Huge Bilateral Paramesonephric Cysts in a 25 year old Nulliparous woman
Haritha Sagili1, Manikandan Krishnan2, Papa Dasari3
1 Assistant Professor, Department of Obstetrics and Gynaecology, Jipmer,Pondicherry, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, Jipmer,Pondicherry, India.
3 Professor, Department of Obstetrics and Gynaecology, Jipmer, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Haritha Sagili, Assistant Professor, Department of Obstetrics and Gynaecology, 12,1st Cross, Saradambalnagar Pondicherry-605005, India.
Phone: 9489390630,
E-mail: harithasagili@gmail.com
Paraovarian cysts are uncommon adnexal masses which are usually asymptomatic. We describe a case of bilateral huge paramesonephric cysts in a nulliparous woman. A 25-year-old lady presented with abdominal distension for one year duration. Examination and imaging revealed large abdominopelvic cystic masses with no solid areas or septations. Intraoperatively there were huge bilateral paraovarian cysts which were excised. Histopathology revealed low cuboidal to ciliated columnar epithelium with no evidence of ovarian parenchyma suggestive of paramesonephric cyst. Paraovarian cyst should be included in the differential diagnosis of a cystic mass visualised on ultrasound.
Paraovarian cysts, Paramesonephric cyst
Case Report
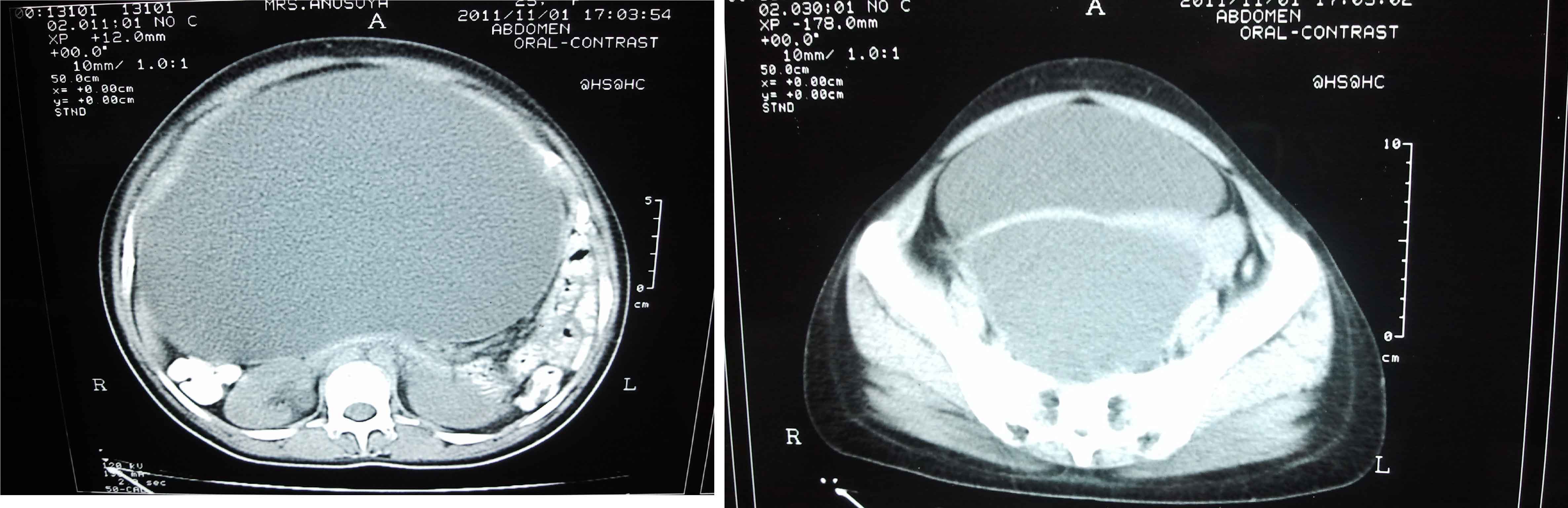
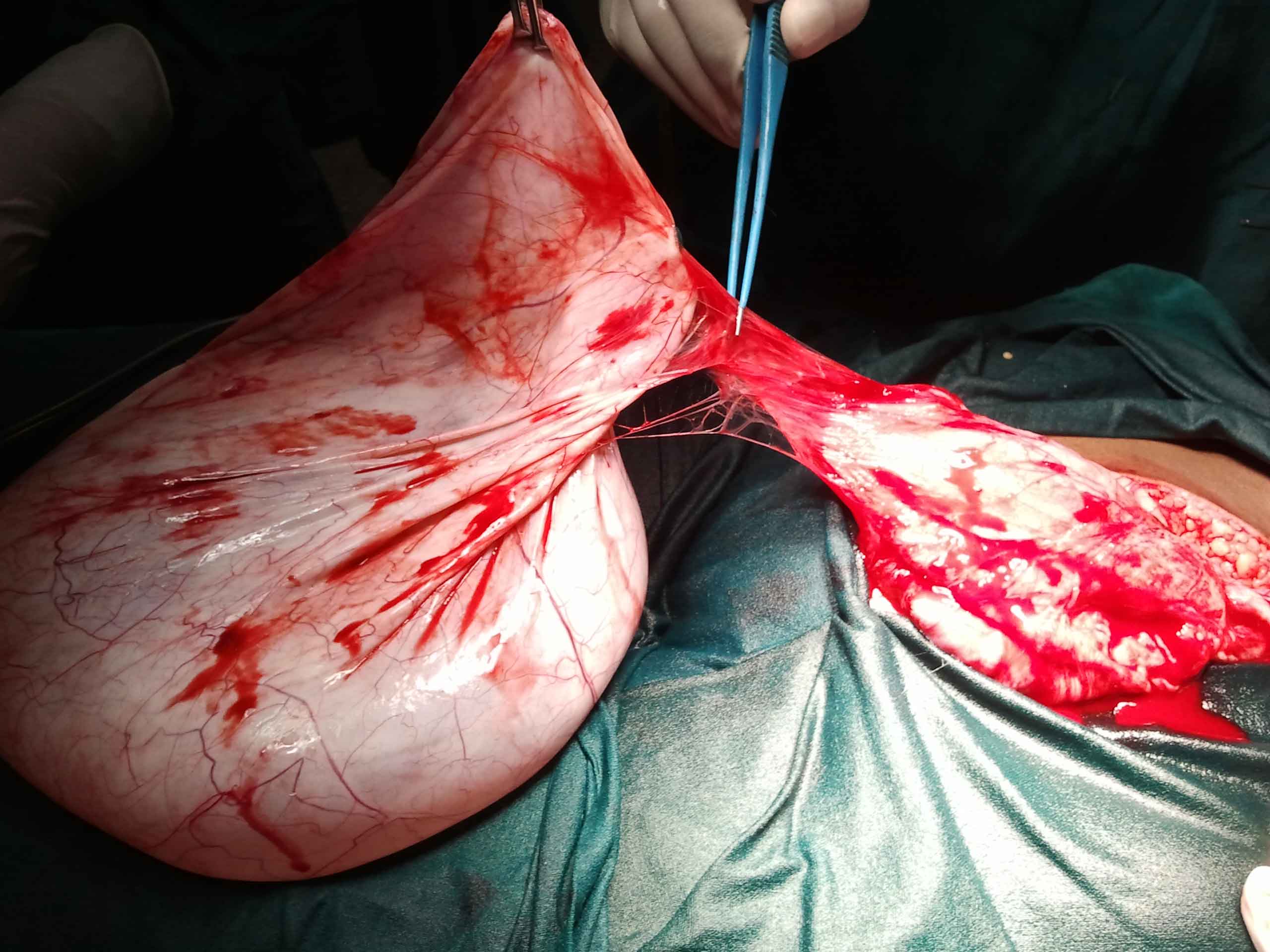
A 25-year-old nulligravida, married for 2 years presented with abdominal distension and weight loss for one year duration. She gave occasional history of pain abdomen. Her menstrual cycles were normal. No other significant past or family history. On examination the abdomen was distended up to the xiphisternum. On bimanual pelvic examination, the uterus was not felt separately and a cystic mass was felt through the posterior fornix. Tumour markers-hCG,PLAP,CA125 and αFP were normal were normal. Ultrasound and a subsequent CT scan [Table/Fig-1] revealed bilateral large abdominopelvic cystic masses with no solid areas or septations. Ovaries were not visualised separately. There was no ascites and lymphadenopathy, and other abdominal viscera were normal. The provisional diagnosis was bilateral ovarian cysts and staging laparotomy was planned. Intraoperatively there were bilateral paraovarian cysts, the left measuring 40 × 40 cm [Table/Fig-2] and the right measuring 30 × 30 cm. Both the fallopian tubes were stretched over the cysts and were separated intact. Uterus and both ovaries were normal. Bilateral paraovarian cystectomy was done. Histopathology revealed low cuboidal to ciliated columnar epithelium with no evidence of ovarian parenchyma, suggestive of paramesonephric cyst. Her post-operative period was uneventful. She was discharged home on the 7th day.
