Neuroendocrine Carcinoma of Breast: A Rare Case Vignette
Nandeesh M.1, Anitha T.K.2, Shravan Rajpurohit3, Santosh R.4
1 Assistant Professor, Department of General Surgery, DMWIMS, Kerala, India.
2 Assistant Professor, Department of Microbiology, DMWIMS, Kerala, India.
3 Senior Resident, Department of General Surgery, DMWIMS, Kerala, India.
4 Senior Resident, Department of General Surgery, DMWIMS, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nandeesh M., #902, DMWIMS Doctors Quaters, Naseera Nagar, Meppadi, Wayanad, Kerala-673577, India.
Phone: 9544954402,
E-mail: nandums2009@gmail.com
Neuroendocrine tumour of breast is an extremely rare condition. It may present as focal neuroendocrine differentiation with other histological subtypes of breast cancer or primary neuroendocrine tumour of breast or a metastatic foci in breast. There are no radiologic or clinical signs specific to this subtype. With rarity of its occurrence and absence of randomised trials regarding neuroendocrine tumour of breast, very little is known about the behaviour, prognosis and proper management of this condition. Only the available case reports suggests the necessary strategies for optimal management of this minimally explored medical condition.
Neuroendocrine Carcinoma Breast, Immunohistochemistry, Chromogranin, Chemotherapy
Case Report
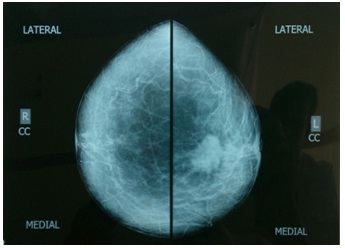
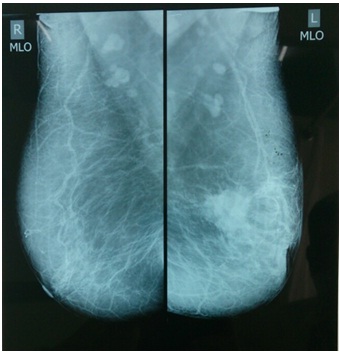
A 67-year-old post-menopausal female patient presented with lump in the left breast since six months with minimal pain. Clinical examination revealed a firm 5cms lump in the upper inner quadrant of left breast with nipple retraction. No signs of skin and chestwall involvement. Left axilla showed solitary lymphadenopathy. Subsequent work up was done with mammo & sonography which showed lesion suspicious of malignancy as in [Table/Fig-1] and [Table/Fig-2], FNAC showed Lobular Carcinoma. Further imaging and laboratory work up for metastasis was negative. The tumour was staged as T3N1MO StageIII and multimodality treatment with neoadjuvant chemotherapy 3 cycles followed by Left Modified radical mastectomy was done. Histopathology revealed, on gross examination the resected breast measured 15cms × 13cms × 5cms with a neoplasm measuring 2.5 cms × 3 cms × 3 cms, cut section appears brownish. Axillary pad of fat shows 10 lymph nodes, with largest one measuring 1 cm. Microscopic section from breast shows infiltration by a neoplasm arranged in solid sheets and lobules seperated by fibrovascular septae. Foci of necrosis were seen. The cells are round to oval with moderate amount of granular cytoplasm and round nuclei. The tumour cells show peripheral pallisading. Stroma shows lymphocytic infiltration. Deep resected margin is free of tumour. All lymphnodes showed reactive hyperplasia. Pathological diagnosis of Neuroendocrine carcinoma of breast was done which was subjected to Immunohistochemical studies.
Mammography-Craniocaudal view
Mammography-Mediolateral oblique
Immunohistochemistry
Showed Estrogen Receptor, Progesterone Receptor positive, strongly positive for Chromogranin and Her 2 Neu negative.
The patient received adjuvant chemotherapy, adjuvant radiotherapy and was started on hormonal therapy with tamoxifen (20mg/day). The patient is healthy and showed no recurrence or metastasis on follow up visit after 6 months.
Discussion
Breast is a rare site for Neuroendocrine tumour. Most neuroendocrine tumors are located in the gastrointestinal tract and the lung [1]. Neuroendocrine Carcinoma Breast (NECB) was originally described in 1963 by Feyrter et al., [2]. Primary neuroendocrine carcinoma of the breast is extremely rare and accounts for less than 5% of all cancers arising from the breast [3]. We are presenting a case of neuroendocrine carcinoma breast, to add better understanding & literature on this minimally explored & poorly understood clinical entity.
