Spectrum of Perforation Peritonitis
Sujit M. Chakma1, Rahul L. Singh2, Mahadev V. Parmekar2, K.H. Gojen Singh2, Buru Kapa2, K.H. Sharatchandra2, Amenla T. Longkumer2, Santhosh Rudrappa2
1 Final year PGT, Surgery, Regional Institute of Medical Sciences (RIMS), Imphal, India.
2 Final year PGT, Surgery, Regional Institute of Medical Sciences (RIMS), Imphal, India.
3 Final year PGT, Surgery, Regional Institute of Medical Sciences (RIMS), Imphal, India.
4 Senior Registrar, Surgery, Regional Institute of Medical Sciences (RIMS), Imphal, India.
5 Second year PGT, Surgery, Regional Institute of Medical Sciences (RIMS), Imphal, India.
6 Professor, Surgery, Regional Institute of Medical Sciences (RIMS), Imphal, India.
7 Second year PGT, Medicine, NRS Medical College, Kolkata, India.
8 Final year PGT, Surgery, Regional Institute of Medical Sciences (RIMS), Imphal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sujit M Chakma, Boula Passa, Opposite Town Hall, Kailashahar, Tripura - 799277, India.
Phone: 8794913346,
E-mail: superdocsujit@gmail.com
Introduction: Perforation peritonitis mostly results from the perforation of a diseased viscus. Other causes of perforation include abdominal trauma, ingestion of sharp foreign body and iatrogenic perforation. The diagnosis is mainly based on clinical grounds. Plain abdominal X-rays (erect) may reveal dilated and oedematous intestines with pneumoperitoneum. Ultrasound and CT scan may diagnose up to 72% and 82% of perforation respectively. The present study was carried out to study various etiological factors, modes of clinical presentation, morbidity and mortality patterns of perforation peritonitis presented in the RIMS hospital, Imphal, India.
Material and Methods: The study was conducted from September 2010 to August 2012 on 490 cases of perforation peritonitis admitted and treated in the Department of Surgery. Initial diagnosis was made on the basis of detailed history, clinical examination and presence of pneumoperitoneum on erect abdominal X-ray.
Results: A total of 490 patients of perforation peritonitis were included in the study, with mean age of 48.28 years. 54.29% patients were below 50 years and 45.71% patients were above 50 years. There were 54.29% male patients and 45.71% female patients. Only 30% patients presented within 24 hours of onset of symptoms, 31.43% patients presented between 24 to 72 hours and 38.57% patients presented 72 hours after the onset of symptoms. Mean duration of presentation was 54.7 hours. Overall 469 patients were treated surgically and 21 patients were managed conservatively. Overall morbidity and mortality recorded in this study were 52.24% and 10% respectively.
Perforation, Peritonitis, Presentation, Etiology, Morbidity, Mortality
Introduction
Perforation peritonitis is one of the commonest surgical emergencies in our country as well as in the RIMS hospital. Despite advancements in surgical techniques, anti–microbial therapy and intensive care, management of peritonitis continues to be highly demanding, difficult and complex [1, 2].
Peritonitis usually presents as an acute abdomen. Local findings include abdominal tenderness, guarding or rigidity, distension, diminished bowel sounds. Systemic findings include fever, chills or rigor, tachycardia, sweating, tachypnea, restlessness, dehydration, oliguria, disorientation and ultimately shock [3].
The diagnosis is based mainly on clinical grounds. Plain Xray, ultrasound and CT scan are the tools that can ascertain the diagnosis. However diagnostic laparoscopy can be helpful in some cases.The study has been carried out to evaluate various etiological factors, modes of clinical presentation, morbidity and mortality pattern of different types of perforation peritonitis presented in RIMS Hospital.
