Hepatic and Adrenal Hemangioendothelioma-A Case Report
Sulata M Kamath1, H.K. Nagaraj2, Vijaya V Mysorekar2
1 Professor, Department of Pathology, M S Ramaiah Medical College and Hospitals, M.S.R Nagar, M.S.R.I.T post, Bangalore - 560054, India.
2 Professor & HOD, Department of Urology, M S Ramaiah Medical College and Hospitals, M.S.R Nagar, M.S.R.I.T Post, Bangalore - 560054, India.
3 Professor, Department of Pathology, M S Ramaiah Medical College and Hospitals, M.S.R Nagar, M.S.R.I.T Post, Bangalore - 560054, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sulata M. Kamath, 38,18th Cross Road, Malleswaram west, Bangalore-560055, India.
Phone: 9343045565,
E-mail: drsmkamath@gmail.com
Haemangioendothelioma (HE) liver is a mesenchymal vascular tumour, intermediate between a haemangioma and an angiosarcoma. It has a variable clinical course, is a low grade malignancy and is associated with long-term survival. It has a characteristic histologic appearance. Immunohistochemical studies have shown that the neoplastic cells in HE are of endothelial derivation. These are essential to distinguish HE from metastatic carcinoma and primary epithelial liver tumour. We report a case of a 36-year-old male with HE of the liver with adrenal involvement, probably metastatic, with tuberculosis as an incidental finding. To our knowledge this is the first such case reported in literature. The confirmation of diagnosis was done by immunohistochemical study.
Liver tumours, Vascular tumours
Case Report
A 36-year-old male patient was admitted with complaints of dull, aching pain in the right loin for 3 months. He also had history of fever, weight-loss and loss of appetite. The ultrasonographic (USG) examination of abdomen and pelvis revealed moderate hepatomegaly with an ill-defined, lobulated hypoechoic lesion in the left lobe of liver measuring 8.5x7.2 cm. Multiple hypoechoic lesions were seen in both the lobes. Also seen was a hyperechoic lesion about 3.5 cms in the posterosuperior portion of the right lobe of the liver. There was splenomegaly with multiple hypoechoic focal lesions measuring 8-15 mm. Para-aortic lymphadenopathy was seen. CT scan with contrast confirmed the USG findings with multiple heterogenous hypoattenuated areas in the liver and the spleen. In addition an irregular, globular area of heterogenous hypoattenuations, 3.05x 2.32 cm in size was seen involving the right adrenal gland. Para-aortic lymphadenopathy was noted bilaterally. The differential diagnoses were:
Hepatosplenomegaly with multiple abscesses of probable infective origin (amoebic),
Right adrenal adenoma / phaeochromocytoma with secondaries in liver,
Retroperitoneal lymphadenopathy.
The 2-D Echocardiogram, colour doppler studies, urinary vanylmandelic acid level (4.87 mg/day) and haematology parameters were normal. Biochemical parameters were normal except for serum alkaline phosphatase which was elevated to 142 U/L. Serum C-reactive protein was elevated to 6.23 mg / dL (normal < 0.5 mg/dL). Chest X-ray revealed prominent bilateral bronchovascular markings.ESR was elevated (25 mm at the end of one hour). Antibodies to human immunodeficiency viruses 1 and 2, hepatitis B virus, and hepatitis C virus were absent.
The patient underwent laparoscopic right adrenalectomy. Intra-operative findings were mild enlargement of the adrenal glands, multiple enlarged peri-venacaval lymph nodes, multiple hepatic subcapsular nodules and adhesions between the liver and right adrenal gland. The resected right adrenal gland and biopsy specimen of the hepatic nodules were subjected to histopathologic examination.