Neuroendocrine Carcinoma Breast is a surprise diagnosis to the pathologist. The WHO eventually proposed three histologic categories (solid carcinoid-like, large cell-type, and small/oat cell-type) In the WHO classification neuroendocrine tumors have been defined as those in which one or more neuroendocrine markers, such as Neuron specific enolase, chromogranin A, and/or synaptophysin, are expressed in at least 50% of cancer cells [4]. In addition to this, diagnosing primary NECB also requires fulfilling two other criteria: (1) other primary sites must be ruled out and (2) the tumor must show histological evidence of a breast in-situ component [5]. Morphologically, neuroendocrine carcinomas of the breast include solid neuroendocrine carcinoma, atypical carcinoid, small cell or oat cell carcinoma and large cell neuroendocrine carcinoma. The most helpful features are cellular monotony, nuclear palisading and pseudorosette formation [6]. Histologically describing the breast in-situ component is important because this determines which adjuvant treatment regimens are to be chosen. Simultaneous presence of an intra-ductal component and the absence of other primary sites establish the breast as the primary organ of origin [7,8]. Pathologists mainly rely on using a panel of the most sensitive and specific IHC neuroendocrine markers (chromogranin A or B and synaptophysin) [9]. The most important histological factor is the histological grade [10]. Prognosis seems to correlate with the stage of the disease at the time of presentation [11]. Since the significance of neuroendocrine differentiation in carcinomas of the breast remains unclear, they are treated in the classical manner [12].
Conclusion
Neuroendocrine carcinoma of breast is rare in its occurrence. The behaviour, treatment & prognosis of the disease is not completely understood. Our case report adds to the literature in managing the condition.
[1]. Modlin IM, Lye KD, Kidd M, A 5-decade analysis of 13,715 carcinoid tumorsCancer 2003 97:934-959.(PMID: 12569593) [Google Scholar]
[2]. Feyrter F, Harmann G, On the carcinoid growth form of the carcinoma mammae, especially the carcinoma solidum (gelatinosum) mammae (in German)Frankf Z Pathol 1963 73:24-39. [Google Scholar]
[3]. Tavassoli FA, Devilee P, Pathology and genetics. In: Tumors of the Breast and Female Genital OrgansWHO Classification of Tumors Series 2003 Lyon, FranceIARC Press:32-34. [Google Scholar]
[4]. Ellis P, Schnitt SJ, Sastre-Garau X, Invasive breast carcinomaIn Pathology and genetics: tumors of the breast and female genital organs 2003 4th editionLyonWorld Health Organization:32-34.Edited by Tavassoli FA, Devilee P. [Google Scholar]
[5]. Kinoshita S, Hirano A, Komine K, Kobayashi S, Kyoda S, Takeyama H, Primary small-cell neuroendocrine carcinoma of the breast: report of a caseSurg Today 2008 38:734-38. [Google Scholar]
[6]. Tsang WY, Chan JK, Endocrine ductal carcinoma in situ (E-DCIS) of the breast. Form of low-grade DCIS with distinctive clinicopathologic and biologic characteristicsAm J Surg Pathol 1996 20:921-43. [Google Scholar]
[7]. Alkaied H, Harris K, Azab B, Dai Q, Primary neuroendocrine breast cancer, how much do we know so far?Med Oncol 2012 29:2613-18. [Google Scholar]
[8]. Hoang MP, Maitra A, Gazdar AF, Albores-Saavedra J, Primary mammary small-cell carcinoma: a molecular analysis of 2 casesHum Pathol 2001 32:753-57. [Google Scholar]
[9]. Righi L, Sapino A, Marchio C, Papotti M, Bussolati G, Neuroendocrine differentiation in breast cancer: established facts and unresolved problemsSemin Diagn Pathol 2010 27:69-76. [Google Scholar]
[10]. McIntire M, Siziopikou K, Patil J, Gattuso P, Synchronous metastases to the liver and pancreas from a primary neuroendocrine carcinoma of the breast diagnosed by fine needle aspirationDiagn Cytopathol 2008 36:54-57. [Google Scholar]
[11]. Papotti M, Macri L, Finzi G, Neuroendocrine differentiation in carcinomas of the breast: a study of 51 casesSemin Diagn Pathol 1989 6:174-188.(PMID: 2503862) [Google Scholar]
[12]. David O, Bhattacharjee M, Diffuse neuroendocrine differentiation in a morphologically composite mammary infiltrating ductal carcinoma: a case report and review of the literatureArch Pathol Lab Med 2003 Mar 127(3):e131-4.(PMID: 12653600) [Google Scholar]