The birth of a healthy infant at term is dependent upon normal placental development. Disordered placentation is responsible for a wide range of pregnancy complications, ranging from miscarriage through second trimester foetal death and third trimester complications of preeclampsia, foetal growth restriction and abruption placenta [1]. On the other hand, pregnancy complications such as infections, diabetes have influence on the placenta. Detailed evaluation of placenta may throw light on the possible cause of foetal demise or foetal growth restriction.
Methodology
A prospective study was conducted with the permission of institutional ethics committee. Women who had foetal demise [Intrauterine death (IUD)] beyond 24 weeks of gestation and women who had delivered growth restricted foetuses (FGR) were included in the study after taking their informed consents. In the included subjects, placentae with membranes and umbilical cords were collected under aseptic precautions during delivery. Gross examination of placentae was done to look for abnormalities. A bit of placental tissue close to the site of cord insertion was collected and sent for bacterial culture studies. Placental weight was obtained by measuring the weight of the placenta with sterile container using electronic weighing machine and deducting the container weight. Placental thickness was measured using a steel tape, by piercing through the placenta, at the centre.
For the bacteriological culture, the amnion from the foetal surface was stripped off the chorion and from that portion, 3–4 bits of 0.5 to 1cm of placenta were taken for culture. They were sent in a sterile container with normal saline to the microbiology laboratory. The whole placenta was placed in container with 10% formalin, completely immersing the placenta and it was sent for a histopathological examination.
Before histopathological examination, the entire placenta was cut into vertical stripes of about 2–5 cm thickness. From the centrally located placental slices, a block of tissue with full thickness was obtained from foetal to maternal surface from the centre. Blocks were also taken from the cords and membranes. Sections were taken from these blocks, one from maternal surface, one from foetal surface, one or two sections from the cord, one or two sections from the membranes.
The placental weights were classified, based on placental weight percentile curves for singleton deliveries [2].
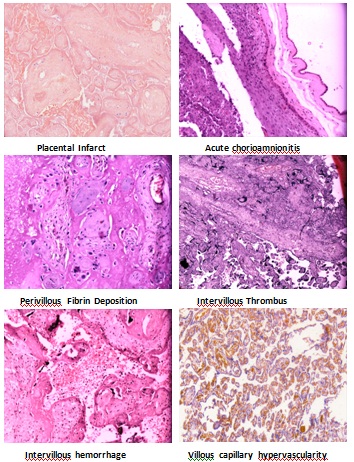
The placental examination findings were classified, as has been shown in [Table/Fig-1, 2,3] [3]. After the histopathological examination, the findings were found to correlate with clinical risk factors, as per [Table/Fig-4, 5] [4].
Gross abnormalities of the placenta, cord & membranes in IUD and FGR
| Gross examination | IUD (n=27) | FGR (n=27) | p–value* |
|---|
| Retroplacental clot | 3 (11.1%) | 2 (7.4%) | 1.0 |
| Infarction | 2 (7.4%) | 1 (3.7%) | 1.0 |
| Calcifications | 6 (22.2%) | 6 (22.2%) | 1.0 |
| Depression | 2 (7.4%) | 1 (3.7%) | 1.0 |
| Accessory lobe | - | 2 (7.4%) | - |
| Circumvallate | 1 (3.7%) | 1 (3.7%) | 1.0 |
| Velamentous cord | - | 1 (3.7%) | - |
| Marginal cord | 1 (3.7%) | 8 (29.6%) | 0.02 |
| True knot | 1 (3.7%) | - | - |
| Varices | 2 (7.4%) | - | - |
| Single umbilical artery | - | 2 (7.4%) | - |
| No abnormality | 15 (55.6%) | 11 (40.7%) | 0.4 |
*There was more than one abnormality in some cases
*Fisher’s exact test
Histopathological abnormalities in IUD and FGR*