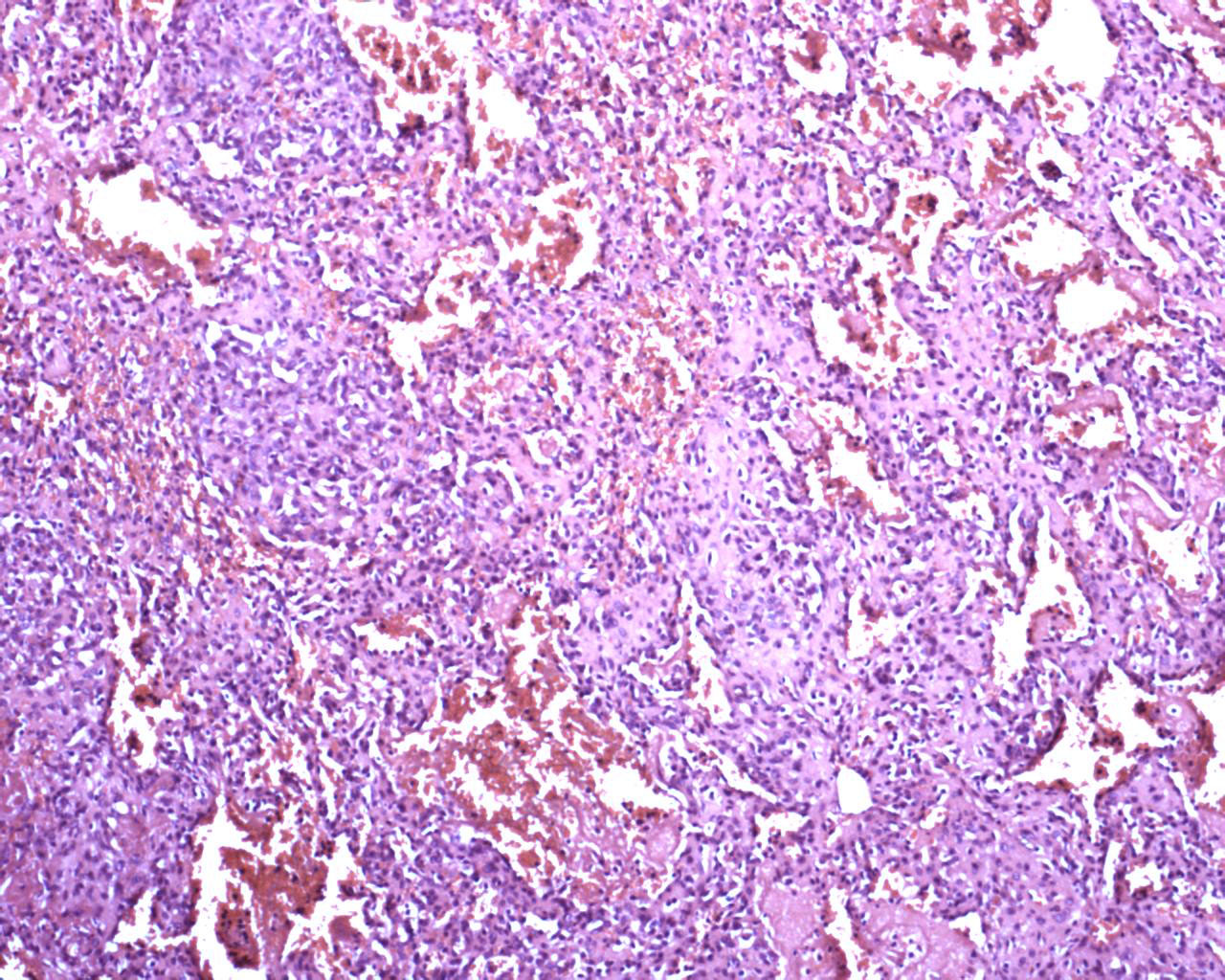
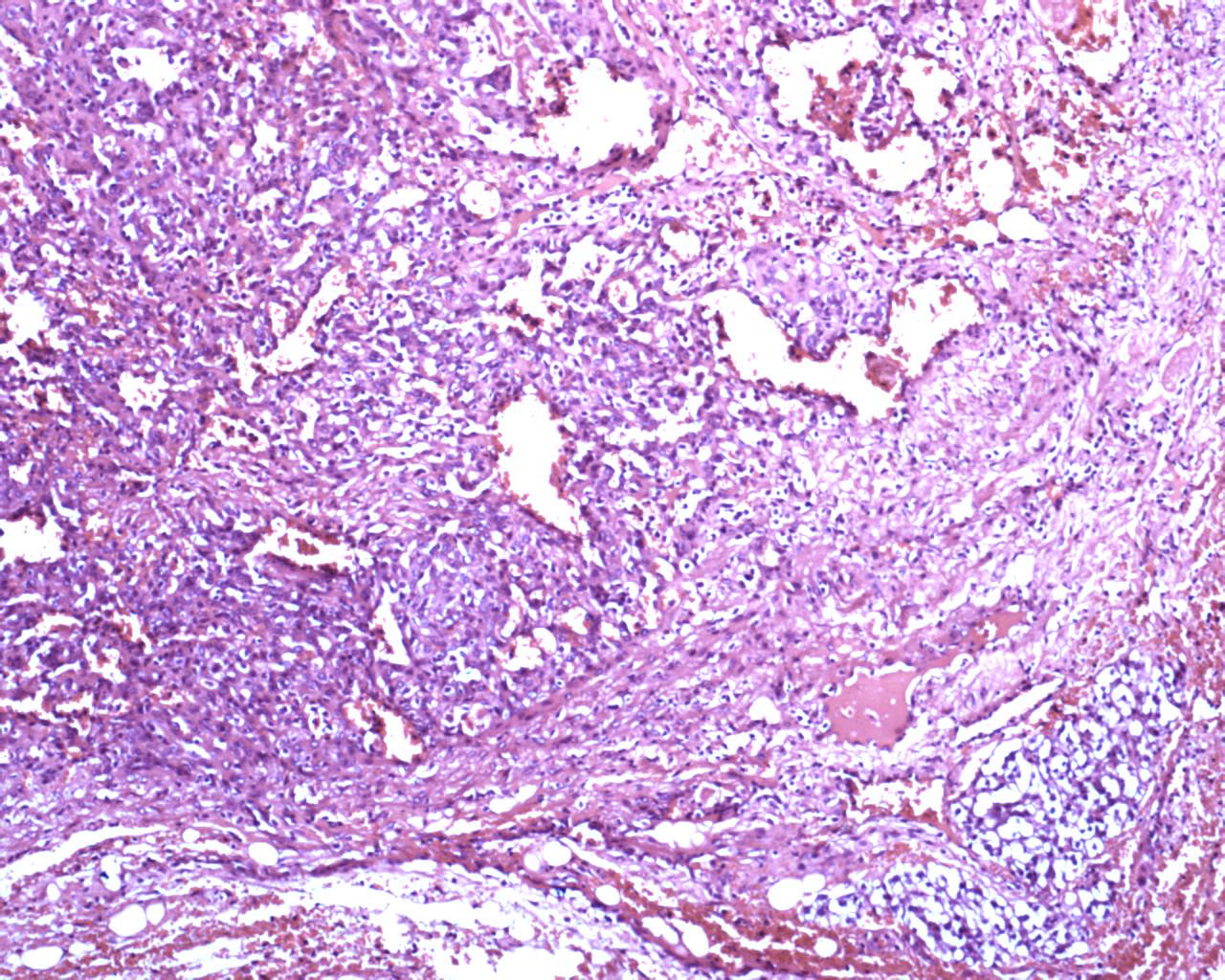
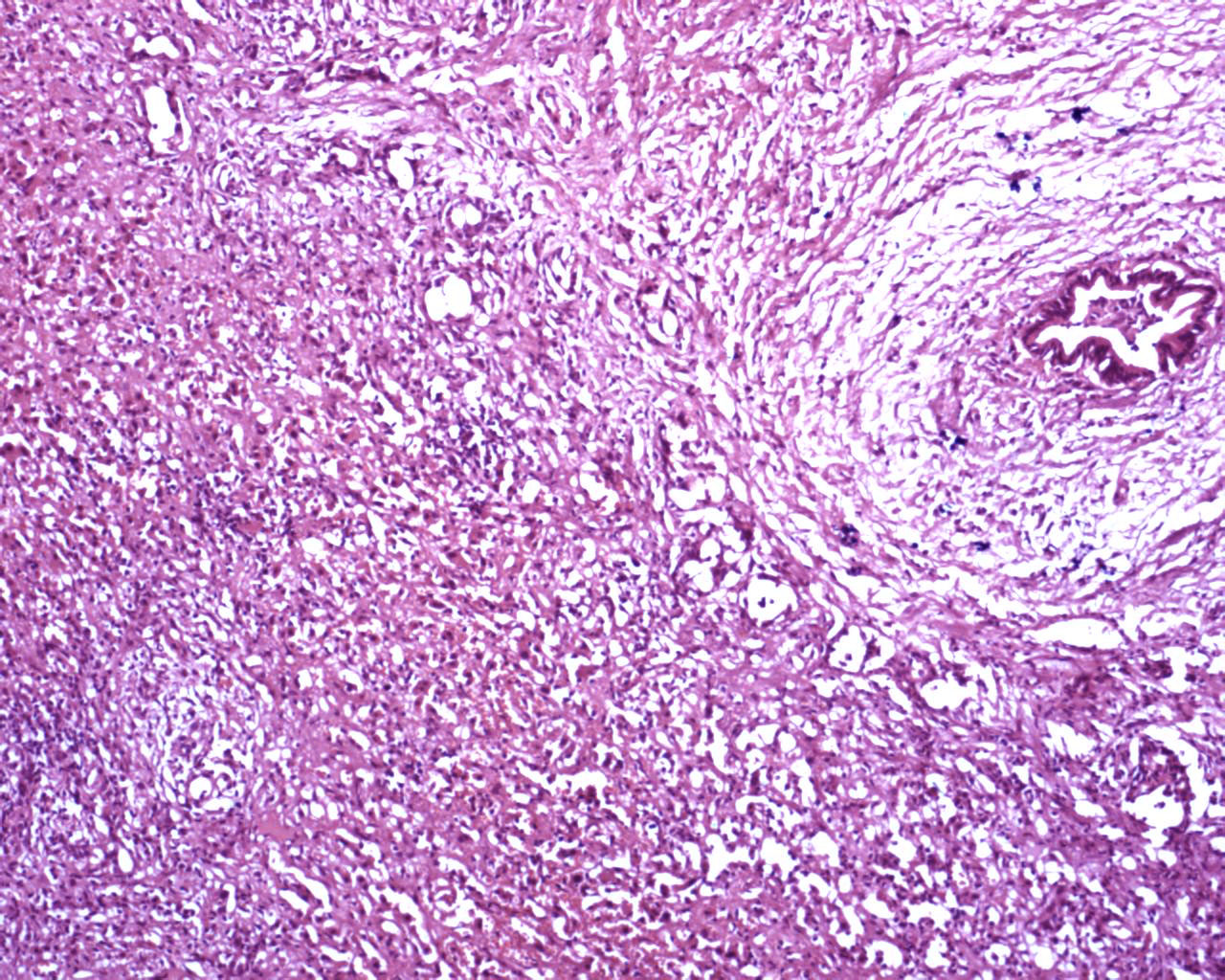
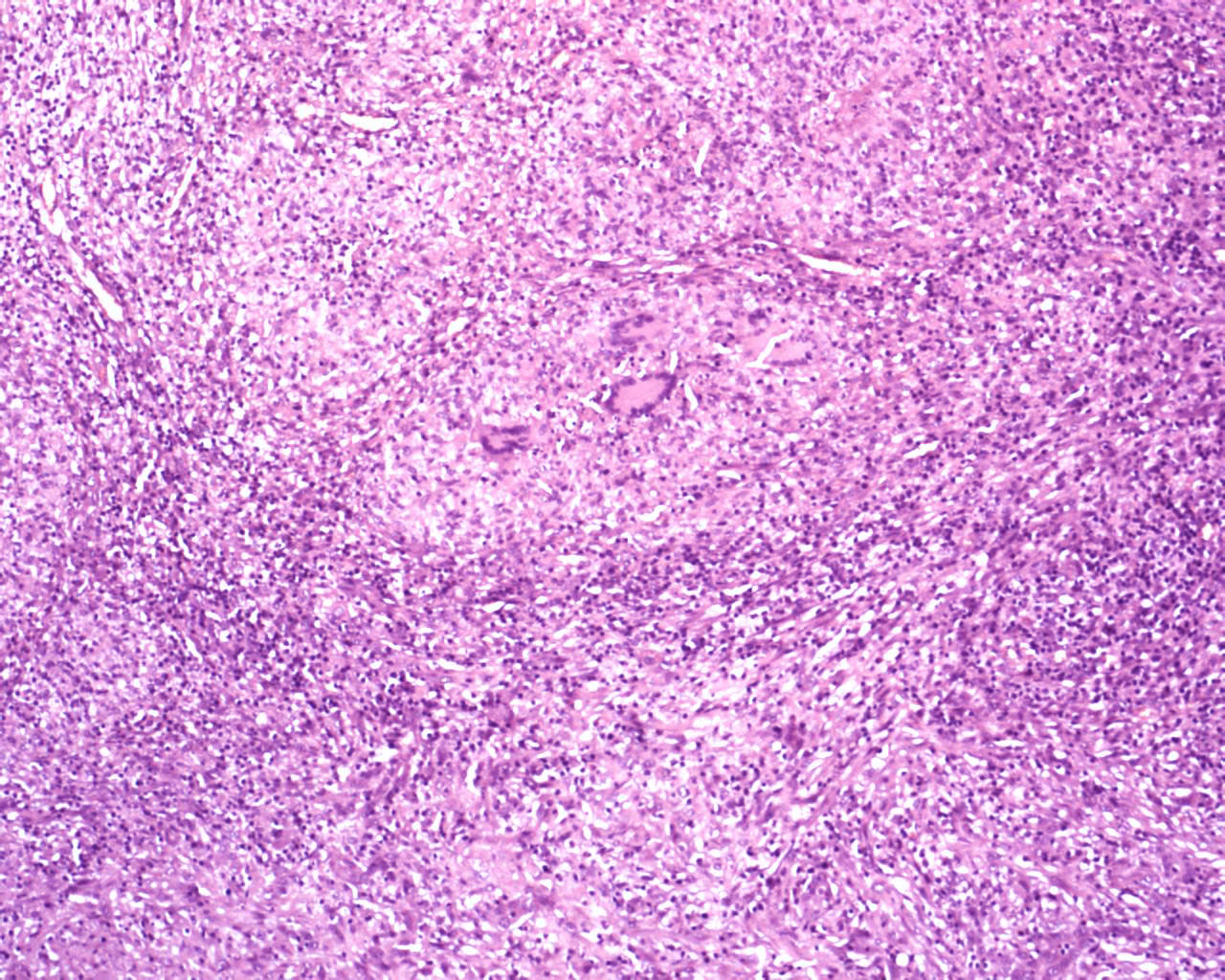
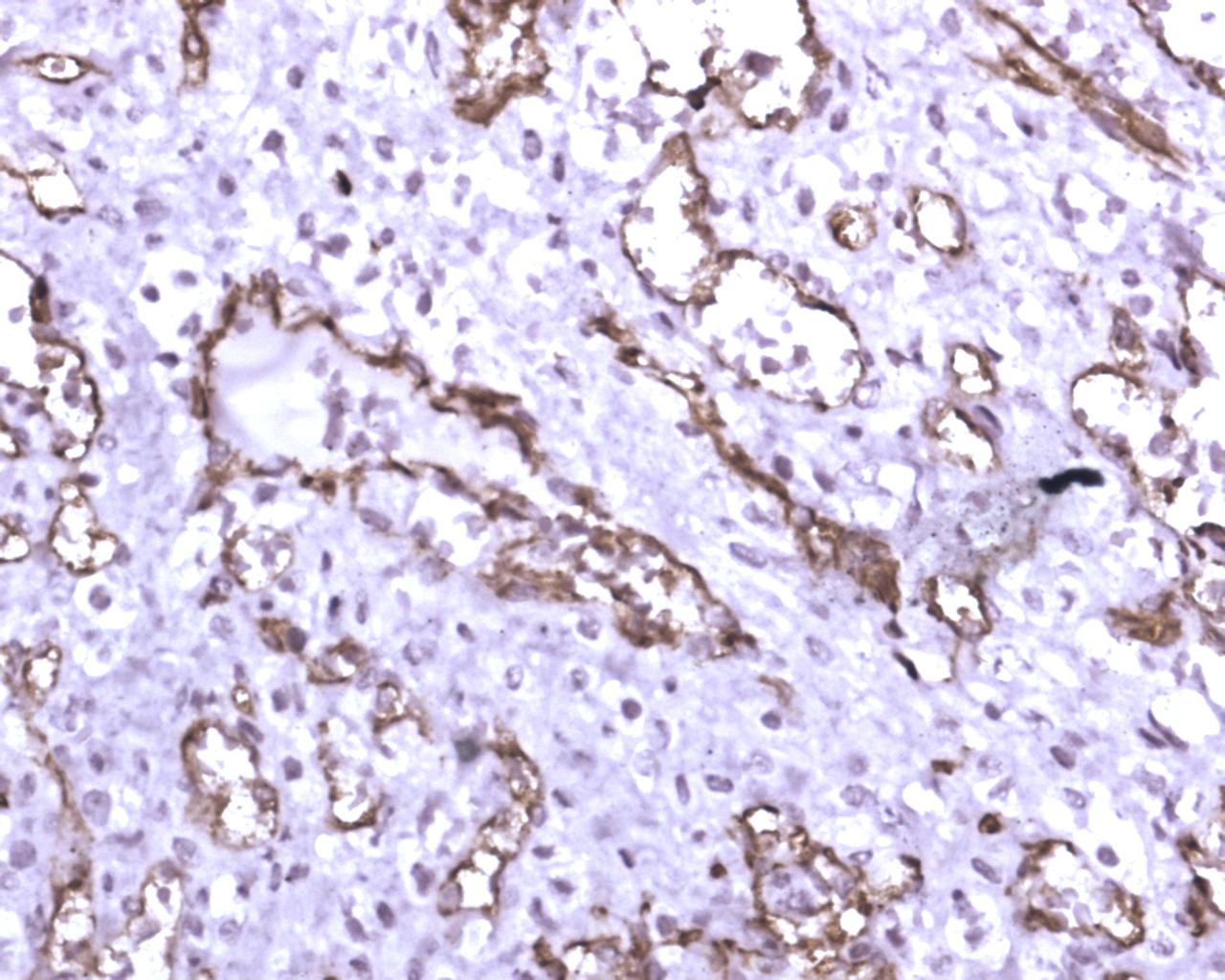
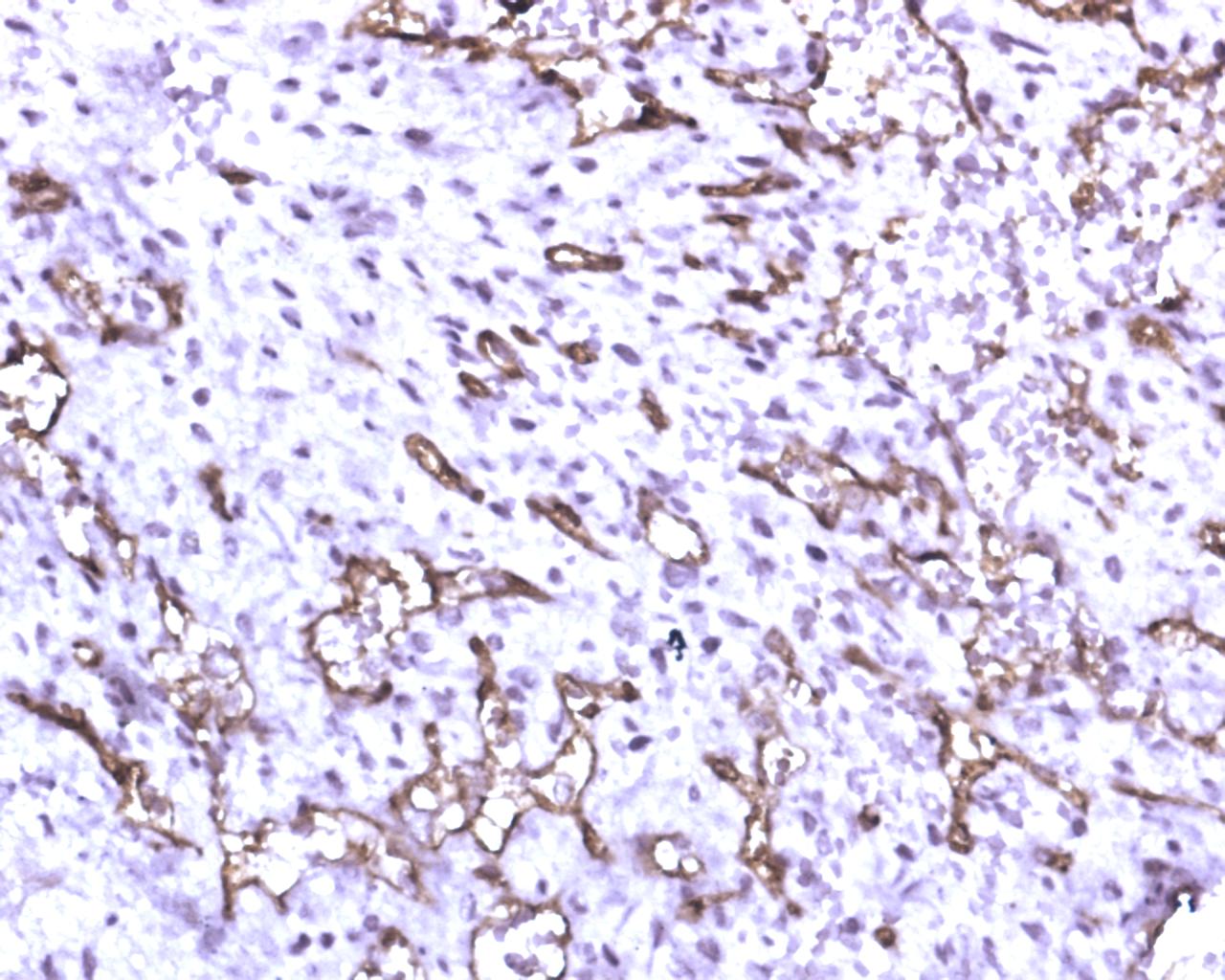
Histopathology revealed liver tissue with distorted architecture and dilated sinusoids [Table/Fig-1]. There were multiple ill-defined aggregates of proliferated blood vessels lined by mildly pleomorphic endothelial cells. These were surrounded by proliferated fibrous tissue [Table/Fig-2,3]. Foci of epithelioid granulomas with Langhans giant cells were seen [Table/Fig-4]. The