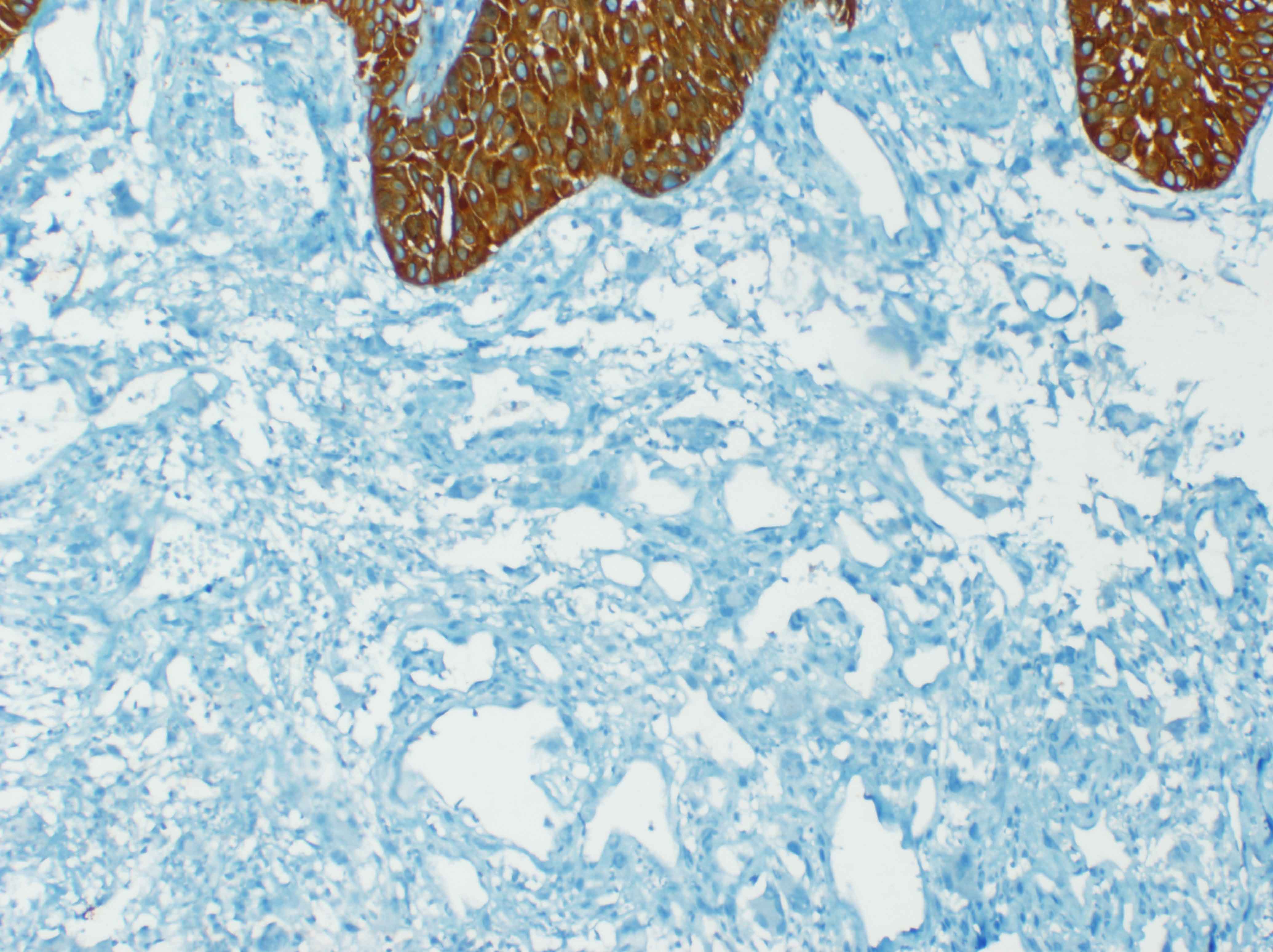
A 67 year male patient reported to Head and Neck Surgery OPD on February 2013 with history of a swelling on the left side of the oral cavity for the past one year. The swelling was insidious in onset, progressively increasing. He had no pain or no difficulty in opening the mouth. He had no history of neck swellings, voice change and respiratory difficulty. He had well differentiated squamous cell carcinoma of the tongue, T2N0M0 for which he underwent wide excision of left lateral tongue with primary closure followed by post-operative radiation of 50 Gy in 15 fractions at November 1994 in our institute. He was on regular followup and detected this swelling presently. He was disease free for a period of 18 years. Patient had no other significant medical illness or other relevant family history. On examination his general condition was fair, moderately built and nourished. Local examination revealed a large 4 x 4cm exophytic, reddish irregular polypoidal mass in the left retromolartrigone (RMT) region with areas of ulceration [Table/Fig-1]. On palpation, mass was firm, non-tender,pedunculated in the left retromolartrigone region. There was no other significant lesion in the oral cavity; initial operated site was normal with no significant induration. No regional lymphadenopathy was noted. Computed tomography (CT) [Table/Fig-2] scan of the lesion showed a large pedunculated lesion of size 2.7x 2x 2.5 cm lesion in the oropharynx originating probably from the left palatoglossal fold, protruding into the left tonsillar fossa. Soft and hard palate was not involved. The lesion is abutting the tip of the medial pterygoid muscle. Punch biopsy from the lesion showed tissue lined by hyperplastic