| Histopathology | IUD (n=27) | FGR (n=27) | p–value* |
|---|
| Uteroplacental vascular insufficiency | 10 (37%) | 7 (25.9%) | 0.5 |
| Acute inflammation | 7 (25.9%) | 1 (3.7%) | 0.05 |
| Perivillous fibrin deposition | 3 (11.1%) | 1 (3.7%) | 0.6 |
| Intervillous hemorrhage | 1 (3.7%) | 1 (3.7%) | 1.0 |
| Intervillous thrombi | 1 (3.7%) | - | - |
| Villous capillary hypervascularity | 2 (7.4%) | 5 (18.5%) | 0.4 |
| Calcifications | - | 3 (11.1%) | - |
| Villous dysmaturity | 3 (11.1%) | - | - |
| No abnormality | 7 (25.9%) | 9 (33.3%) | 0.7 |
*There was more than one abnormality in some case
*Fisher’s exact test
Histopathology in clinically unexplained cases (IUD and FGR)
| Histopathology in clinically unexplained cases | IUD (n=7) | FGR (n=7) |
|---|
| Uteroplacental vascular insufficiency | 1 | 2 |
| Acute inflammation | 2 | 0 |
| Intervillous thrombi | 1 | 0 |
| Perivillous fibrin deposition with villous capillary hypervascularity | 1 | 2 |
| Villous dysmaturity | 1 | |
| No abnormality | 1 | 3 |
Correlation between clinical risk factors and histopathology in fetal deise
| Clinical risk factors | n=20 | Histopathology | n=20 |
|---|
| Preeclampsia with or without complications | 11 | Uteroplacental vascular insufficiency | 6 * |
| Villous dysmaturity | 1 |
| Perivillous fibrin deposition | 1* |
| No abnormality | 3 |
| Placenta previa | 1 | Acute inflammation | 1 |
| Oligoamnios | 2 | Intervillous hemorrhage | 1 |
| No abnormality | 1 |
| Diabetes | 1 | Villous dysmaturity | 1 |
| Twins | 1 | No abnormality | 1 |
| Cerebral malaria | 1 | Uteroplacental vascular insufficiency with inflammation | 1 |
| HBsAg hepatitis with sepsis | 1 | Perivillous fibrin deposition with acute inflammation | 1 |
| Pyrexia of unknown origin | 1 | No abnormality | 1 |
| Acute maternal hypotension | 1 | No abnormality | 1 |
*One had additional evidence of acute inflammation, one villous capillary hypervascularity
*had additional evidence of inflammation
Histopathology of abnormal placentae
Observation and Results
A total of 54 pregnant women were recruited for the study; 27 had foetal demise and 27 had foetal growth restriction.
Patient profile
The patient profile, as summarized in [Table/Fig-6], shows that in both the groups (IUD as well as FGR), primigravids were slightly more in number than multigravids. In the IUD group, male foetuses were more in number than female foetuses (70.4% versus 29.6%), though it was not significant. The sex ratio was almost equal in newborns with growth restriction (males 52% and females 48%).
| Profile | IUD (n=27) | FGR (n=27) |
|---|
| Age of mother |
| 20-29 years | 23 (85.2%) | 18 (66.7%) |
| 30-34 years | 3 (11.1%) | 7(25.9%) |
| ≥35 years | 1 (3.7%) | 2 (7.4%) |
| Parity of mother |
| Primi | 16 (59.3%) | 15 (55.6%) |
| Multi | 11 (40.3%) | 12 (44.4%) |
| Sex of the fetus |
| Male | 19 (70.4%) | 14 (51.9%) |
| Female | 8 (29.6%) | 13 (48.1%) |
| Clinical risk factors |
| Preeclampsia & complications | 11 (40.7%) | 11 (40.7%) |
| Oligoamnios | 2 (7.4%) | 5 (18.5%) |
| Abruption | - | 1 (3.7%) |
| GDM | 1 (3.7%) | 1 (3.7%) |
| Overt diabetes | - | 1 (3.7%) |
| Placenta previa | 1 (3.7%) | - |
| Acute maternal hypotension | 1 (3.7%) | - |
| Anemia | 1 (3.7%) | 3 (11.1%) |
| Twins | 1 (3.7%) | - |
| Medical illness | 3 (11.1%) | 1 (3.7%) |
| No risk factors | 7 (25.9%) | 7 (25.9%) |
Among the foetal deaths,10 were fresh stillborns, 17 were macerated stillborns. Nearly two third of the foetal demises were seen in small for gestational age foetuses (59.3%).
