An ideal intravenous induction agent or a combination of induction agents having rapid and smooth onset and recovery with minimal hemodynamic alterations and side-effects is desirable in day care gynecological surgeries [1]. Both Ketamine & Propofol have rapid and smooth onset of action, however cause significantly opposing hemodynamic effects which can be detrimental in patients with high risk, if used as sole induction agents [2,3]. Few investigators have used various combinations of propofol and ketamine with an aim to offset the hemodynamic effects and minimize other adverse effects of both agents [4–6]. We hypothesized to elucidate a hemodynamically stable combination of propofol and ketamine for induction of anesthesia in day care gynecological surgeries.
Patients and Methods
After formal ethical clearance from Hospital Ethics Committee and written informed consent from 180 adult female patients belonging to ASA (physical status) grade I and II, subjects were scheduled to undergo elective gynecological day care surgery, chosen by computer generated random numbers & for the study purpose divided into five Groups of 30 patients each.
Group I Intravenous injection of propofol (2mg/kg) followed by injection of normal saline.
Group II Intravenous injection of ketamine (2mg/kg) followed by injection of normal saline.
Group III Intravenous injection of propofol (2mg/kg) followed by injection of ketamine (1mg/kg).
Group IV Intravenous injection of ketamine (2mg/kg) followed by injection of propofol (1mg/kg).
Group V Intravenous injection of propofol (1mg/kg) and injection of ketamine (1mg/kg).
A thorough pre-anesthetic check-up comprising of a detailed history, general physical examination and systemic examination of all patients was performed prior to surgery. Baseline investigations were obtained. Patients with remarkable medical or psychiatric illness on treatment and history of addiction were excluded categorically from the study.
All patients were kept nil per oral atleast 6 hours prior to the study period. All patients received injection midazolam 2 mg and injection glycopyrolate 0.2 mg intramuscularly as pre-medication one-hour prior to surgery. In the operation theatre, monitoring in the form of non invasive blood pressure (NIBP), electrocardiogram (ECG) and arterial oxygen saturation (SpO2) were instituted.
Intravenous access was secured under all aseptic conditions after local infiltration with 0.5% lignocaine 0.5 ml. Baseline hemodynamic variables like heart rate (HR), respiratory rate (RR), non invasive systolic (SBP), diastolic (DBP) and mean arterial pressure (MAP) and SpO2 were recorded. Thereafter anesthesia was induced with study drugs by the attending anesthetist in double blind manner.
HR, RR, SpO2 and MAP were observed every minute for five minutes, after administration of study drugs. Patients were also assessed for apnea, which was defined as loss of respiratory effort for 20 seconds or longer. Apnea was treated with 100% oxygen by mask ventilation using Magill’s circuit. Side effects, if any, during the process were also recorded. After the end of study period, anesthesia and analgesia was continued according to standard protocol.
Results
The demographic profile was comparable in all the Groups.
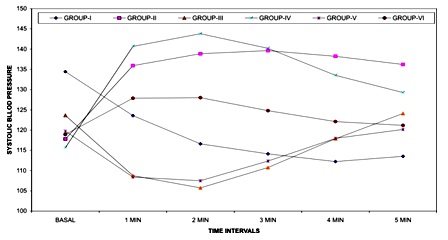
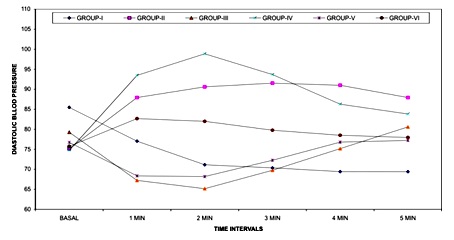
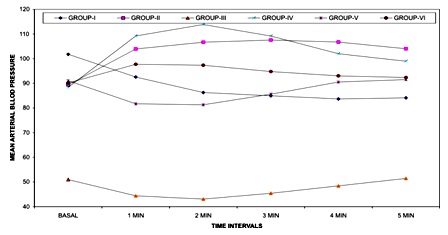
Statistically significant change was observed in systolic blood pressure, diastolic blood pressure and mean arterial blood pressure at fifth minute in Groups I, II and IV (p<0.01). The increase in SBP, DBP and MAP in Groups III and V over the baseline values were statistically non-significant. Inter-Group comparison revealed statistically non-significant changes in arterial pressures between Groups III and V [Table/Fig-1,2and3].