Material and Methods
The study was conducted from September 2010 to August 2012. A total of 490 cases of perforation peritonitis were treated in the Department of Surgery, RIMS hospital Imphal, India were included in the study. The cases due to anastomotic dehiscence or those patients who were not willing to participate have been excluded. In all patients of suspected perforation peritonitis, resuscitation was given first and initial diagnosis was made on the basis of detailed history, physical finding and presence of pneumoperitoneum on erect abdominal X-ray. Emergency investigations were done that included Hb%, serum urea and electrolytes, random blood sugar and urine albumin and sugar. Ultrasound of abdomen was done in selected patients. In all cases nasogastric tube was put for gastric aspiration. Urinary catheterization was done for monitoring urine output. After proper hydration, all the patients who were fit for anaesthesia underwent emergency exploratory laparotomy. Control and repair source of contamination, generous irrigation of peritoneum and drain insertion was done during surgery. Abdomen was closed with continuous non–absorbable suture. The patients who were not fit for surgery were managed conservatively and ultrasound guided vacuum suction drain inserted when possible.
Results
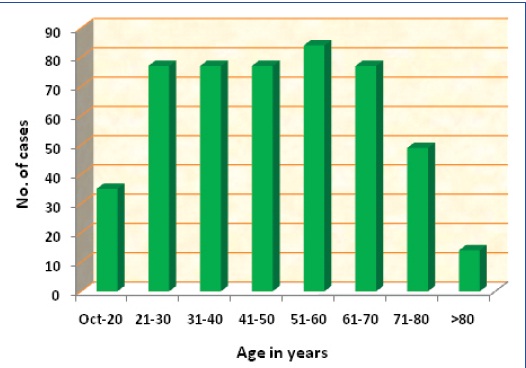
The male to female ratio was 1.18: 1. Majority of patients presented late to the hospital after the onset of symptoms. Only 147(30%) patients were presented within 24 hours of onset of symptoms, 154 (31.43%) patients presented between 24 to 72 hours and 189 (38.57%) patients presented 72 hours after the onset of symptoms. Highest number (17.15%) of patients belongs to the age group of 51 to 60 years [Table/Fig-1].
Abdominal tenderness was the commonest clinical finding and was present in all patients. Abdominal guarding was present in 97.14% patients followed by diminished or absent bowel sound (57.14%), shock (54.29%). tachycardia (54.28%), dehydration (52.85%) and obliteration of liver dullness (48.57%) [Table/Fig-2].
| Types of perforation | No. of cases | Percentage (%) |
|---|
| Duodenal ulcer | 266 | 54.29 |
| Typhoid ulcer | 105 | 21.43 |
| Appendicular | 55 | 11.22 |
| Traumatic | 42 | 8.57 |
| Gastric ulcer | 14 | 2.86 |
| Tubercular | 7 | 1.43 |
| Idiopathic | 1 | 0.2 |
| Total | 490 | 100 |
Total 469 patients were treated surgically and 21 patients were managed conservatively as these patients were not fit for anaesthesia. Graham’s omental patch repair was done in 56.72% of the cases, primary closure 31.34%, appendicectomy 11.65%. A proximal colostomy was added in 8 cases of primary closure of colon.
Overall morbidity and mortality recorded in this study were 52.24% and 10% respectively. Morbidity and mortality was higher among those who presented late to the hospital and those who were in advanced age group with associated co-morbidities [Table/Fig-3].
Complications of perforation
| LOCAL | Name of complications | No. of cases | (%) |
|---|
| Wound infection | 175 | 37.31 |
| Paralytic ileus | 56 | 12.43 |
| Abdominal dehiscence | 7 | 1.49 |
| Intra-abdominal abscess | 24 | 5.97 |
| Fecal fistula | 0 | 0 |
| Intestinal obstruction | 0 | 0 |
| SYSTEMIC | Respiratory | 84 | 17.91 |
| Renal | 35 | 7.46 |
| Cardiovascular | 14 | 2.98 |
| MOSF | 14 | 2.98 |
| Septicemia | 21 | 4.48 |
Discussion
Mean age was 48.28 years in the study and it ranged from 36.8 to 60 years in various studies [4–7]. It was almost equivalent to the mean age of 49 years found by Singh G et al., [7] The incidence of perforation was slightly higher in female population as compared to other studies [4,5,8]. In majority of the cases, the presentation to the hospital was late with well established generalized peritonitis with purulent/faecal contamination and varying degrees of septicaemia.
