Diabetic Foot Ulcer Due to Scedosporium Apiospermum
Vijaya D.1, Nagaratnamma T.2, Sathish JV.3
1 Professor & HOD, Department of Microbiology, AIMS, BG, Nagara–571448, Karnataka, India.
2 Professor, Department of Microbiology, B & L.C.Hospital Bangalore, India.
3 Assistant Professor, Department of Microbiology, AIMS, BG, Nagara–571448, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vijaya D., Professor & HOD, Department of Microbiology, AIMS, BG, Nagara–571448, Karnataka, India.
Phone: 94820 09120,
E-mail: vijayadanand@rediffmail.com
We report a case of diabetic foot ulcer caused by Scedosporium apiospermum in a seventy year old male patient with uncontrolled diabetes. Scedosporium apiospermum, the asexual phase of Pseudallescheria boydii a fungus isolated from a variety of natural substrates throughout the world including soil, polluted water, sewage and manure of poultry and cattle. P.boydii is now recognized as a medically important opportunistic fungus. This case has been reported for its rarity.
Scedosporium apiospermum, Diabetic foot, Pseudoallescheria boydii
Introduction
Scedosporium apiospermum, the anamorphic form of Pseudallescheria boydii, is a filamentous fungus with low inherent virulence, increasing number of cases of this infection have been reported probably related to rising number of immunosuppressed persons. Apart from mycetoma, cutaneous and subcutaneous infection is rarely encountered in clinical practice [1]. P. boydii is now recognized as a medically important opportunistic fungus. S.apiospermum is reported to cause endocarditis, osteomyelitis, and arthritis primarly in previously normal patient. S.apiospermum was first described as a human pathogen in 1911 by Saccardo from a case of mycetoma in Italy [2].
Case Report
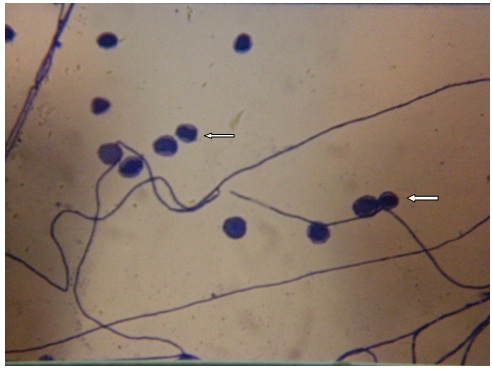
A seventy year old diabetic male patient since 10 years, agriculturist by occupation, presented with history of an ulcer of right great toe since one year, was referred to the department of Microbiology from surgical OPD of B & L C Hospital Bangalore, India. History of trauma for the first time to the right great toe while working in the field. On physical examination, patient was afebrile, normal built. All systems were normal. Local examination- ulcer over right great toe involving the skin, subcutaneous tissue and muscle but not the bone. Mycetoma was ruled out as there were no features like tumefaction, discharging sinus and granules from the ulcer. Routine investigation showed random blood sugar level 300 mg/dl, fasting blood sugar 210 mg/dl, VDRL non-reactive and HIV negative. Swabs from the lesion were collected and processed in the department of Microbiology. Gram stain showed occasional pus cells and no bacteria. KOH mount- presence of septate hyaline hyphae. Acid fast stain was negative for acid fast bacilli. Bacterial culture for aerobes & anaerobes- no bacterial growth seen. Two sets of Sabouraud dextrose agar (SDA) tubes were inoculated. One set was incubated at room temperature and other at 370C. After 3 days SDA slope incubated at 370C showed, grayish white filamentous fungal growth. There was no growth in the SDA slope incubated at room temperature. Similar growth was seen on blood agar and chocolate agar at 370C. Slide culture showed presence of septate hyphae with unicellular oval conidia borne singly on the conidiophores [Table/Fig-1]. The fungus was inoculated on cornmeal agar to look for P. boydii, the telemorph (sexual) stage of S.apiospermum. The isolate did not show the sexual stage. The fungus was identified S.apiospermum, the asexual stage of P. boydii. Repeat culture from the lesion yielded the same fungus. Patient refused for admission and was then lost for follow up.
Lactophenol cotton blue preparation showing septate hyphae with unicellular oval conidia, born singly at the end of the conidiophores (40X)
Discussion
P.byodii is the major etiologic agent of eumycotic mycetoma in United States and Europe. In India, mycetoma is distributed widely in different geographical areas eg., large number of mycetoma cases are seen in Tamil Nadu, India, the most Southern part and Rajasthan, India, the dry western part of India. The mycetoma is more prevalent in developing countries as compared to developed countries and the incidence is more in rural than urban areas. The prevalence of etiological agents of mycetoma varies from place to place. The eumycetoma accounts for about 40% and actinomyces 60% of mycetoma in the world. In Southeast Asia, India and Pakistan eumycotic and actinomycotic mycetoma ratio is 35% and 65%. In India, Rajasthan eumycetoma is more prevalent, where as actinomycetoma is more common in south India [3].
S. apiospermum is the asexual form of P. boydii and there is no difference in their virulence. Infection with this fungus has increased in patients with severe systemic disorders and in those who have received immunosuppressive therapy, such as corticosteroids [4]. In recent years it has been shown to be pathogenic for both immunocompetent and immunosuppressed patients [5]. In the present case, patient had uncontrolled diabetes with history of trauma leading to diabetic foot ulcer. Other cases reported in literature are S. apiospermum causing thyroid abscess, brain abscess with chronic suppurative otitis media and Keratomycosis [5–7]. In-vitro antifungal activity was not determined for the present isolate. Other studies indicate that azoles have significant antifungal activity, except fluconazole and ketoconazole on S. apiospermum [8]. Early identification of the fungi and proper antifungal therapy depending on clinical response can be helpful in the treatment of infections due to S.apiospermum. This case has been reported for its rarity.
[1]. Chaveiro MA, Vieira R, Cardoso J, Afonso A, Cutaneous infection due to Scedosporium apiospermum in an immunosuppressed patientJ Eur Acad Dermatol Venereol 2003 Jan 17(1):47-49. [Google Scholar]
[2]. Kwon-Chung KJ, Bennett JE, Pseudallescheriasis and Scedosporium infections (allescheriosis,petrielliosis, monosporiosis, scedosporiosis)Medical Mycology 1992 2nd edPhiladelphiaLea and Febiger:678-94. [Google Scholar]
[3]. Chander J, Textbook of Medical Mycology 2009 3rd edNew Delhi, IndiaMehta:422-33. [Google Scholar]
[4]. Kusuhara M, Hachisuka H, Lymphocutaneous infection due to Scedosporium apiospermumInt J Dermatol 1997 36:677-99. [Google Scholar]
[5]. Sireesha P, Kumar Manoj CH, Setty CR, Thyroid abscess due to Scedosporium apiospermumIndian J Med Microbiol 2010 28(4):409-11. [Google Scholar]
[6]. Acharya A, Ghimire A, Khanal B, Bhattacharya S, Kumari N, Kanungo R, Brain abscess due to Scedosporium apiospermum in a non- immunocompromised childIndian J Med Microbiol 2006 24(3):231-32. [Google Scholar]
[7]. Nath R, Gogoi RN, Saikia L, Keratomycosis due to Scedosporium apiospermumIndian J Med Microbiol 2011 28(4):414-15. [Google Scholar]
[8]. Cortez KJ, Roilides E, Quiroz-Telles F, Meletiadis J, Antachopoulos C, Knudsen T, Infections caused by Scedosporium sppClin Microbiol Rev 2008 January 21(1):157-97. [Google Scholar]