adrenal gland showed a vascular lesion with similar morphology as in the liver. Some of the vascular spaces contained thrombi. The differential diagnosis was between HE and a low grade angiosarcoma. Immunohistochemistry revealed positivity for CD34 and CD31 in the hepatic and adrenal lesions [Table/Fig-5,6]. In view of mitotic rate of 1-2 / hpf, a final diagnosis of epithelioid HE with atypical morphology was confirmed. This could either be a multicentric primary lesion involving both the liver and right adrenal gland or a primary liver lesion with metastasis to the right adrenal gland. In addition, the granulomatous inflammation in the liver was diagnosed as tuberculosis.
Photomicrograph showing liver tissue with a tumour composed of multiple vascular spaces filled with blood (H & E, X 100)
Photomicrograph showing proliferated blood vessels lined by atypical endothelial cells in the tumour (H & E, X 100)
Photomicrograph of a bile ductule and an adjacent encapsulated tumour showing vascular aggregates (H & E, X 400)
Epithelioid cell granulomas in the adjacent liver parenchyma (H & E, x 400)
Immunohistochemistry showing CD 34 positivity in the tumour cells in the liver (X 200)
Immunohistochemistry showing CD 34 positivity in the tumour cells in the adrenal gland (X 200)
Subsequently, re-biopsy of another liver nodule and interaortocaval lymph nodes done revealed caseating tuberculosis. Although the splenic and vertebral lesions were not biopsied, they are most likely to be tuberculous. Priority was given to the treatment of tuberculosis, considering the patient’s debility, and he was started on anti-tuberculous treatment. No immediate treatment for the vascular lesions was started as these appeared to be asymptomatic at present. The patient is doing well and has symptomatic recovery during the two year follow-up period. A repeat scan revealed persistence of the vascular space occupying lesion in liver and adrenals with regression of lymphnodes.
Discussion
Haemangioendothelioma (HE) is a rare vascular tumour which exhibits behaviour similar to that of a benign haemangioma and an aggressive angiosarcoma [1]. Typically, adults are affected. Generally, neither abnormal liver biochemical parameters nor increased tumour markers are observed. Epithelioid HE, first described in soft tissue by Weiss and Enzinger in 1982, is a rare vascular endothelial tumour of unknown aetiology and variable clinical course [2]. HE was first described in the liver by Ishak in [2]. Besides characteristic histomorphologic features, diagnosis is confirmed by immunohistochemistry for endothelium-specific markers CD 34, CD 31 or factor VIII. Due to variable clinical presentation it is crucial to confirm the histopathological diagnosis to prevent missed or delayed diagnosis. It is essential to rule out extrahepatic metastasis as it has significant implications on the type of treatment to be adopted for the patient. Tumour dissemination to organs e.g. liver, lung, bone, brain, spleen, peritoneum, diaphragm, meninges, breast, head and neck, lymph nodes, heart, stomach and soft tissue is seen in 30-40% of cases [2].