Preeclampsia and related complications were the most common factors associated with both IUD and FGR (40.7% each). Four out of 54 cases had more than one risk factor, 14 out of 54 (25.9%) cases were without any clinical risk factor.
Observations at placental examination
Majority of the placentae weighed less than 10th percentile in both the groups (61% in IUD and 93% in FGR).Thicknesses of 41.5% (11 out of 27) placentae in IUD group and of 63% (17 out of 27) placentae in FGR group were less than 2 cm. The gross abnormalities seen in placentae are shown in [Table/Fig-2]. It was noticeable that significant number of women of FGR group had marginal insertion of cord.
The histopathological findings among the women with IUD and FGR are as shown in [Table/Fig-3], [5]. Abnormal histopathological findings in placentae were noted in 20 (74%) women who showed foetal demise and in 18(66.7%) who showed foetal growth restriction. Uteroplacental insufficiency and acute inflammation were the leading identifiable abnormalities in IUD group; the former was found significantly in FGR group as well.
In the group with foetal demise, 22 (81%) had placental abnormalities (either gross pathology or histopathology or both), 5 (19%) had no abnormalities. In FGR group also, 22 (81%) had abnormalities (either gross pathology or histopathology or both), 5 (19%) had no abnormalities. Forty seven placentae were subjected to bacteriological culture studies. Placental cultures could not be collected in 4 IUD and 3 FGR cases. Among 17 cases with bacteriological growth on placental cultures, 2(11.8%) showed histopathological evidence of inflammation. Among 6 cases with evidence of inflammation on histopathology, 2 (33.3%) showed bacteriological growth on placental cultures.
Among the clinically unexplained IUD and FGR (7 in each group) cases, placental pathology was present in 6 (86%) and 4 (57%) women respectively [Table/Fig-4].
Correlation between clinical factors and placental pathology
In IUD group, 20 cases had clinical risk factors, among which histopathology was found to correlate in 12 (60%); in 2 (10%) cases, other abnormal histopathologies were found; in 6 (30%) cases, no abnormality was found. Among the 12 cases where histopathology correlated with clinical diagnosis, 5 (41.6%) had additional abnormal histopathologies [Table/Fig-5].
In FGR group, 20 cases had clinical risk factors, among which histopathology correlated in 8 (40%) cases, other abnormal histopathologies were found in 6 (30%) cases and no abnormality was found in 6 (30%) cases [Table/Fig-7].
Correlation between clinical risk factors and histopathology in FGR
| Clinical risk factors | n=20 | Histopathology | n=20 |
|---|
| Pre eclampsia | 10 | Uteroplacentalvascularinsufficiency | 2 |
| Acute inflammation | 1 |
| Perivillousfibrindeposition | 1 |
| Villous capillary hypervascularity | 2 |
| Calcifications | 1 |
| No abnormality | 3 |
| Oligoamnios | 5 | Uteroplacental vascular insufficiency | 1 |
| Villous capillary hypervascularity | 1 |
| Calcifications | 1 |
| No abnormality | 2 |
| Overt diabetes with preeclampsia | 1 | Uteroplacental vascular insufficiency | 1 |
| Abruption | 1 | Intervillous hemorrhage | 1 |
| Anemia | 3 | Uteroplacental vascular insufficiency | 1 |
| Calcifications | 1 |
| No abnormality | 1 |
In FGR, 20 cases were with clinical risk factors, out of which histopathology was correlating in 8 (40%), other abnormal histopathology was found in 6 (30%), no abnormality in 6 (30%)
Discussion
The cause of IUD or FGR can be maternal, foetal or placental. Though most of the times, some risk factor or cause for IUD or FGR can be identified, in some, the cause remains obscure. Several researchers have attempted to identify the risk factors/ causes clinically and/ or by studying the placenta. Korteweg et al., included placental histopathology in the classification system for the causes of perinatal deaths [5].
In the present study, we noted the identifiable clinical risk factors for the IUD and FGR groups; we extended our search by looking into placental pathology in each of such cases.