The perforations of proximal gastro–intestinal tract were approximately 7 times as common as distal tract which is in sharp contrast to developed countries where distal perforations are more common [9]. Duodenal ulcer perforation was the most common (54.29%) and same result was shown by other studies [4,6]. Gastric ulcer perforation accounted for 2.86% of all cases and the incidence was slightly higher than shown by Afridi SP et al., in their study [5]. Peptic ulcer perforation was noticed in increased frequency among the older age group in this study and same was noticed by Strang C et el.,[10] Peptic ulcer perforation was more common in males than in females with male to female ratio of 2.6:1. But the incidence of peptic perforation in females was higher in comparison to the study by Kozoll DD et al., and DeBakey M [11].
In various studies, it has been observed that there is an association between peptic perforation and use of NSAIDS, steroids and alcohol ingestion [4,12,13]. In this study 36.84% of patients of duodenal ulcer perforation had positive history of NSAID ingestion, 2.63% had history of steroid and 18.42% had history of alcohol consumption. Seven patients of gastric ulcer perforation had history of alcohol consumption. Mortality rate of peptic ulcer perforation in this study was 7.5% and it varies from 4-11% in other studies.[6,14,15]. Twenty one patients of peptic ulcer perforation were died and 14 of them were treated conservatively as they were not fit for surgery due to moribund condition and associated co-morbidities. Seven patients died due to MOSF and 7 died due to renal failure with respiratory complications. Seven patients died post–operatively due to septicaemia.
Primary closure was done in all cases of typhoid ileal perforation and mortality rate was 6.67%. Reported mortality of other studies ranges from 7.9% to 31% [16,17].
Appendicular perforations were seen in 55(11.22%) patients comparable to other studies that showed an incidence of 5% to 13.7% [4,5]. Seven patients died post–operatively due to late presentation, faecal peritonitis and sepsis. There were 34 male and 21 female patients, age ranged from 27 to 70 years with mean age 44 years. Appendectomy, peritoneal toileting and systemic antibiotics were used in all cases.
Traumatic perforations accounted for 8.57% of all causes and it is comparable with the 9% incidence shown by Jhobta RS et al., [4]. Road traffic accidents were major cause (50%) of traumatic perforations in this study and Mukhopadhyay M found 55.31% of traumatic perforations were due to road traffic accidents [18], 33.33% patients with traumatic perforation died post–operatively.
Rare causes of perforation were tuberculosis and idiopathic perforation. Only 7 cases (1.43%) of ileal perforation due to tuberculosis were found. Various studies showed tuberculosis as one of the least common cause of perforation and incidence ranged from 4% to 21%.[4,5,8,19,20] Idiopathic perforation of colon is a rare condition. Only 1 case was found in this study. Age of the patient was 61 years and mean age of idiopathic colon perforation is 60 years reported by Yang B et al., [21].
The higher incidence of wound infection may be because majority (38.51%) of patients presented late (>72hours) to the hospital with well–established peritonitis and majority were older group. Moreover 91(19.40%) patients had pre-operative co-morbidities and morbidity was higher among them. Overall morbidity of 50.24% was comparable with the study by Jhobta RS et al., [4].
Overall mortality in this study was 10% and similar mortality were reported by various studies varying from 6% to 38% [4,5,22].
Conclusion
The majority of perforation peritonitis cases in the study comprised of peptic ulcer perforations followed by typhoid ileal, appendicular and traumatic perforations. Tuberculous and idiopathic perforations were rare. Overall morbidity and mortality were acceptable. However, with conservative treatment, moribund patients and in cases of extremely delayed presentation, worse outcomes were noted. The basic principles of early diagnosis, prompt resuscitation and urgent surgical intervention still form the cornerstones of management in these cases. It is once again confirmed that the spectrum of peritonitis in our part of the world is markedly different from that of the western world.