In the largest reported series of 137 cases of liver epithelioid HE from the Armed Forces Institute of Pathology, the patients ranged in age from 12to 86 years with 61% females and 39% males [3]. Ours is a 36-year old male. There are no clear risk factors for the development of HE although liver trauma, hormones, vinyl chloride, asbestos, thorotrast contrast, alcohol and viral hepatitis may be implicated [4]. Serafinska et al mention dietary failure and alcoholic intake to be factors inducing tumour progression [4]. In our case, the patient had disseminated tuberculosis with associated dietary failure which might have been responsible for progression of the HE. Patients are either asymptomatic or have right upper quadrant pain. Other symptoms include jaundice, weight loss, fatigue, ascites, hepatomegaly and fever. In our case, the patient had dull aching abdominal pain, fever, loss of appetite and weight which could be attributed to systemic tuberculosis. Patients with HE have hypoechoic nodules differing in size. The histopathologic criteria are proliferated vascular channels containing red blood cells, lined by atypical endothelial cells; presence of myxomatous to densely fibrotic stroma. Hala et al reported a series of 32 cases with HE [5]. They concluded that the histology of the tumour, nuclear pleomorphism and mitotic count are of no value in predicting the clinical outcome. High cellularity is an unfavourable prognostic parameter as mitotic counts are often quite low in both low grade and aggressive tumours. Lack of cellular atypia and absence of anastomosing vascular channels in our case do not support a diagnosis of angiosarcoma. Progressive fibrosis observed at the edge of the HE lesions may limit tumour growth, which could account for the long term survival [6]. In our case, the above mentioned microscopic features were identified. In our immunohistochemical study, majority of the tumour cells were positive for CD31 and CD34.
The natural evolution of this tumour is from a well-defined nodular form to a diffuse multinodular form [7].The clinical course and prognosis are unpredictable.
Despite no treatment or after orthotopic liver transplant with positive lymph nodes or vascular invasion, long term survival has been reported and some cases of spontaneous regression of the lesion have been reported [8]. Without treatment, 5-year survival rates vary widely from 28%-67%. In contrast, in some cases, rapid tumour progression has been encountered with subsequent liver failure and death. There are no clinical or histological criteria for predicting evolution of the disease. Although, the tumour is considered malignant it carries a better prognosis compared to other hepatic malignancies, even in the presence of distant metastases and it is therefore, important to distinguish between them.
[1]. Yoshitaka Kurisu, Motonu Tsuji, Hiroko Kuwabara, Yuro Shibayama, Characteristic Cytologic Findings of Epithelioid Hemangioendothelioma : A Case Report and Review of LiteratureDiagn. Cytopathol 2011 39:1245 [Google Scholar]
[2]. Lauffer Jorg M, Zimmerman Arthur, Krahenbuhl Lukas, Triller Jurgen, Baer Hans U, Epithelioid Hemangioendothelioma of the Liver. A Rare Hepatic TumourCancer 1996 78:2318-27. [Google Scholar]
[3]. Soslow Robert A, Yin Polly, Steinberg Charles R, Yang Grace C.H, Cytopathologic Features Of Hepatic Epithelioid HemangioendotheliomaDiagn.Cytopathol 1997 17:50-3. [Google Scholar]
[4]. Serafinska Sylvia, Smolinski Patryk, Inglot Malgorzata, Krysztof Simon, Fulminant Hemangioendothelioma course - a case reportE & C Hepatology 2005 1(2):113-16. [Google Scholar]
[5]. Makhlouf Hala R, Ishak Kamal G, Goodman Zachary D, Epithelioid Hemangioendothelioma of the liver. A Clinicopathologic Study of 137 CasesCancer 1999 85:562-82. [Google Scholar]
[6]. Mosoia Liviu, Jean-Yues Mabrut, Mustapha Adham, Olivier Boillot, Christian Ducerf, Christian Partensky, Hepatic Epithelioid HemangioendotheliomaJournal of Surgical Oncology 2008 (98):432-37. [Google Scholar]
[7]. Maret-Pierre Bralet, Benoit Terris, Valerie Vilgrain, Laurence Bregland, Georges Molas, Michele Corbic, Epithelioid Hemangioendothelioma, Multiple Focal Nodular Hyperplasias, and Cavernous Hemangiomas of the Liver. An Unusual AssociationArch Pathol Lab Med. 1999 123:846-49. [Google Scholar]
[8]. Menahem Ben-Hain, Sasan Roayaie, Ming Q, Ye Swan N Thung, Sukru Emre, Thomas A, Fishbein. Hepatic Epithelioid Hemangioendothelioma: Resection or Transplantatation, Which and When?Liver Transplantation and Surgery November 1999 vol.5(No.6):526-31. [Google Scholar]