squamous epithelium with sub-epithelium demonstrating infiltrating neoplasm composed of pleomorphic cells [Table/Fig-3] with moderate to abundant cytoplasm, round, irregular pleomorphic nuclei with nucleoli. Multinucleate tumor cells present. Cytokeratin [Table/Fig-4], EMA, HMB45 were negative, whereas Vimentin (mesenchymal tissue marker) [Table/Fig-5] and S-100 protein(nerve fiber) were strongly positive. With a history of pre-existing squamous cell carcinoma and radiation therapy and strongly positive vimentin, diagnosis of sarcoma is made. Treatment option of radical surgery with reconstruction was explained to the patient. As the patient wanted to be on follow up, he is being followed up regularly.
Clinical photograph showing large 4 x 4cm exophytic, reddish, firm irregular polypoidal mass in the left Retromolar Trigone (RMT) region with areas of ulceration

CT picture showing a large irregular heterogeneously enhancing mass lesion measuring approximately 27 x 20 x 25 mm is seen in the region of the left oropharynx. The lesion has a few foci of calcification within and a small stalk of origin, arising possibly from the palatoglossus fold protruding inferiorly into the left tonsillar fossa
Biopsy showing highly pleomorphic cells beneath the squamous epithelium (H&E × 200)
Vimentin positivity in neoplastic cells. Overlying Squamous epithelium is negative (IHC × 200)
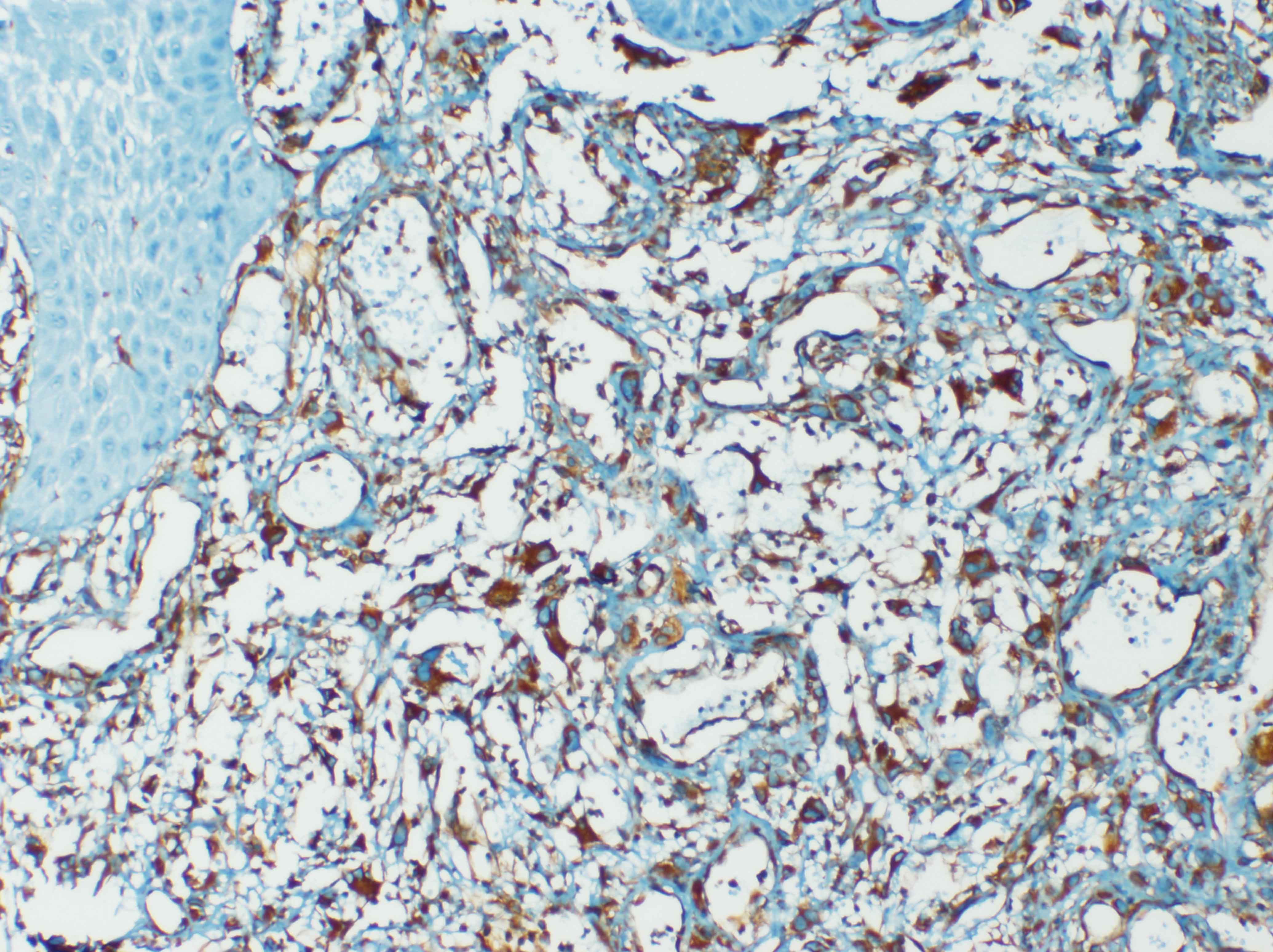
Cytokeratin stain: Neoplastic cells are negative, overlying squamous epithelium is positive (IHC ×200)
Discussion
Radiation induced sarcoma is a rare but recognised complication of radiotherapy and is associated with poor prognosis. In a review article on radiation induced sarcomas, Malcolm Feign [1] had summarized 10 reports totalling 14 000 patients, the reported incidence being 0.16%.