In this study, placental histopathology correlated with clinical risk factors in 60% women of IUD group and in 40% women of FGR group; 10% women of IUD group and 30% women of FGR group showed other histopathologies which did not correlate. Possibly, these additional histopathological abnormalities would have compounded with clinical risk factors and may have resulted in IUD/FGR.
Among the women with no identifiable clinical risk factors, placental histopathology was abnormal in 86% women of IUD group and 57% women of FGR group; here, studying placental pathology was useful in evaluation of unexplained stillbirth and foetal growth restriction, for determining the cause. Placental study revealed uteroplacental vascular insufficiency in one case of unexplained IUD and in two women with unexplained FGR. Two of the unexplained IUDs were found to be caused by acute infections. Intervillous thrombi, perivillous fibrin deposition and villous dysmaturity were the other findings.
Long et al., showed that prevalence of perinatal deaths was significantly higher in pregnancies with early onset preeclampsia and foetal growth restriction [6]. It is an unfortunate fact that FGR may go unnoticed by the conventional methods. In our study, preeclampsia and related complications (40.7%) and foetal growth restriction(59%) were found to be the most common risk factors for IUD. The features suggestive of uteroplacental insufficiency, observed in preeclampsia and FGR, were present in 37% of IUD cases. William Rayburn et al., observed 25.8% incidence of features of uteroplacental insufficiency in stillbirths [7].
Several authors who studied placentae for placental infections found that chorioamnionitis was more common and also more severe among unexplained stillbirths [8,9]. However, Rayburn et al., despite finding marked placental inflammation, could not demonstrate bacteria in the intraplacental exudates. As was seen in several previous studies, Tolockiene et al., too found chorioamnionitis in 82% stillbirths; but they however, found bacteria only in 50% of them [10]. Interestingly, they also found chorioamnionitis in 68% normal term pregnancies, among which 37% showed positive bacteriological findings and the authors explained this as a cause of or a change- related- to- labour onset. In our study too, there was no correlation between histopathological findings of placental infection and bacteriological studies. Besides, the difficulties in collection and avoiding contamination of the sample are a big challenge. Probably, the two cases where both histopathological findings and microbiological studies were correlated to foetal demise can be attributed to infection.
Histopathological evaluation of placentae and interpretation of the findings demands lot of experience and expertise. Quite a few technical problems are faced during preservation of placentae before undertaking histopathological studies. Due to inadequate preservation, the true findings may be masked. The histopathological findings may be confusing, especially when two or more pathologies are compounded. For example, a case of preeclampsia may be compounded with PPROM and chorioamnionitis; here, there may be overlapping findings of uteroplacental insufficiency as well as acute inflammation. Besides the interpretation of the findings and their correlation with clinical findings are all the more difficult, because one particular histopathologcal finding may be found in several clinical situations. For example, the various features suggestive of uteroplacental insufficiency, such as increased syncitial knots, infarct, villous fibrosis, hypovascularity, may be found in preeclampsia, chronic hypertension, diabetes mellitus and SLE. Stallmach et al., showed that findings of placental maturation defects which can cause foetal hypoxia and stillbirth, may be associated with hypertension, diabetes mellitus, foetal anomalies and maternal fetal rhesus incompatibility [11].
Placenta, being a large tissue where different areas may show different pictures on histopathology, depending on the changes within, the section studied may not be the representative section and the diagnosis may be missed or correlation may be difficult. The elaborate work, time and expertise required to study the placenta and to correlate with the clinical scenario makes the job go undesired. Despite all the odds, it appears from the study, that at least in cases of unexplained foetal demise, it is worth looking for the cause by studying the placenta.
Conclusion
The pathological examination of placenta is complex and it may not be of much use in presence of known clinical cause. However, in cases with unexplained foetal demise and foetal growth restriction, the histopathological findings may be of use for explaining the cause. Knowing the pathological cause will help in understanding the intricacies of foetoplacental unit. However, it is extremely important to take utmost care, to avoid contamination during collection, transport and processing of placentae and also to prevent the changes in the placentae before they are sectioned and slides are prepared.
*There was more than one abnormality in some cases
*Fisher’s exact test
*There was more than one abnormality in some case
*Fisher’s exact test
*One had additional evidence of acute inflammation, one villous capillary hypervascularity
*had additional evidence of inflammation