CT scan images showing bilateral cysts probably ovarian in origin
Excision of a huge left paraovarian cyst measuring 40 × 40 cm
Discussion
Parovarian cysts are responsible for about 10% of all adnexal masses. They arise from the tissues of the broad ligament, predominantly from mesothelium covering the peritoneum but also from paramesonephric and mesonephric remnants.
The majority have been reported in young women and rarely are they large enough to be clinically significant [1]. Most patients are without symptoms. When large, they become symptomatic due to pressure effect, lower abdominal pain, abdominal distension and menstrual irregularities. It is difficult to distinguish an ovarian mass from one arising in the parovarium. Complications include torsion, haemorrhage and neoplasm within the cyst. Clinically, torsion of a paraovarian cyst is uncommon, and it is difficult to distinguish it from torsion of other adnexal masses, an ovarian accident, appendicitis, etc. [2]. Papillary serous Cystadenoma, borderline tumour and endometrial sarcoma arising in paraovarian cysts have been reported [3–5].
Paraovarian cysts can show a wide range of sonographic features [6]. Sonographically they are usually thin-walled, smoothly marginated, unilocular cysts. Their risk of malignancy is low if no papillary projections are detected at transvaginal sonography, but when mural proliferations are present, a borderline tumor can be found at pathological examination. MRI might be useful in making a preoperative diagnosis [7]. On microscopic examination a basement membrane may be demonstrated beneath the mesonephric epithelium, although such a layer is usually absent in the mullerian structures.
Pre-operative diagnosis of paraovarian cyst is difficult and it should be included in the differential diagnosis along with large physiologic ovarian cysts and unilocular ovarian cystadenoma when cystic mass is visualised on ultrasound.
[1]. Rijal P, Pokharel H, Chhetri S, Pradhan T, Agrawal A, Bilateral huge fimbrial cysts with torsion of right fallopian tubeHealth Renaissance 2012 Vol 10:No-2.:153-154. [Google Scholar]
[2]. Hasuo Y, Higashijima T, Mitamura T, Torsion of parovarian cyst—report of two casesKurume 1991 38(1):39-43. [Google Scholar]
[3]. Honoré LH, O’Hara KE, Serous papillary neoplasms arising in paramesonephric parovarian cysts. A report of eight casesActa Obstet Gynecol Scand 1980 59(6):525-8. [Google Scholar]
[4]. Puig F, Crespo R, Marquina I, Serous cystadenoma of borderline malignancy arising in a parovarian paramesonephric cystEur J Gynaecol Oncol 2006 27(4):417-8. [Google Scholar]
[5]. Persaud V, Anderson MF, Endometrial stromal sarcoma of the broad ligament arising in an area of endometriosis in a paramesonephric cyst. Case reportBr J Obstet Gynaecol 1977 Feb 84(2):149-52. [Google Scholar]
[6]. Athey PA, Cooper NB, Sonographic features of parovarian cystsAJR Am J Roentgenol 1985 Jan 144(1):83-6. [Google Scholar]
[7]. Kishimoto K, Ito K, Awaya H, Paraovarian cyst: MR imaging featuresAbdom Imaging 2002 27:685.9 [Google Scholar]