Changes in systolic blood pressurefrom basal in different groups
Changes in diastolic blood pressurefrom basal in different groups
Changes in mean arterial blood pressurefrom basal in different groups
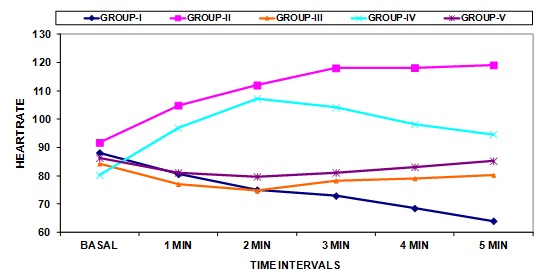
There was rise in heart rate by 29.80% and 5.41% in Group II and IV respectively. InterGroup comparison showed a statistically non-significant change in heart rate in Groups III and V. No statistically significant change in heart rate seen over the baseline values in Group V [Table/Fig-4].
Changes in heart rate from basal in different groups
Maximum incidence (23.33%) of apnea was observed in Group I while in GroupV a lower incidence of apnea was observed (3.33%). No other significant side effects were observed.
Discussion
A stable hemodynamic profile along with negligible adverse effects of induction agents is desirable for day care gynecological surgeries. Ketamine causes sympathetic stimulation leading to increase in myocardial contractility and peripheral vascular resistance, which in turn causes an increased mean arterial pressure and heart rate [7]. Similar effects which were observed in Group II, have been validated by other studies [1,8]. While the use of ketamine may be indicated in cases of hypovolemia, haemorrhage or shock, it has detrimental effects in patients with severe coronary artery disease, hypertension etc. [1].
Propofol induces a larger decrease in arterial pressure after induction of anesthesia, by decreasing peripheral vascular resistance and myocardial contractility [9]. Patients with hypovolemia, cardiac failure and hypertension are occasionally prone to greater decreases in arterial pressure with propofol. Propofol also causes lowering of the heart rate secondary to vagotonic effects [10–12].These hemodynamic effects have been corroborated by observed significant decreases in HR, systolic, diastolic and MAP when propofol 2mg/kg was used.
The combination of propofol 2mg/kg and ketamine 1mg/kg led to a transient fall in SBP, DBP, MAP and HR, owing to the predominant hemodynamic effects of propofol during first two minutes which returned to normal by fifth minute due to opposing hemodynamic effects of ketamine. The results were in accordance with studies which used similar combination of anesthetic agents for induction of anesthesia [4,5,13].
The rise in SBP, DBP, MAP and HR observed when higher dose of ketamine 2mg/kg followed by propofol 1mg/kg was used, due to predominant effects of ketamine on the hemodynamic profile. However stable haemodynamics were achieved when equal dose combinations of propofol and ketamine were used, that is, propofol 1mg/kg and ketamine 1mg/kg [14–16]. Thus the cardiostimulant effects of ketamine were blunted by the cardiodepressant effects of propofol.
No significant difference in respiratory rate and arterial oxygen saturation were observed in our study which is in consistent with studies by other researchers [17,18]. No cardiac dysrrhythmias were encountered throughout the period of our study. The maximum incidence of apnea was observed in Group I.
We understand that an invasive arterial blood pressure(IABP) monitoring is the ideal methods for evaluation of the hemodynamic profile, however we did not monitor IABP due to short nature of surgery which contraindicated placement of IABP. Apart from this a small sample size could be other limitation of our study, which needs to be addressed by future studies.
Conclusion
To conclude, significant hemodynamic changes elucidated when using both propofol and ketamine as sole anesthetic agent or when higher dose of ketamine was used in combination with propofol (i.e. I, II and IV). We achieved optimal hemodynamic stability when equal dose combination of both the drugs were used (propofol 1mg/kg and ketamine 1mg/kg), thereby making it a desirable combination for induction of anesthesia in day care gynecological surgeries.