In 1948, Cahan et al., [2] proposed,the following criteria for the diagnosis of RIS:
Sarcoma must develop within the boundaries of a previously irradiated area;
Relatively long asymptomatic latent period (atleast 4 years) must have elapsed;
Sarcoma must have a different histology from the original lesion;
Sarcoma must be histologically confirmed.
These criteria were revised and updated by Murray et al., [3] in 1999:
History of irradiation with the sarcoma arising in the area included in the radiation field and the 5% isodose line;
No evidence that the sarcoma was present before the radiation therapy;
Sarcomas must be proven histologically and be of different pathology compared with the primary tumor.
The latency period for development of RIS is typically 5–20 years [2]. Consensus does not prevail to agree the duration of latency after radiation exposure.The sarcoma team at MSKCC suggests that a latency of six months is sufficient to affirm the diagnosis of RIS [4]. Our patient had alatency period of 18 years after the radiation exposure fitting in time frame of the latency duration.
Histologically, while examining the slides, the prior history of radiation appears to be the only clue to the pathologist in making the diagnosis, when an undifferentiated pattern is encountered. Such undifferentiated tumors were formerly included within the terms “malignant fibrous histiocytoma (MFH)” and “undifferentiated pleomorphic sarcoma (UPS)”, and now a separate soft tissue sarcoma category with an undifferentiated pleomorphic variant [5]. As per the Cahan’s or others modifications no specific histologic pattern is stamped for the diagnosis of Radiation induced sarcoma.