[1]. Memon AA, Siddique FG, Abro AH, Agha AH, Lubina Shahazadi, Memon AS, An audit of secondary peritonitis at a tertiary care university hospital of Sindh, PakistanWorld J Emerg Surg 2012 Mar 7:6 [Google Scholar]
[2]. Bosscha K, Van Vroonhoven TJ, Vander WC, Surgical management of severe secondary peritonitisBr J Surg 1999 86:1371-7. [Google Scholar]
[3]. Doherty GM, Current diagnosis and treatment, Surgery 2010 13th editionNew YorkThe McGraw-Hill Companies, Inc.:464-8. [Google Scholar]
[4]. Jhobta RS, Attri AK, Kaushik R, Sharma R, Jhobta A, Spectrum of perforation peritonitis in India - review of 504 consecutive casesWorld J Emerg Surg 2006 1:26 [Google Scholar]
[5]. Afridi SP, Malik F, Rahaman SU, Shamim S, Samo KA, Spectrum of perforation peritonitis in Pakistan: 300 cases of Eastern experiencesWorld J Emerg Surg 2008 3:31 [Google Scholar]
[6]. Patil PV, Kamat MM, Hindalekar MM, Spectrum of perforative peritonitis-a prospective study of 150 casesBombay Hospital J 2012 54(1):38-50. [Google Scholar]
[7]. Singh G, Sharma RK, Gupta R, Gastrointestinal perforations-a prospective study of 342 casesGastroentrol Today 2006 Sept-Oct 10(4):167-70. [Google Scholar]
[8]. Sharma L, Gupta S, Soin AS, Bikora S, Sikora S, Kapoor V, Generalized peritonitis in India-The tropical spectrumSurg Today 1991 May 21(3):272-7. [Google Scholar]
[9]. Nishida T, Fujita N, Megawa T, Nakahara M, Nakao K, Postoperative hyperbilirubinemia after surgery for gastrointestinal perforationSurg Today 2002 32:679-84. [Google Scholar]
[10]. Strang C, Spencer IOB, Factors associated with perforation in peptic ulcerBr Med J 1950 Apr 1(4658):873-6. [Google Scholar]
[11]. Kozoll DD, Meyer KA, Laboratory findings in acute perforated gastroduodenal ulcersArch Surg 1962 Jun 84:646-61. [Google Scholar]
[12]. Gilies M, Skyring A, Gastric and duodenal ulcer, the association between aspirin ingestion, smoking and family history of ulcerMed J Aus 1969 Aug 2(6):280-5. [Google Scholar]
[13]. Dayton MT, Kleckner SC, Brown DK, Peptic ulcer perforation association with steroid useArch Surg 1987 Mar 122(3):376-80. [Google Scholar]
[14]. Boey J, Wong J, Ong GB, A prospective study of operative risk factors in perforated duodenal ulcerAnn Surg 1982 Mar 195(3):265-9. [Google Scholar]
[15]. Rajesh V, Chandra SS, Smile SR, Risk factors predicting operative mortality in perforated peptic ulcer diseaseTrop Gastroenterol 2003 Jul-Sep 24(3):148-50. [Google Scholar]
[16]. Adensunkanni AR, Desunkan MI, Ajao OG, The prognostic factors in typhoid ileal perforation: A prospective study of 50 patientsJ R Coll Surg Edinb 1997 42:395-9. [Google Scholar]
[17]. Mock CN, Amaral J, Visser LE, Improvement in the survival from typhoid ileal perforation: Result of 221 operative casesAnn Surg 1992 Mar 215(3):244-9. [Google Scholar]
[18]. Mukhopadhyay M, Intestinal Injury from Blunt Abdominal Trauma: A Study of 47 CasesOMJ 2009 24:256-9. [Google Scholar]
[19]. Wani RA, Parray FQ, Bhat NA, Wani MA, Bhat TH, Farzana F, Nontraumatic terminal ileal perforationWorld J Emerg Surg 2006 1:7 [Google Scholar]
[20]. Talwar S, Talwar R, Prasad R, Tuberculous perforations of the small intestineIJCP 1999 53:514-8. [Google Scholar]
[21]. Yang B, Ni HK, Diagnosis and treatment of spontaneous colonic perforation: Analysis of 10 casesWorld J Gastroenterol 2008 July 14(28):4569-72. [Google Scholar]
[22]. Gupta SK, Gupta R, Singh G, Gupta S, Perforation peritonitis: A two year experienceJK Science 2010 July-Sept 12(3):141-4. [Google Scholar]