Bilateral Acute Epidural Hematoma with Good Outcome
Wellingson Silva Paiva1, Almir Ferreira De Andrade2, Aderaldo Costa Junior Alves3, Iuri Neville Ribeiro4, Manoel Jacobsen Teixeira5
1 Faculty, Division of Neurosurgery – University of Sao Paulo Medical School, Brazil.
2 Faculty, Division of Neurosurgery – University of Sao Paulo Medical School, Brazil.
3 Faculty, Division of Neurosurgery – University of Sao Paulo Medical School, Brazil.
4 Faculty, Division of Neurosurgery – University of Sao Paulo Medical School, Brazil.
5 Faculty, Division of Neurosurgery – University of Sao Paulo Medical School, Brazil.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Wellingson Silva Paiva, Enéas Carvalho de Aguiar Street, 255, Office 4080. Zipcode 5403-010 – São Paulo, SP, Brazil.
E-mail: wellingsonpaiva@yahoo.com.br
Epidural haematomas are one of the most common complicated closed-head injuries, but they, rarely show any bilateral localization. We are reporting here a case of a man found unconscious with Glasgow Coma Scale score; 8/15. Computed tomography of skull revealed bilateral epidural hematoma. Two emergency craniotomies were performed simultaneously, with satisfactory radiological control and neurological outcome. We discussed the aspects of a etiology and treatment about this unusual condition.
Cranial epidural haematoma, Traumatic brain injury, Computed tomography
Case Report
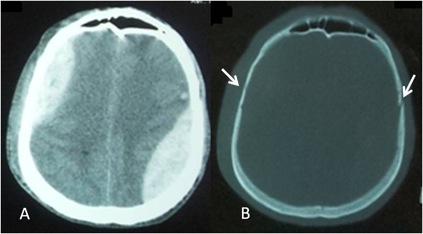
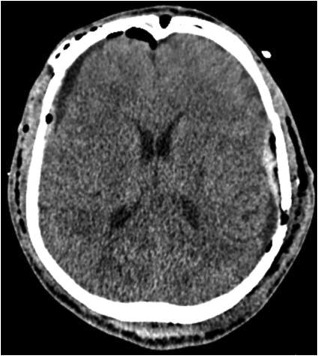
An unknown middle aged man was found unconscious and was brought to our service. On the admission, the patient was comatose and his Glasgow Coma Scale was 8/15. Both the pupils were isochoric and reactive to light with left periorbital edema and a report of seizure. ATLS (Advanced Trauma Life Support) primary survey did not reveal any other abnormality. A Computed Tomography (CT) was taken which showed asymmetric Bilateral Epidural Hematoma (BEH) that measuring 127cm3 at left and 57cm3 at right, with a total volume of 184cm3, and bilateral overlying skull fracture [Table/Fig-1]. He underwent emergency surgery for removal of the Epidural Haematomas (EDH). Both the focal lesions had immediate surgical indication and the drainage was performed simultaneously. The head was placed in Mayfield tongs in neutral position; this cranial fixation system was placed in the midline of the skull, with the tongs fixation slightly diverted to avoid holes on the sagittal sinus.Tongs application on the skull fractures was avoid. Incisions were made at the same time. The craniotomies were also performed simultaneously. Once completed trepanation on one side, already was performed and the other side, quickly performed the two large craniotomies without complications, with satisfactory CT control [Table/Fig-2]. The patient had a prolonged hospitalization due to clinical complications and the need for inpatient rehabilitation and was discharged after one month. During follow-up he presented with Glasgow Outcome Scale 4/5 ninety days after the trauma.
In A – Axial Skull CT showing asymmetric BEH. In B – Skull CT with bone window showing fractures (arrows) and underlying hematomas suggesting arterial source.
Postoperative Skull CT demonstrated a good surgical result with hematomas well evacuated.
Discussion
The first BEH case was described by Roy in 1884. Since then, BEH reports have been sporadic with an incidence rangs from 0,5 to 2% of all EDH [1,2]. High mortality rates (42-100%) have been reported in old series of BEH. With the widespread use of CT scan, early diagnosis has changed the surgical results and prognosis with recent series reported a decrease in mortality rates to 15,7% [1].
Linear skull fractures are associated with EDH in 61-95% of cases. In over one-half of all patients, the middle meningeal artery gives rise to the haematoma [3,4]. However, the main cause of bleeding in the BEH is usually venous bleeding [1]. We suppose that our case of BEH was caused by arterial bleeding after the laceration of both right and left middle meningeal arteries as a result of bilateral skull fracture. In general, haematomas secondary to arterial bleeding require more urgent evacuation since it can rapidly lead to intracranial hypertension (ICH). When surgery is indicated, either arterial or venous EDH are treated by craniotomy, with haematoma evacuation, haemostasis and dural retention sutures (along bone edges and centrally).
Once the diagnosis of BEH is made, urgent surgical treatment should be considered, and in cases of asymmetric EDH, the responsible one for the neurological deterioration (when possible to identify) must be removed first. In cases which the hematoma is small, it can be followed with close clinical and tomographic observation or treated by embolization of the middle menigeal artery to prevent additional enlargement of EDH [2,5]. We opted to remove both haematomas in the same procedure due to their large volumes. To this end, we positioned the patient in the dorsal decubitus position. The head was placed in Mayfield tongs by the two surgeons to facilitate surgical access to cranium both sides, so the EDHs could be treated at the same time. We think BEH should be evacuated simultaneously whenever possible in order to relieve more quickly the ICH and prevent an eventual increment of the contra lateral haematoma during removal of the first EDH in a sequential manner.
In the largest series [1,6,7], when BEH has different dimensions, the side with a larger volume should be evacuated first, followed by the contralateral haematoma, and when they have similar volumes should be evacuated first side of the dominant hemisphere. However, simultaneous craniotomy is possible and recommended, allowing the emergency treatment of intracranial hypertension, and functional recovery even in patients operated in critical neurological conditions.
Mortality is significantly higher in unconscious patients with haematomas >150cm3 size [4]. The patient was unconscious with total volume of intracranial hematoma:184cm3, due to ICH. and Required approach provided an effective treatment.
[1]. Görgülü A, Çobanogÿlu S, Armagÿan S, Karabagÿlı H, Tevrüz M, Bilateral epidural hematomaNeurosurgery Rev 2000 23:30-33. [Google Scholar]
[2]. Pereira CU, Silva AD, Silva MA, Haematoma Extradural Bilateral: Consideraçóes sobre quatro casosJ Bras Neurocirurg 1997 8(1):20-22. [Google Scholar]
[3]. Paiva WS, Andrade AF, Mathias Júnior L, Guirado VM, Amorim RL, Magrini NN, Management of supratentorial epidural haematoma in children: report on 49 patientsArq Neuropsiquiatr 2010 68(6):888-92. [Google Scholar]
[4]. Cooper PR, Post-traumatic Intr-acranial Mass Lesions. Cap 13, p. 275-329. In: Cooper PRHead injury 1993 3rd edBaltimoreEd Williams & Wilkins [Google Scholar]
[5]. De Andrade AF, Figueiredo EG, Caldas JG, Intracranial Vascular Lesions Associated with Small Epidural HaematomasNeurosurgery 2008 62(2):416-20. [Google Scholar]
[6]. Dharker SR, Bhargava N, Bilateral epidural haematomaActa Neurochir (Wien) 1991 110:29-32. [Google Scholar]
[7]. Barlow P, Kohi YM, Acute simultaneous bilateral extradural hematomaSurg Neurol 1985 23:411-13. [Google Scholar]