Risk factors for developing RIS are young age at treatment and treatment-related factors, including high radiation dose and simultaneous chemotherapy with alkylating agents [6]. Our patient had received a radiation of 50 Gy in 47 years of age. He did not receive any chemotherapy.Radiation above 50Gy cause cell death, while lower doses (<30Gy) cause genomic instability and damage cell repair mechanisms. RIS typically occur within or at the edges of the radiation field. At the edges of the radiation field, the dose of radiation is not homogeneous and may be less than the tumor killing dose. Our patient developed the tumor at the edge of the radiation field in the left palatoglossal fold, but well within the field of radiation.
Familial gastrointestinal stromal tumor syndrome (GIST), Li-Fraumeni syndrome, retinoblastoma, Werner syndrome,Neurofibromatosis Type 1, Costello Syndrome, and Nijmegen breakage syndrome are associated with increased risk of bone or soft tissue sarcoma, along with multiple other tumors [3]. Our patient did not undergo any genetic testing.
The MIB-1 score has been reported to be the most significant independent prognostic factor for soft tissue sarcoma. Zhengbo Wei et al., [7] in his immunohistochemical study of 13 patients of RIS sarcoma of head and neck region gave a conclusion that MIB-1 score may be used as a histological grading system for RISHN. Positive bcl-2 was observed in 12 (100%) and survivin in 10 (76.9%) patients. The Ki-67 labeling index ranged from 1% to 90%, and it showed significant positive correlation with mitosis count.
Surgery is the standard treatment for RIS [8]. It is very difficult for complete resection because of its proximity to vital organs in the head and neck. The prognosis of patients with incompletely excised tumors is much worse than that of patients with no residual tumor because of tumor insensitivity to chemo-and radiotherapy.
Our patient fulfills all the criteria for the establishment of RIS. The clinical diagnosis of RIS can be difficult because of induration and fibrosis within radiation field. Additional genetic testing will quantitate the prognosis of the patient. This patient is reported to emphasise the proper investigations based on the patient’s history & symptoms, especially the appearance or a change in the irradiated area, which can lead to an early diagnosis.
[1]. Should cancer survivors fear radiation-induced sarcomas? MALCOLM FEIGEN Sarcoma (1997) 1, 5± 15 [Google Scholar]
[2]. Cahan WG, Woodward HQ, Higinbotham NL, Stewart FW, Coley BL, Sarcomaarising in irradiated bone: report of eleven casesCancer 1948 1:3-29. [Google Scholar]
[3]. Murray EM, Werner D, Greeff EA, Taylor DA, Postradiation sarcomas: 20 cases and a literature reviewInt J RadiatOncolBiolPhys 1999 45:951-61. [Google Scholar]
[4]. Gladdy R. A., Qin L. X., Moraco N., Edgar M. A., Antonescu C. R., Alektiar K. M., Do radiation-associated soft tissue sarcomas have the same prognosis as sporadic soft tissue sarcomas?J ClinOncol 28 :2064-69. [Google Scholar]
[5]. Fletcher CDM, Chibon F, Mertens F, Undifferentiated/unclassified sarcomasIn: WHO classifiction of tumours of soft tissue and bone 2013 4thLyonIARC:236Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F. (Eds) [Google Scholar]
[6]. Virtanen A, Pukkala E, Auvinen A, Incidence of bone and soft tissue sarcoma after radiotherapy: a cohort study of 295,712 Finnish cancer patientsInt J Cancer 2006 118:1017-21. [Google Scholar]
[7]. Zhengbo Wei, Jian Xu, Xianjie Zeng, Radiation-induced Sarcoma in the Head and Neck Region: a Clinicopathologic and Immunohistochemical Study of 13 CasesAsian Pacific Journal of Cancer Prevention 2011 12:2995-99. [Google Scholar]
[8]. Xi M, Liu MZ, Wang HX, Radiation-induced sarcoma in patients with nasopharyngeal carcinoma: a single-institution studyCancer 2010 116:5479-86. [Google Scholar]